Chapter 22
CHOROID

Two important trauma-related conditions involve the posterior uvea: choroidal rupture and SCH. The universally used term choroidal rupture is inaccurate because in addition to the rupture of Bruch’s membrane, there is associated injury to the adjacent choriocapillaris and a break in the overlying RPE. It may lead to legal blindness if the fovea is involved. In SCH,a blood accumulates external to the choroid; the diagnosis may be difficult initially because of the presence of associated tissue injuries. SCH may develop/rebleed intraoperatively and result in the expulsion of intraocular contents with total blindness. Choroidal rupture is rather common1 in contused eyes; SCH is less frequently recognized than its true incidence.
CHOROIDAL RUPTURE
Etiology and Diagnosis
Choroidal ruptures have been classified2,3 as:
• direct, occurring at the site of impact, most commonly anteriorly and parallel with the limbus; or
• indirect, occurring away from the site of impact, usually in the posterior pole concentric to the optic disk or through the fovea (Fig. 22–1).
Choroidal rupture must always be ruled out in contused eyes; the lower (indirect) incidence figureb in rupture injuries is probably due to the diffusion of the expansile forces and to the eyewall defect acting as a vent to release the force of the impact. The choroidal rupture in contusion trauma is probably caused by a rapid shortening of the globe’s anteroposterior diameter and its expansion in the frontal plane. The relatively rigid sclera and the relatively distensible choriocapillaris and sensory retina are more resistant and thus less likely to rupture than Bruch’s membrane. The crescent shape of indirect choroidal ruptures may be secondary to a “tethering” effect of the optic nerve.4
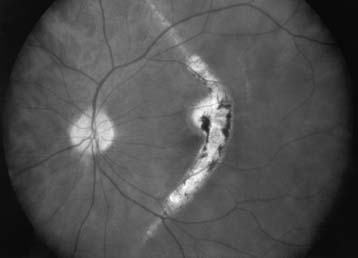
FIGURE 22–1 Fundus photograph showing a choroidal rupture through the center of the fovea.
The diagnosis of an indirect choroidal rupture is easily made with the IBO; if obscured by overlying subretinal and/or vitreous hemorrhage,4–7 the rupture remains invisible until the blood resolves, also limiting the usefulness of FA in earlier detection.5–8 ICG imaging appears more helpful.7,9,10 Studies of associated visual field defects have been inconsistent, but usually there is no direct correlation between the perimetry findings and the location of the rupture.8
PEARL… Early identification of a transfoveal choroidal rupture assists the clinician in providing the patient with a more realistic prediction regarding the visual outcome.
Prognosis
The injured eye’s vision can vary with time: it may be initially poor due to overlying hemorrhage but improve as the hemorrhage resolves. A more realistic prognostic indicator is the location of the rupture in relation to the fovea4,11; in patients with:
• subfoveal rupture, the vision tends to remain poor;
• extrafoveal rupture, the vision may remain excellent until and unless CNV develops;
• contusion maculopathy, the visual potential is limited (Fig. 22–2).
The development of CNV is a late (even 37 years after injury16) cause of vision loss12–16 (Fig. 22–3). CNV presumably occurs from choroidal capillaries growing through the breaks in Bruch’s membrane. Ruptures closer to the fovea and with greater length may have an increased risk of subsequently developing CNV.11
Treatment
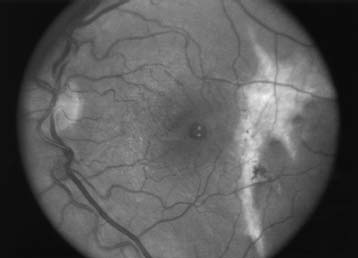
FIGURE 22–2 Choroidal rupture temporal to the fovea with associated traumatic macular hole.
Treatment
• There is no treatment for the rupture itself, although surgery may be indicated for the subretinal or vitreous hemorrhages (see Chapter 23). The CNV commonly regresses spontaneously2 or may not progress, for which the relatively healthy RPE surrounding the lesions may be responsible.16,c Photocoagulation, even though shown to prevent the recurrence of CNV in association with choroidal rupture,12,13 should therefore be used with caution.
• Extrafoveal CNVs may be photocoagulated.
• Subfoveal and juxtafoveal lesions are usually observed, although successful surgical removal of subfoveal choroidal neovascular membranes in eyes with previously good vision has been reported.18 Surgical results may nevertheless be limited by a high recurrence rate.
PEARL… CNV associated with choroidal rupture, usually responding poorly to laser photocoagulation, often involutes spontaneously, leaving a relatively small scotoma.
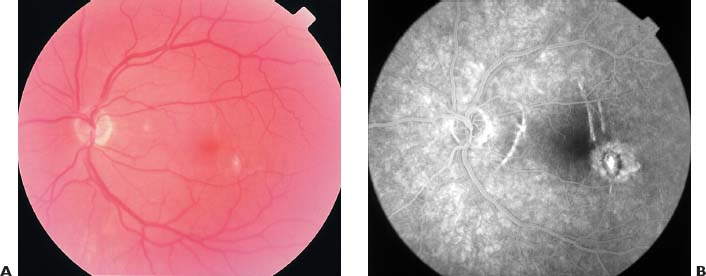
FIGURE 22–3 Choroidal rupture with associated choroidal neovascular membrane temporal to the fovea. (A) Clinical appearance. (B) Corresponding FA.
Photodynamic therapy may eventually become a treatment option; however, to date, there is no datum or even anecdotal clinical report regarding this treatment.
SCHd
Anatomy and Pathophysiology
The suprachoroidal space is a potential one between the choroid and the sclera, containing only approximately 10 µL of fluid.19 The choroid is attached to the sclera at the edge of the optic nerve, at the scleral spur, and at the ampullae of the vortex veins. The arterial supply of the choroid comes mainly through the short posterior ciliary arteries20 (Fig. 22–4); the long posterior ciliary arteries, passing within the suprachoroidal space, contribute by forming anastamoses with the short posterior ciliary arteries.

FIGURE 22–4 Drawing of dissected globe. Choroidal arteries that enter the suprachoroidal space by piercing the sclera surrounding the optic nerve can be seen radiating from the optic nerve (left). Two vortex veins are at the top and bottom. (From Tasman W, Jaeger EA, ed. Duane’s Foundations of Clinical Ophthalmology. Philadelphia: Lippincott Williams & Wilkins, 1999:8, by permission from Lippincott Williams & Wilkins.)
Many hypotheses have been proposed for SCH development.21–24 It is probably caused by the rupture of a short/long posterior ciliary artery, rapidly filling the suprachoroidal space with blood.
• SCH in open globe injuries may be related to direct trauma to the vessels.
• Contusion may cause SCH via vessel rupture due to shearing forces (anteroposterior shortening and equatorial expansion of the globe).
• SCHs can be precipitated by hypotony, presumed to lead initially to choroidal effusion with subsequent expansion of the suprachoroidal space, causing stretching and rupture of the ciliary arteries and potential expulsion of intraocular contents through the wound.23
Etiology, Epidemiology, and Risk Factors
SCH may occur intraoperatively20–22,24–27 with tissue extrusion (expulsive SCH, Fig. 22–5), postoperatively (delayed SCH), or even spontaneously.28–31
PEARL… The incidence of SCH in trauma is not known but appears to be greatly underreported. Analyzing the pathological specimens of a series of 28 NLP eyes that underwent enucleation due to rupture, an incidence of 100% was found even though clinically not a single eye was described to have SCH.33

FIGURE 22–5 Clinical appearance of an intraoperative expulsive SCH (cataract extraction).
| Systemic | advanced age | |
| anticoagulation | ||
| atherosclerotic disease | ||
| blood dyscrasias | ||
| diabetes mellitus | ||
| hypertension | ||
| Ocular | aphakia/pseudophakia | |
| choroidal arteriolar sclerosis | ||
| history of previous vitrectomy | ||
| increased axial length | ||
| increased preoperative IOP | ||
| Peri-/intraoperative | acute drop in IOP | |
| general anesthesia | ||
| hypertension | ||
| intraoperative tachycardia | ||
| retrobulbar anesthesia without epinephrine | ||
| Valsalva maneuvers | ||



