Ultrasound investigation of the major salivary glands has been routinely used for the past 25 years. Ultrasound provides an immediate diagnosis in acute or chronic inflammatory salivary diseases and can visualize sialolithiasis as small as 0.4 mm. Ultrasound is also an important imaging modality for salivary gland tumors, guiding fine needle aspiration (FNA) for cytological diagnosis. It is particularly sensitive in detecting suspicious lymph nodes in the neck and helps to guide FNA. Ultrasound is a first-line tool for diagnosis of salivary pathology. It is simple to use, noninvasive, and well tolerated, even in children.
Since the 1980s, ultrasound (US) has been shown to be a highly sensitive means of evaluating the major salivary glands. Because of technological advances and the superficial location of the major salivary glands, most regions are now accessible by high-resolution transducers. Only a small portion of the deep lobe of the parotid gland may be hidden by the acoustic shadow of the mandible. Linear transducers with high frequencies between 7.5 and 16 MHz are used. In large lesions, transducers with a lower frequency may be used to completely visualize the lesion.
Salivary gland US should always be performed on both sides; many lesions occur bilaterally. If a tumor is suspected, the cervical lymph nodes should examined as well. Color Doppler may be useful to investigate inflammatory lesions and tumors. Color Doppler is performed by comparing the vessel density with a normal reference gland or by comparing the vessel density of the tumor with the normal parenchyma. The peak systolic flow is generally measured, but the correction for the angle of the Doppler beam may be difficult to calculate in some cases. In Sjogren’s syndrome, for example, the systolic peak velocity after salivary stimulation (with lemon juice) is often double the peak velocity in the resting state.
Ultrasonographic anatomy
All salivary glands are homogeneous echogenic organs. The normal sizes of the salivary glands have been evaluated. The parotid gland measures on average 46 mm in its vertical dimension and 37 mm in its horizontal dimension, with a thickness of 7 mm anteriorly and 22 mm posteriorly. The submandibular gland measures approximately 33 × 35 × 14 mm. There does not seem to be any gender-related differences, but the size of the glands increase significantly with body weight.
Parotid Gland
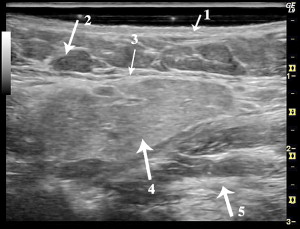
The parotid gland is located in the retromandibular fossa. Anatomically, the superficial lobe and deep lobe are separated by the plane of the facial nerve. On US, the nerve cannot be visualized and thus the anatomic lobes cannot be distinguished. Some refer to the caudal portion of the parotid gland as the superficial lobe, but we prefer referring to structures visualized around or within the gland for orientation, which avoids confusion with the anatomic definition of the parotid lobes. In most cases, the retromandibular vein is visualized without difficulty; however, normal intraglandular salivary ducts and the main duct (Stensen’s duct) are generally not seen, even with high-frequency transducers. A dilated Stensen’s duct may be visualized, running superficially along the masseter muscle through the corpus adiposum buccae and then turning medially through the buccinator muscle. In this anterior region, accessory salivary tissue can often be seen. The echostructure is usually homogeneous and the echogenicity comparable to that of the thyroid gland. Lymph nodes can be seen within the gland, and are located in the anatomic superficial lobe.
On US, the parapharyngeal space is only rarely visualized with sufficient quality. The internal carotid artery, the internal jugular vein and the posterior belly of the digastric muscle are not always seen. Because of acoustic absorption and dispersion, the deep part of the parotid gland is often difficult to visualize ( Fig. 1 ).

Submandibular Gland
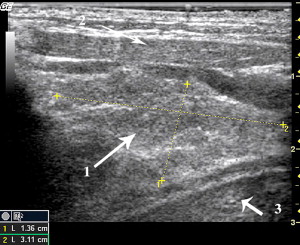
The submandibular gland is located anterior and caudal to the parotid gland. Sometimes the salivary tissues of both glands can be found adjacent to each other without any intervening facia, but their echostructure is different: the submandibular gland is more hypoechoic than the parotid gland. The other anatomic structures in the submandibular region are the mandible, the mylohyoid muscle, the anterior belly of the digastric muscle, and the facial vessels. The facial artery runs posterior to or even within the submandibular gland. On a typical oblique section of the submandibular gland, the palatine tonsil can also be visualized as hypoechoic area in a cranio-posterior position relative to the submandibular gland. Normally, the submandibular glands have a triangular shape with a posterior base. Normal intraglandular ducts are only rarely visualized. After stimulation with lemon, they may be more easily seen. The main submandibular duct (Wharton’s duct) originates from the deep portion of the gland and ascends anteriorly to the caruncula in the floor of the mouth. The main duct can be differentiated from the lingual vessels by color Doppler ( Fig. 2 ).
Sublingual Gland
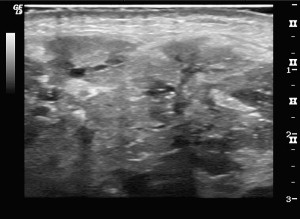
The sublingual glands are localized in the floor of the mouth, cranial to the mylohyoid muscle, medial to the mandible and lateral to the geniohyoid muscle. In some cases the salivary tissue can even extend posteriorly to the submandibular gland. The sublingual glands have multiple small excretory ducts that are not visible with US. The glands appear more echogenic than the hypoechoic muscles of the floor of the mouth ( Fig. 3 ).
Salivary gland infections or sialitis
Infection of a salivary gland is called sialitis , which can be further divided into infection of the gland itself, or sialadenitis , and infection of the salivary duct or ducts, termed sialodochitis . This section will cover the most common infections.
Viral Sialadenitis
Endemic parotitis or the mumps, caused by a paramyxovirus, is the most frequent acute infection, even in the era of systematic vaccination. Usually, the clinical presentation is sufficient for a definitive diagnosis. In 75% of cases both parotid glands are enlarged. Cervical lymph nodes are also always enlarged. On US, the parotid glands are enlarged with a more rounded shape, a convex lateral surface, and a hypoechoic structure. Sometimes the salivary ducts are enlarged and visible. Color Doppler demonstrates diffuse hypervascularization.
Bacterial Sialadenitis
Acute bacterial parotitis
Normally the saliva within the salivary glands is sterile. Bacterial infection can originate in several ways. The most common origin is retrograde infection via the oral cavity, bacteria infecting the gland by way of the salivary duct. Less common origins include extracapsular spread of temporomandibular joint infections and hematogenous septicemia.
Acute bacterial parotitis is as common in adults as in children. Clinical presentation is typically unilateral, with sudden pain and swelling and increased pain at each meal (salivary colic, even in the absence of lithiasis). The examination of the ostium reveals cloudy saliva or pus. Sialadenitis in adults is associated in approximately 50% of cases with sialolithiasis.
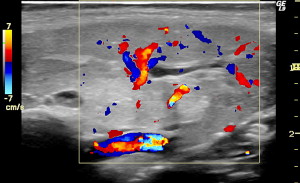
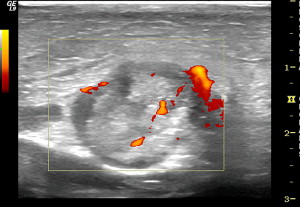
US is the only radiographic examination indicated, revealing salivary duct dilatations, hypoechoic parenchyma, and enlarged intraglandular lymph nodes ( Fig. 4 ). Hypervascularization because of the inflammation is visible on color Doppler ( Fig. 5 ). The main goal of US in inflammatory diseases is to rule out lithiasis or other ductal obstructions. In severe infections, intraglandular liquid spaces, implying abscess formation, may be observed and are more frequent in diabetic patients. Air may also be seen, as well as moving, echoic debris within an abscess. US guidance is particularly useful for needle aspiration or drainage of the abscess ( Fig. 6 ).
Acute bacterial submandibulitis
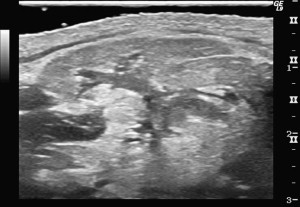
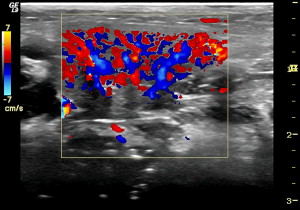
Acute bacterial submandibulitis occurs suddenly, with submandibular pain and swelling. Pus and debris may be seen at the Wharton’s duct ostium in the floor of the mouth. US is essential for diagnosis ( Fig. 7 ). The gland is heterogeneous with dilatation of the salivary ducts and increased vascularization on Doppler ( Fig. 8 ). US is also necessary in this case to rule out an associated lithiasis.
Pediatric chronic bacterial parotitis
Chronic bacterial parotitis in children is a relatively common disease. Occurring at age 2 or 3, more rarely at a younger age, this sialadenitis presents initially like an acute viral infection. Then it evolves unilaterally or bilaterally with episodes of acute pain and swelling and enlarged cervical lymph nodes.
US is indicated as soon as the first symptoms occur. Images are typical and pathognomonic. Multiple hypoechoic, cystoid areas and 2- to 3-mm vacuoles in the parotid glands are caused by the destruction of the glandular tissue by the chronic infection, and can take on a milary aspect on US ( Figs. 9 and 10 ). Focal destruction of the glandular tissue can also cause salivary duct ectasia, which can be visualized on US. Small hyperechoic calcifications, which are not lithiases but a reaction to the inflammation, may also be seen. The Doppler shows hypervascularization of the gland and of the intra- and extraglandular lymph nodes ( Fig. 11 ).

Chronic parotitis in adults
In chronic inflammation, the glandular modifications seen on US are often less prominent than in acute diseases. An atrophic hypoechoic gland may be seen, but the size of the gland is variable. Sometimes ductal ectasia is found ( Fig. 12 ); however, sialography is superior to US for visualizing chronic inflammatory obstructions of the salivary ducts.
Adult chronic parotitis may occur in a patient having suffered from chronic or acute parotitis as a child or with a history of acute parotitis, or in the context of a systemic disease such as Sjogren’s syndrome. It can also be secondary to a stricture or stenosis of a salivary duct, itself secondary to an acute infection.
US shows partial destruction of the gland, which is heterogeneous with hypoechoic regions representing destroyed parenchyma and hyperechoic regions of sclerosis. Dilatation of the salivary ducts with strictures or stenosis is always found, with strictures along Stensen’s canal creating a “string of pearls” image. Ductal ectasia may also be present. Lymph nodes are visible within the gland and in the cervical regions. Doppler may or may not show hypervascularization, according to whether inflammation is present or not.
Tuberculous parotitis
Tuberculosis of the salivary glands is rare, with parotitis mimicking a malignant tumor. Moderate pain, or no pain at all, may be present. On US, there are heterogeneous, hypoechoic, poorly-defined lesions, with regional lymphadenopathy ( Fig. 13 ). The lymph nodes themselves have poorly defined margins as well ( Fig. 14 ). US-guided fine-needle aspiration (FNA) cytology is diagnostic showing specific granulomatous lesions with giant cells and necrosis.
Idiopathic Dilatation of the Salivary Ducts
This problem is attributable to a stricture or stenosis located at the level of the sphincter of the main salivary duct that causes a dehiscence of the wall of the duct. The dilatation resembles a hernia of the main salivary duct, occurring during meals. As the disease progresses, pain can also occur, giving rise to a salivary colic, and bilateralization generally occurs. At this stage, the duct can be seen and palpated under the skin of the cheek. It occurs most often in Stensen’s duct of the parotid gland, primarily in females.
US confirms the diagnosis, showing a major dilatation of the duct with a diameter of up to 1 cm, all along the duct ( Fig. 15 ). The stenosis is generally well visualized, and may be located anywhere along the canal ( Fig. 16 ). No lithiasis is visible ( Figs. 17 and 18 ). The glandular tissue may be hypotrophic with other dilated ducts. Signs of infection are often associated with the disease because of the stagnation of saliva within the gland. Doppler shows hypervascularization along the wall of the duct and also at the level of the stenosis.
Sialodochitis with Sialolithiasis
It is now generally acknowledged that lithiasis formation can be found during early childhood, around the age of 1 year, but even earlier in some cases (our youngest case was a 2-month-old girl). A genetic predisposition has also been shown, with more that 300 families identified. In our experience of 3500 cases of lithiasis over a 20-year period, we have observed that only one type of major salivary gland is involved per patient, uni- or bilaterally; we have never observed lithiasis in different types of glands (parotid and submandibular, for example) in the same patient. Submandibular and parotid lithiases show the same composition, but with different proportions of calcium and phosphate.
More than 80% of salivary concretions are localized in the submandibular gland or in Wharton’s duct. Approximately 15% of cases of sialolithiasis occur in the parotid gland or in Stensen’s duct. Sublingual lithiasis is rare.
Salivary calculi usually cause symptoms only if an obstruction of the ductal system occurs. For therapeutic purposes it is important to differentiate lithiasis of the main duct from those of the intraglandular ducts. Typical locations for lithiasis are at the anterior bend of Wharton’s duct and at the confluence of the intraglandular ducts. Sometimes intraoral transducers are used to localize submandibular stones. Lithiasis of the parotid system is often located in the ducts in the periphery of the gland or deep in the parenchyma.
Sonographically, lithiasis typically appears as a bright curvilinear echo complex with posterior shadowing ( Figs. 19 and 20 ). In lesions smaller than 2 mm, this shadow may be missing ( Fig. 21 ).
In symptomatic sialolithiasis, a concomitant dilatation of the ductal system or inflammation is often visualized ( Fig. 22 ). Intraglandular duct ectasia presents as multiple tubular hypoechoic structures, whereas the dilated main duct is located in an extraglandular position and has a more linear shape. Inflammatory changes render the gland diffusely hypoechoic and with more rounded, globular margins. Color Doppler shows hypervascularization.
The accuracy of US in the assessment of sialolithiasis is approximately 90%. It is possible to differentiate calcified lymph nodes and phleboliths in facial veins from sialolithiasis. Approximately 20% to 40% of the salivary lithiases are not opaque on plain films, but most of these stones are visible on US. Salivary stimulation (lemon or vitamin C) leads to more prominent intraglandular ducts. This facilitates the visualization of small lithiases and the echogenic lithiases contrast better with the dilated hypoechoic ducts.
In experienced hands, US is the primary method for detecting salivary calculi. Computed tomography, MRI, or sialography can be reserved for those patients with inconclusive sonographic results or for patients with negative sonographic results and a typical clinical presentation of ductal obstruction.
Sialosis
The term of sialosis designates all the chronic diseases of the salivary glands that are not infections or tumors. This includes nutritional, dystrophic, and systemic diseases affecting the salivary glands. Most of these diseases are characterized by a hyperplasia of the salivary gland or glands, termed sialomegaly , and with deficit in salivary secretion.
Sialoadenosis
Often diabetes, alcoholism, and anorexia nervosa are clinically evident. US shows enlarged glands with a hyperechoic structure and no focal lesions. Because of the high echogenicity, the deep portions of the parotid glands are usually not visualized ( Fig. 23 ). Sometimes low-frequency transducers have to be applied to delineate the glands completely. Hypervascularization, as often found in acute inflammation, should be ruled out by demonstration of normal or subnormal color Doppler saturations ( Fig. 24 ). In these bilateral painless enlargements of the glands it is important to rule out tumors and ductal obstructions. This can be performed by demonstration of a homogeneous glandular structure.
Systemic Sialosis
Sjogren’s syndrome
Sjogren’s syndrome (SS) is an autoimmune disease with chronic inflammation of the major salivary glands, the lacrimal glands, and arthritis. The exocrine glands are infiltrated by lymphocytes and plasma cells. The incidence of Sjogren’s disease in women is seven to nine times higher than in men. Usually, patients present with a sicca complex. Often the antinuclear antibodies (ANAs) are positive, especially the subsets Anti-Ro/SSA, Anti-La/SSB. Definitive diagnosis is made by biopsy of the minor salivary glands of the lips.
In SS, usually all of the major salivary glands are involved. In the acute stage, swelling and hypoechoic transformations are found. Often the glands are heterogeneous because of inflammation, enlarged lymph nodes, and myoepithelial hyperplasia ( Fig. 25 ). The peripheral ductal system may be dilated; furthermore, multiple small cysts are found. The sonographic changes correlate with histological involvement( Fig. 26 ). With time, the glands become small, hypoechoic, heterogeneous, and difficult to delineate ( Fig. 27 ).
Color Doppler shows hypervascularization in the acute inflammatory stage ; however, when the salivary production is impaired owing to chronic fibrotic changes, the arterial blood flow reaction caused by stimulation is diminished. Salivary stimulation causes a significant elevation of the arterial blood flow. In SS, the maximum systolic flow velocity is often doubled.
An important issue in SS is to rule out malignant lymphoma, which has an increased incidence in this disease; however, in a heterogeneous gland it is difficult to rule out small lesions through imaging. For hypoechoic lesions larger than 2 cm and for rapidly growing lesions, a biopsy should be performed.
Kimura’s disease
Kimura’s disease, a non-neoplastic-hyperplastic multinodular lymph node disease, occurs predominately in the Asian population. Often the cervical lymph nodes and the nodes in the salivary glands are involved. No specific, distinguishable sonographic signs have been described, however.
Salivary gland infections or sialitis
Infection of a salivary gland is called sialitis , which can be further divided into infection of the gland itself, or sialadenitis , and infection of the salivary duct or ducts, termed sialodochitis . This section will cover the most common infections.
Viral Sialadenitis
Endemic parotitis or the mumps, caused by a paramyxovirus, is the most frequent acute infection, even in the era of systematic vaccination. Usually, the clinical presentation is sufficient for a definitive diagnosis. In 75% of cases both parotid glands are enlarged. Cervical lymph nodes are also always enlarged. On US, the parotid glands are enlarged with a more rounded shape, a convex lateral surface, and a hypoechoic structure. Sometimes the salivary ducts are enlarged and visible. Color Doppler demonstrates diffuse hypervascularization.
Bacterial Sialadenitis
Acute bacterial parotitis
Normally the saliva within the salivary glands is sterile. Bacterial infection can originate in several ways. The most common origin is retrograde infection via the oral cavity, bacteria infecting the gland by way of the salivary duct. Less common origins include extracapsular spread of temporomandibular joint infections and hematogenous septicemia.
Acute bacterial parotitis is as common in adults as in children. Clinical presentation is typically unilateral, with sudden pain and swelling and increased pain at each meal (salivary colic, even in the absence of lithiasis). The examination of the ostium reveals cloudy saliva or pus. Sialadenitis in adults is associated in approximately 50% of cases with sialolithiasis.
US is the only radiographic examination indicated, revealing salivary duct dilatations, hypoechoic parenchyma, and enlarged intraglandular lymph nodes ( Fig. 4 ). Hypervascularization because of the inflammation is visible on color Doppler ( Fig. 5 ). The main goal of US in inflammatory diseases is to rule out lithiasis or other ductal obstructions. In severe infections, intraglandular liquid spaces, implying abscess formation, may be observed and are more frequent in diabetic patients. Air may also be seen, as well as moving, echoic debris within an abscess. US guidance is particularly useful for needle aspiration or drainage of the abscess ( Fig. 6 ).




