Chapter 32
CHEMICAL INJURIES: CLINICAL COURSE AND MANAGEMENT

The etiology and therapeutic strategies for acute management of chemical injuries of the eye were discussed in Chapter 11; here we focus on the pathophysiologic mechanisms that influence subsequent therapeutic strategies; the evolving clinical course; specific therapeutic recommendations during the acute, early repair, and late repair phases; and the visual rehabilitation of patients with severe chemical injuries.
PATHOPHYSIOLOGY
The management of chemical injuries after initial emergency intervention is based on an understanding of the complex interactions between:
• ocular surface regeneration;
• stromal matrix degradation and repair; and
• the inflammatory response.
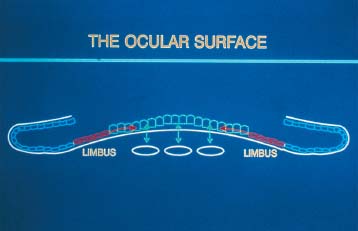
Ocular Surfacea Regeneration
Centripetal movement of cells from the peripheral cornea, limbus, or conjunctiva is responsible for the normal2,3 or pathologic4,5 replacement of the corneal epithelium. The limbal epithelial region serves as the generative tissue for corneal epithelial cells (Fig. 32–2).6–8,b
Following epithelial débridement of the entire corneal and limbal epithelium, the surrounding conjunctival epithelium not only resurfaces the cornea but also evolves to resemble the normal corneal epithelium phenotypically.9
PEARL… The process termed “transdifferentiation”10 (i.e., the conjunctival epithelium evolving to become corneal epithelium) established the rationale for conjunctival autograft transplantation as a means of surgically restoring the ocular surface of chemically injured eyes.11
Transdifferentiation of the conjunctival epithelium is, however, rarely (if ever) complete, especially after severe chemical injury,1,12,13 and is associated with:
• delayed reepithelialization14;
• superficial and deep stromal neovascularization12;
• persistence of goblet cells within the corneal epithelium13; and
• recurrent epithelial erosions due to abnormal epithelial basement membrane14.
If the limbal stem cell loss is complete, severe superficial pannus invariably occurs, resulting in “conjunctivalization” of the resurfaced cornea.15
PEARL… The limbal stem cells appear to be the most qualified cells to restore functional competence after extensive ocular surface as well as limbal stem cell injury.16,17
Corneal Stromal Degradation and Repair
PEARL… The maintenance and regeneration of the corneal stroma are the primary function of the keratocyte.18,19 Following chemical injury, keratocytesc are mobilized from adjacent regions to repopulate the area of injury.24
PITFALL
Keratocyte synthesis of collagen may be compromised by deficient levels of ascorbate in the aqueous following severe chemical injury25 or by the injudicious use of topical corticosteroids.26,27
Type I collagen synthesis is maximum between days 7 and 56, with a peak at day 21.24 It is essential to prevent stromal ulceration due to collagenolysis.
• MMPs (formerly known as collagenase) cause specific cleavage of the collagen molecule.28,29 MMP-1 and MMP-8,d produced by keratocytes21,22 and polymorphonuclear leukocytes,30,31 respectively, can degrade type I, II, or III fibrillar collagen in the corneal stroma. These enzymes are not present in significant amounts until 14–21 days after chemical injury, corresponding to the period of maximal collagen synthesis and repair.32
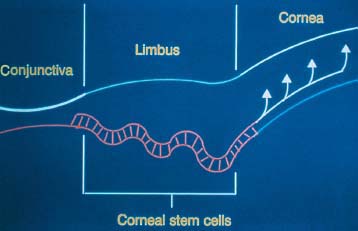
FIGURE 32–2 Schematic depiction of the corneal basal epithelial cells. Basal epithelial (stem) cells migrate centripetally along the basal epithelial layer and then anterior toward the surface. (From Wagoner MD, Kenyon KR, Shore JS. Ocular surface transplantation. In: Barrie J, Kirkness C, eds. Recent Advances in Ophthalmology. Vol 9. New York: Churchill Livingstone; 1995:59–90. Reprinted with permission from Churchill Livingstone.)
Inflammatory Response
The association of inflammation with corneal ulceration and its cessation following exclusion of inflammatory cells are well recognized.33–36
Within 12–24 hours after chemical injury, infiltration of the peripheral cornea with inflammatory cells occurs.37 If the injury is severe, a second wave of inflammatory cell infiltration:
• begins at 7 days; and
• peaks between 14 and 21 days when corneal repair and degradation are maximal.37
Persistent inflammation may delay reepithelialization38 and perpetuate continued inflammatory cell recruitment, thereby initiating a vicious circle of progressive inflammatory cell-related destruction of the corneal stroma.
CLINICAL EVALUATION AND COURSE
Previous gradings of chemical injury severity39,40 stressed the prognostic importance of vascular ischemia and necrosis in the limbal zone.
Table 32–1 shows the limbal stem cell-based classification system41 we propose to guide the intervention and predict the outcome.
The clinical course (see Table 32–2) after chemical injury progresses through three distinct phases:
• acute (0–7 days);
• early repair (7–21 days); and
• late repair (>21 days).42
The healing pattern occurring during these phases correlates with the original degree of limbal stem cell injury and provides support for subsequent therapeutic decisions.
| Grade | Stem Cells | See Figure |
|---|---|---|
| Grade I | Little or no loss of stem cells | 3A,C |
| Grade II | Subtotal stem cell loss | 4A, C |
| Grade III | Complete stem cell loss | 5A, C |
| Grade IV | Complete stem cell loss + loss of proximal conjunctival epithelium | 6A, C |
THERAPEUTIC PRINCIPLES
Three-Step Approach
Our modified three-step approach to sterile corneal ulceration, (that is:
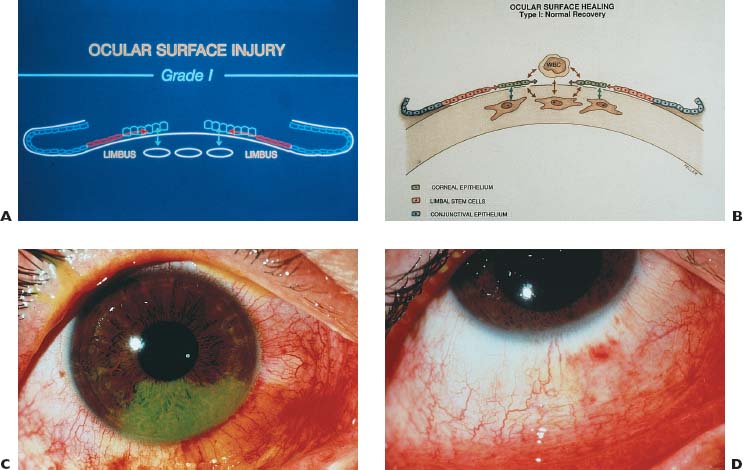
FIGURE 32–3 (A) Grade III chemical injury: schematic. The epithelial defect involves corneal epithelium but not limbal stem cells.(B) Type III healing pattern: schematic. During the brief period required for reepithelialization with normal phenotypic epithelium, all interactions between epithelium, inflammatory cells, and keratocytes are appropriate for repair. (C) Grade I chemical injury: clinical appearance. Epithelial defect involving one quadrant without significant limbal ischemia or evidence of limbal stem cell loss. (D) Type I healing pattern: clinical appearance. Prompt reepithelialization with normal corneal epithelial appearance without vascularization confirms that limbal stem cells adjacent to the corneal epithelial defect were unaffected by the chemical injury. (From Wagoner MD. Chemical injuries of the eye: current concepts in pathophysiology and therapy. Surv Ophthalmol. 1997;41:275–313. Reprinted with permission from Elsevier Science.)
| Phase (Days) and Type | Clinical Picture | See Figure |
|---|---|---|
| Acute (0–7) | ||
| Type I | Reepithelialize without incident | 3B, D |
| Type II | Delayed reepithelialization | 4B |
| Type III | Little or no reepithelialization | 5B |
| Type IV | Little or no reepithelialization | 6B |
| Early repair (7–21) | ||
| Type II | Delayed reepithelialization in deficient quadrant +/– vascularization | |
| Type III | Persistent epithelial defect | |
| Type IV | Persistent epithelial defect | |
| Late repair (21+) | ||
| Type II | Persistent epitheliopathy with or without neovascularization in limbal stem cell-deficient quadrant | 4D |
| Type III | Little or no reepithelialization, with progressive “conjunctivalization” of the corneal surface over a several month period | 5D |
| Type IV | Continued absence of epithelium from both the proximal conjunctiva and cornea with development of sterile corneal ulceration | 6D |
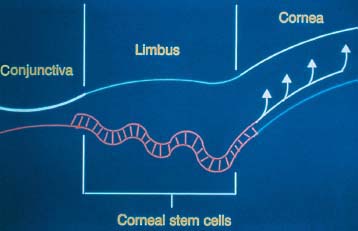
FIGURE 32–4 (A) Grade II chemical injury: schematic. Injury to the corneal epithelium and partial limbal stem cell loss. (B) Type II healing pattern: schematic. Reepithelialization from areas of normal limbal stem cells proceeds normally, while reepithelialization in areas of limbal stem cell loss is initially from conjunctival epithelium. Transient subepithelial vascularization may accompany the conjunctival epithelium. Interactions between epithelium, inflammatory cells, and keratocytes are usually appropriate for repair. (C) Grade II chemical injury: clinical appearance. In the quadrant with epithelial defect there is obvious limbal ischemia and probable loss of limbal stem cells (in contrast to the appearance in Fig. 32–5C). (D) Type II healing pattern: clinical appearance. Following reepithelialization, there are persistent epitheliopathy, subepithelial vascularization, and stromal haze. (From Wagoner MD. Chemical injuries of the eye: current concepts in pathophysiology and therapy. Surv Ophthalmol. 1997;41:275-313. Reprinted with permission from Elsevier Science.)
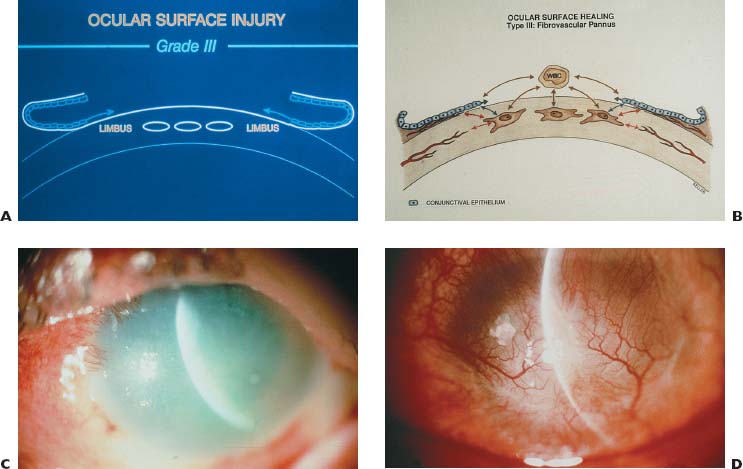
FIGURE 32–5 (A) Grade Ill chemical injury: schematic. There is loss of all corneal epithelium and limbal stem cells but preservation of the proximal conjunctiva. (B) Type Ill healing pattern: schematic. All reepithelialization must come from the conjunctival epithelium, which is usually considerably delayed. Interactions between the conjunctival epithelium, inflammatory cells, and keratocytes may or may not result in appropriate corneal repair. (C) Grade III chemical injury: clinical appearance. There is complete corneal and proximal conjunctival epithelial defect with loss of corneal stromal clarity. (D) Type Ill healing pattern: clinical appearance. There is complete coverage of the cornea with “conjunctivalized” epithelium and superficial and deep stromal vascularization. (A and B from Wagoner MD. Chemical injuries of the eye: current concepts in pathophysiology and therapy. Surv Ophthalmol. 1997;41:275–313. Reprinted with permission from Elsevier Science. C and D from Wagoner MD, Kenyon KR, Shore JS. Ocular surface transplantation. In: Barrie J, Kirkness C, eds. Recent Advances in Ophthalmology. Vol 9. New York: Churchill Livingstone; 1995:59–90. Reprinted with permission from Churchill Livingstone.)
1. promoting reepithelialization/transdifferentiation;
2. limbal stem cell transplantation; and
3. human amniotic membrane transplantation);
remains applicable to the entire clinical course following chemical injury.34,35
Step 1. Promoting Reepithelialization/ Transdifferentiation
The reestablishment of an intact and phenotypically normal corneal epithelium is the most important determinant of favorable outcome following chemical injury. In grade III or IV injuries,e surgical restoration of a suitable stem cell population is mandatory to achieve this objective.
Step 2. Limbal Stem Cell Transplantation
Limbal autograft transplantation involves harvesting from the limbus of the patient’s uninjured or less injured contralateral eye:
• two crescents of peripheral corneal limbal epithelium with
• a corresponding section of the conjunctiva (Fig. 32–7).16
This treatment is becoming standard even in the early clinical course of severe chemical injury, prior to the development of conjunctivalization of the corneal surface in grade III injury (Fig. 32–8) or corneal stromal ulceration in grade IV injury (Fig. 32–9).
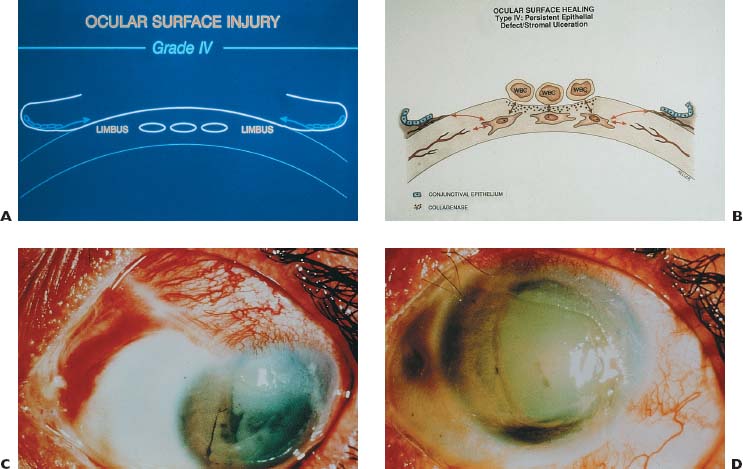
FIGURE 32–6 (A) Grade IV chemical injury: schematic. There is loss of all corneal epithelium and limbal stem cells and proximal conjunctiva. (B) Type IV healing pattern: schematic. Little or no reepithelialization is expected from the distal conjunctival epithelium. Interactions between inflammatory cells and keratocytes, in the absence of modulation by migrating epithelium, result in excessive collagenolysis instead of appropriate repair. (C) Grade IV chemical injury: clinical appearance. Complete corneal epithelial defect with limbal ischemia remains unchanged 4 months after the original injury. (D) Type III healing pattern: clinical appearance. Sterile corneal ulceration with perforation and iris prolapse in the inferior cornea. A mature cataract is also present. (A and B from Wagoner MD. Chemical injuries of the eye: current concepts in pathophysiology and therapy. Surv Ophthalmol. 1997;41:275–313. Reprinted with permission from Elsevier Science. D from Mandel ER, Wagoner MD. Atlas of Corneal Disease. Philadelphia: WB Saunders; 1989:72. Reprinted with permission from WB Saunders.
Limbal allograft transplantation with stem cells obtained from a living relative43–45 or cadavers46–49 is necessary in bilateral injuries.
• Limbal tissue may be harvested from the entire circumference of cadavers and transplanted to the entire limbal zone of the donor eye.46,–47
• Limbal tissue harvested from living relatives is obtained in a manner identical to that described for limbal autografts, taking care not to excise more than 6 clock hours of limbal tissue.43
• It has been demonstrated that human limbal stem cells can survive in animal models.50,51
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


