39 Cochlear Implants
For over 30 years cochlear implants (Fig. 39.1) have restored auditory sensitivity in hearing impaired patients with advanced sensorineural hearing loss (SNHL). It provides access to speech, environmental sounds, and other informational cues that cannot be captured by other hearing technologies in these patients. As cochlear implant technology has evolved and improved, candidacy criteria has been broadened to include all ages and varying degrees of hearing loss because of increasing observed levels of benefit. In very young children, cochlear implants can eliminate significant delays in developmental learning. As clinical outcomes continue to show improvement in speech recognition, spoken language levels in children, quality of life measures, cochlear implant technology can expand to provide improved hearing in individuals who currently rely on conventional amplification (hearing aids).
In this chapter, we describe detailed practices related to cochlear implant candidacy, techniques of device placement and device programming, clinical outcomes, and training of the auditory system in conjunction with cochlear implant use.
Candidacy
Candidates for cochlear implants include those with significant hearing loss that receive little to no benefit using hearing aids. The amount of benefit received from a cochlear implant can vary depending upon etiology of hearing loss, age at implantation, age of significant hearing loss, hearing history and hearing aid history, motivation, support of oral language development, linguistic abilities, and the presence of other disabilities.
Adult candidates typically have unaided thresholds in the severe to profound hearing loss range but the most important measure of candidacy is speech recognition. Current requirements as per the U.S. Food and Drug Administration (FDA) guidelines include speech recognition on sentence test material (i.e., hearing-in-noise test) typically completed at normal conversational levels (50 or 60 dB sound pressure level) of less than 60% in the better hearing ear and less than 50% in the ear to be implanted with the cochlear implant in the best aided condition.1 Medicare and Medicaid guidelines are more strict than the FDA guidelines and require a score of less than 40% on sentence test material.2
Candidacy in children includes level of hearing impairment as well as lack of progress in auditory skills and language development, family motivation, appropriate expectations, health of the child, and rehabilitative and educational services available. A multidisciplinary approach for evaluation of candidacy in children is essential. Medical, audiological, rehabilitation, educational, and psychological aspects need to be considered when determining candidacy. The multidisciplinary collaboration will help ensure the optimal outcome in hearing, language, social, and educational development for the child receiving cochlear implantation. Appropriate expectations from parents, other relatives, and school personnel are important in as individuals support the child in their development and provide access to follow-up care.
Surgical Techniques
Surgical techniques of cochlear implantation represent modifications of procedures used over the past century in the management of chronic infections of the mastoid and middle ear. Surgery is performed in the conventional otologic position with the use of aseptic precautions, microscopy (up to x160), and a rotating drill.
The mastoid cortex and surrounding temporal skull are exposed by raising a soft tissue “flap,” pedicled anteriorly and inferiorly. Surgeons most commonly use an inverted j-shaped flap (based on posterior-inferior arterial supply) in preference to previously used anteriorly based c-shaped flaps, and inferiorly based u-shaped flaps. The design of the soft tissue flaps should accommodate placement of the implant at safe margins from overlying incisions and in a location compatible with an ear-level processor.
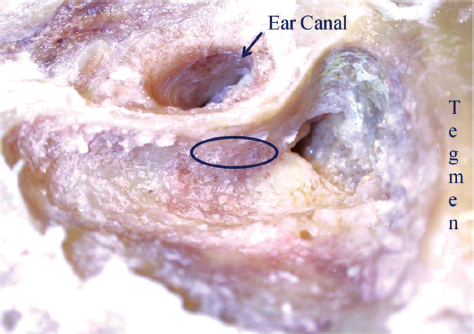
A simple mastoidectomy is performed with the superior (middle fossa tegmen) and posterior (sigmoid sinus) cortical margins maintained intact (Fig. 39.2). The resulting bony ledge provides protection for connecting leads and a bony plateau for embedding the receiver-stimulator. A bony well is drilled and prepared for placement of the receiver-stimulator device. The bony facial recess (between the chorda tympani nerve and vertical segment of the facial nerve) is opened to visualize the incudostapedial joint and cochlear promontory. The facial recess is opened to maximize visualization via thinning of the bony canal wall, and adequate removal of air cells to enable systematic exposure of the horizontal semicircular canal, fossa incudus, and chorda-facial angle.
As the dimensions of the tympanic cavity are established at birth and completed by 6 months of age, the risk associated with the facial recess approach is no greater in children than in adults.3 The chorda tympani nerve may be sacrificed if the facial recess is small or if the array to be implanted requires a generous exposure.4 Permanent taste disturbance, however, is rare. The round window niche is opened exposing its tegmen and the round window membrane.5 When the round window niche is bridged with bone, drilling commences 2 mm below the inferior margin of the oval window.
Figure 39.1 The internal device of a typical cochlear implant consisting of a magnet with a processor. The processor is coupled to an electrode array. In this particular device, a ground lead is incorporated.
Printed with permission from: Cochlear Americas, Centennial, Colorado, United States, 2011.
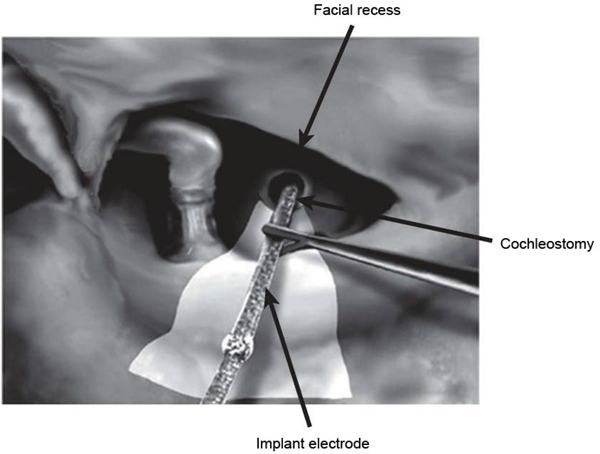
The preferred cochleostomy approach is to access the scala tympani through the promontory, anterior-inferior to the round window. The electrode array is advanced under direct visualization, minimizing trauma to the membranous components of the scala, particularly the basilar membrane (Fig. 39.3). Resistance to array insertion can produce buckling of the carrier array. Buckling can induce spiral ligament and basilar membrane injury, and consequent neural loss. Cochlear trauma with array placement is associated with poorer outcomes in clinical trials of adults6 and children.7 With normal cochlear anatomy, the scala tympani offers an easily accessible, mechanically shielded site for electrode placement that places stimulating electrodes in close proximity to surviving dendrites and cell bodies of auditory nerve afferent fibers.
Figure 39.2 Cadaveric dissection on a left temporal bone. A cortical mastoidectomy has been performed. The black ellipse outlines the facial recess.
Proximity of electrodes to targeted neuronal populations may influence channel selectivity. With closer approximation of electrodes to the modiolar wall, more focused stimulation of spiral ganglion cells may be achieved.6 Enhanced curvature of the carrier of the array is now favored as a strategy to achieve closer positioning. Current electrode carriers are typically inserted over a distance of up to 25 to 30 mm. Insertion along this length of the cochlea places electrodes of the array adjacent to fibers of the auditory nerve that normally subserve the entire range of speech frequencies.8 The aim is to simulate the frequency analysis normally provided by basilar membrane mechanics and the tonotopic pattern of fiber activation within the cochlea.
Obstruction of each of the scalae may occur because of inflammatory changes (associated with meningitis, Cogan syndrome, syphilis, chronic otitis media, and malignant otitis externa), otosclerosis, and trauma.9 Labyrinthitis ossificans results in the formation of fibrous tissue, with the possibility of subsequent dystrophic calcifications deposited in the normally fluid-filled scalae. The scala tympani, especially in the basal turn, is the most common site of fibrous tissue and new bone growth, regardless of the etiology.
As many patients with cochlear ossification receive only partially inserted electrode arrays, performance may suffer either because of smaller numbers of available channels or spiral ganglion cell depletion. However, studies of implant performance with ossified cochleae have shown that general levels of auditory performance are similar to those of patients with patent cochleas.10,11
A significant percentage of children with congenital deafness exhibit cochlear malformation; typically manifested as cochlear hypoplasia or a common cavity.12 Hypoplastic cochleas are associated with poor definition of cochlear turns and partitions between the modiolus and internal auditory canal (IAC) and relatively low spiral ganglion cell populations.13 Implantation of an ear with a severely narrowed IAC is contraindicated in the absence of evidence of peripheral auditory function. Preoperative electrical testing, called promontory stimulus testing may help in determining this.
Figure 39.3 A schematic view of the surgical anatomy during cochlear implantation in a right ear. The facial recess is opened to visualize the round window. The cochleostomy is opened to enter the scala tympani of the cochlea. The electrode array is inserted into the cochleostomy.
Complications
Cochlear implantation entails risks inherent in extended mastoid surgery and those associated with the implanted device. Major complications include facial nerve paralysis and implant exposure because of flap loss. Facial nerve injury is uncommon and, when recognized promptly, is unlikely to produce permanent, complete paralysis. Facial nerve activity is routinely monitored during surgery, which may help decrease the incidence of facial nerve injury. However, otologic surgeons should not solely rely on the facial nerve monitor for locating the facial nerve. Instead, a keen understanding of the anatomic course of facial nerve and its variations is vital in facial nerve preservation. Loss of flap viability can lead to wound infection and device extrusion, necessitating scalp flap revision. When intractable infection is present, device removal is completed with or without replacement.
Device Failure
Revision implant surgery because of device malfunction, infection, electrode migration, facial stimulation, and upgrades from single-channel to multiple-channel cochlear implants occur in approximately 10% of cases.14 Trauma or flaws in manufacturing the internal device may lead to device malfunctions or failures. Device failure commonly produces a sudden loss of sound or intermittent signal, adverse auditory sensations (popping and banging), and nonauditory sensations (pain). Explanted devices are sent to the manufacturer for assessment of electronic and circuit integrity.
Implant Infection and Meningitis
The risk of bacterial infection of an implanted device producing labyrinthitis or meningitis and associated reactive fibrosis and destruction of neural elements appears to be low. However, several studies have shown a higher risk for the meningitis in patients with cochlear implants compared with the general population. Children appear to be particularly affected: of the 52 cases originally reported by the FDA, 33 (63%) were under the age of 7. In the year 2002, an increase in the number of postimplantation meningitis cases was noted. Initial reports suggested a higher risk of meningitis in patients implanted with a positioner, which is a device designed to help the electrodes to hold the modiolus. The increased risk of meningitis eventually led the manufacturer to recall all unimplanted devices using the positioner. The level of risk did not suggest the need for positioner removal unless repeated infections occurred.
Reefhuis et al15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree