Purpose
To compare intraocular pressure (IOP) measurements after penetrating keratoplasty (PK) using Goldmann applanation tonometry (GAT; Haag-Streit USA), TonoPen XL (Reichert Inc), Pascal Dynamic Contour tonometer (PDCT; Swiss Microtechnology AG), and Ocular Response Analyzer (ORA; Reichert Inc) and to analyze effects and correlation of corneal thickness and curvature on these measurements.
Design
Prospective, cross-sectional study.
Methods
settings: Departments of Ophthalmology, University of Auckland and Auckland District Health Board, New Zealand. study population: Thirty-one eyes of 31 participants with previous PK. observations: IOP measured using GAT, TonoPen, PDCT, and ORA. Central corneal thickness (CCT) and corneal astigmatism were assessed by Pentacam rotating Scheimpflug tomography. main outcome measure: Degree of agreement in IOP measures and correlation with CCT and corneal astigmatism.
Results
Mean age was 44.5 ± 21.0 years and mean time since PK was 27.7 ± 28.2 months (range 3.0–122.4 months). Mean CCT was 585 ± 149 μm and mean corneal astigmatism 5.5 ± 3.8 diopters. There was no significant difference in IOP measured by GAT and TonoPen; however, both PDCT (2.12 mm Hg, P < .01) and ORA (6.29 mm Hg, P < .01) measured significantly higher IOPs compared to GAT. ORA showed the least agreement with GAT. Significant correlation was identified between each pair of measurement techniques. No instruments correlated significantly with CCT. Only PDCT showed no significant correlation with corneal astigmatism. However, no IOP measures correlated with corneal astigmatism if sutures in situ or less than 1 year post-PK.
Conclusions
TonoPen or PDCT are the most suitable alternatives for measuring IOP in PK eyes where GAT readings are difficult to obtain. PDCT also offers the advantage of being independent of both CCT and corneal astigmatism.
The incidence of raised intraocular pressure (IOP) following penetrating keratoplasty (PK) has been reported between 14% and 78%. Not only can prolonged elevation of IOP damage the optic nerve, it can be harmful to the donor endothelium and ultimately affect the success of the corneal graft. IOP monitoring is therefore an essential aspect of patient management following PK.
The Goldmann applanation tonometer (GAT; Haag-Streit USA, Mason, Ohio, USA) is currently the gold standard for IOP measurement and is in widespread use in clinical practice. Goldmann and Schmidt calibrated the tonometer for a mean central corneal thickness (CCT) of 520 μm. The accuracy of this instrument is therefore affected by corneal thickness that deviates from this “normal” value. Furthermore, the relationship between measured IOP in the context of increased CCT related to edema is expected to be different from the relationship between physiological CCT and applanation-measured IOP. Corneal astigmatism is also an important source of error in GAT and previous studies suggest that corneal astigmatism affects the measured IOP by between 0.25 10 and 0.67 mm Hg/diopter. Post-PK corneas commonly exhibit moderate to marked astigmatism, typically have pachymetry greater than 520 μm, and may have a degree of clinical or subclinical edema; therefore, GAT may be inaccurate in post-PK corneas.
A plethora of instruments have been developed for measuring IOP, each claiming specific advantages over GAT. The TonoPen XL (Reichert Inc, Depew, New York, USA) measures over a smaller corneal area (1.5 mm) and so may be an accurate alternative to GAT for measuring IOP in eyes with irregular corneas. The Pascal Dynamic Contour tonometer (PDCT; Swiss Microtechnology AG, Port, Switzerland) uses a nonapplanating technique and is designed to be largely independent of structural properties of the cornea. The Ocular Response Analyzer (ORA; Reichert Inc) provides cornea-compensated IOP (IOPcc) that are adjusted to account for corneal hysteresis.
The aims of this study were 1) to compare IOP measurements in post-PK eyes taken using GAT and 3 contemporary, alternative instruments to measure IOP (TonoPen XL, PDCT, and ORA); and 2) to analyze the effects and correlation of corneal thickness and curvature on the aforementioned measurements.
Methods
A prospective analysis was performed of patients with a penetrating corneal transplant recruited from the Department of Ophthalmology, Greenlane Clinical Centre, Auckland District Health Board. Patients who had previously undergone PK in 1 eye, at least 3 months prior to recruitment, were invited to participate in the study. Exclusion criteria were history of ocular trauma, previous ocular surgery other than corneal transplantation, current contact lens wear, and an episode of corneal transplant rejection within the last 6 months. The 3-month-postoperative time point was selected because any postoperative stromal edema should have resolved, the corneal epithelial architecture restored, and the sutures-in corneal astigmatism typically stabilized by this time.
The order of IOP examination technique was randomized to 1 of 6 combinations, and 1 minute of recovery time was allowed between each examination.
Pentacam rotating Scheimpflug tomography (OCULUS Optikgerate GmbH, Wetzlar, Germany) was performed on the study eye, followed by examination using the ORA. ORA measurements were obtained using automated alignment and release mechanisms, initiated by the examiner, and the IOPcc was recorded.
All eyes were subsequently anesthetized using a drop of 0.4% benoxinate hydrochloride (Chauvin Pharmaceuticals, Ltd, Essex, United Kingdom). IOP was then measured using a slit lamp–mounted GAT with the prisms in the vertical and horizontal meridian and the mean value recorded. Three IOP measurements were obtained using the PDCT and the measurement with the highest Q score was recorded (Q = 1, optimum; Q = 2 or 3, acceptable; Q = 4, questionable; Q = 5 or 6, repetition recommended). IOP was also measured using a TonoPen XL.
Statistical Analysis
SPSS version 15.0 for Windows (SPSS, Chicago, Illinois, USA) was used for statistical analysis. Where data were demonstrated to have a normal distribution, as shown by the 1-sample Kolmogorov-Smirnov test, parametric tests were used. Statistical P values of .05 or less were considered significant.
Results
Thirty-six eyes of 36 participants (17 male and 19 female) were enrolled for this study. Three eyes had a known history of glaucoma and 7 eyes were on topical medication for raised IOP.
GAT was measurable in all 36 patients. For PDCT measurements, Q scores of 3 or less were obtained in 31 of participants (86.1%) and only these cases were used for further analysis. Four of the 5 patients with Q scores above 3 had corneal sutures in place.
The mean age was 44.5 ± 21.0 years (range 19.0–88.3 years). The mean duration since PK was 27.7 ± 28.2 months (range 3.0–122.4 months). Of the 31 patients, corneal sutures had been previously removed in 15 (48.4%), whereas 10 patients (32.2%) had interrupted sutures in place and 6 (19.4%) had a combination of continuous and interrupted sutures.
The mean Pentacam-derived CCT was 585 ± 149 μm and 10 of 31 patients (32.2%) had a CCT of greater than 600 μm. The mean topographic corneal astigmatism was 5.5 ± 3.8 diopters (range 0.3–17.5 diopters).
Table 1 shows the mean and range of IOP measurements obtained using each of the 4 tonometers. There was no statistically significant difference in IOP measured by GAT and TonoPen XL; however, both PDCT and ORA measured significantly higher IOPs compared to GAT.
| Tonometer | Number of Eyes | IOP (Mean ± SD), mm Hg | IOP Range, mm Hg | Mean Difference in IOP Compared to GAT |
|---|---|---|---|---|
| GAT | 31 | 17.83 ± 5.8 | 10–34 | — |
| TonoPen XL | 31 | 17.26 ± 5.6 | 8–31 | 0.57 mm Hg lower ( P = .43) |
| PDCT | 31 | 19.95 ± 7.3 | 12.3–43.5 | 2.12 mm Hg higher ( P < .01) |
| ORA | 31 | 24.12 ± 8.1 | 11.2–50.2 | 6.29 mm Hg higher ( P < .01) |
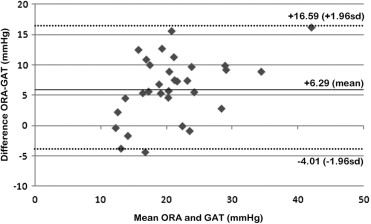
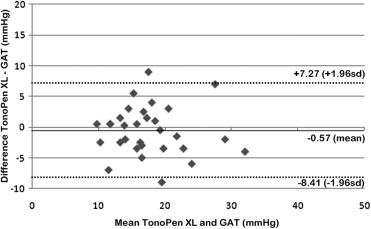
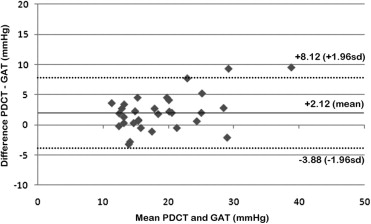
Using Bland-Altman plots for agreement ( Figures 1 through 3 ) , ORA showed the least agreement with GAT and PDCT measurements showed the greatest agreement. PDCT and ORA showed a tendency to overestimate at high IOPs and underestimate at low IOPs compared to GAT.
For the whole group of eyes with PK, and in subgroups based on time since PK ( Table 2 ) and subgroups based on the presence or absence of sutures ( Table 3 ), there was a significant correlation between each pair of measurement techniques. However, none of the 4 instruments’ IOP measurements correlated significantly with CCT.
| Significance (2-Tailed) | |||||
|---|---|---|---|---|---|
| Corneal Astigmatism | GAT | TonoPen XL | PDCT | ORA | |
| CCT | |||||
| All eyes (n = 31) | .189 | .533 | .227 | .250 | .345 |
| Time since surgery under 1 year (n = 12) | .103 | .390 | .435 | .237 | .675 |
| Time since surgery over 1 year (n = 19) | .540 | .542 | .258 | .615 | .285 |
| Corneal astigmatism | |||||
| All eyes (n = 31) | .033 a | <0.01 b | .277 | .031 a | |
| Time since surgery under 1 year (n = 12) | .987 | .410 | .997 | .875 | |
| Time since surgery over 1 year (n = 19) | .010 a | <0.01 b | .106 | .002 b | |
| GAT | |||||
| All eyes (n = 31) | <0.01 b | <0.01 b | <0.01 b | ||
| Time since surgery under 1 year (n = 12) | .005 b | <0.01 b | .002 b | ||
| Time since surgery over 1 year (n = 19) | <0.01 b | <0.01 b | <0.01 b | ||
| TonoPen XL | |||||
| All eyes (n = 31) | <0.01 b | <0.01 b | |||
| Time since surgery under 1 year (n = 12) | .004 b | <0.01 b | |||
| Time since surgery over 1 year (n = 19) | .001 b | <0.01 b | |||
| PDCT | <0.01 b | ||||
| All eyes (n = 31) | |||||
| Time since surgery under 1 year (n = 12) | .002 b | ||||
| Time since surgery over 1 year (n = 19) | .001 b | ||||
a Correlation is significant at the .05 level (2-tailed).
| Significance (2-Tailed) | |||||
|---|---|---|---|---|---|
| Corneal Astigmatism | GAT | TonoPen XL | PDCT | ORA | |
| CCT | |||||
| All eyes (n = 31) | .189 | .533 | .227 | .250 | .345 |
| Sutures absent (n = 15) | .666 | .553 | .250 | .693 | .677 |
| Sutures present (n = 16) | .000 a | .414 | .283 | .233 | .344 |
| Corneal astigmatism | |||||
| All eyes (n = 31) | .033 b | <0.01 a | .277 | .031 b | |
| Sutures absent (n = 15) | .067 | .005 a | .337 | .021 b | |
| Sutures present (n = 16) | .407 | .350 | .221 | .221 | |
| GAT | |||||
| All eyes (n = 31) | <0.01 a | <0.01 a | <0.01 a | ||
| Sutures absent (n = 15) | .001 a | <0.01 a | <0.01 a | ||
| Sutures present (n = 16) | <0.01 a | <0.01 a | <0.01 a | ||
| TonoPen XL | |||||
| All eyes (n = 31) | <0.01 a | <0.01 a | |||
| Sutures absent (n = 15) | .007 a | <0.01 a | |||
| Sutures present (n = 16) | <0.01 a | <0.01 a | |||
| PDCT | |||||
| All eyes (n = 31) | <0.01 a | ||||
| Sutures absent (n = 15) | .001 a | ||||
| Sutures present (n = 16) | <0.01 a | ||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


