Purpose
To examine the clinical characteristics of periconus choroidal neovascularizations (CNVs) in eyes with pathologic myopia.
Design
Retrospective observational case series.
Methods
We reviewed the medical records of 260 eyes of 254 patients with a myopic CNV and selected those with a periconus CNV. A periconus CNV was defined as a CNV that is located next to a myopic conus. To differentiate a periconus CNV from a subfoveal CNV that has expanded to the edge of the disc, eyes whose CNV involved the fovea were excluded. The data of the eyes with a subfoveal CNV were used for comparison.
Results
Eleven eyes (4.2%) of 11 patients had a periconus CNV. These CNVs had a triangular or oval shape whose base was directed toward the myopic conus. The eyes with a periconus CNV had a significantly larger myopic conus than eyes with a subfoveal myopic CNV. The degree of myopia and axial length were not significantly associated with the incidence of periconus CNV. In 5 of the 11patients, the periconus CNV had a spontaneous regression without treatment, and none had a recurrence. The other 6 patients received treatment and obtained an angiographic closure after a single treatment. A chorioretinal atrophy (ChRA) developed in 3 eyes, and the ChRA enlarged over the fovea in 2 of these eyes, which led to a significant decrease of vision.
Conclusion
A periconus CNV is rare (4.2%) among the eyes with a myopic CNV and is more likely to develop in eyes with a large myopic conus. The absence of a significant association between the degree of myopia and incidence of periconus CNV suggests that the morphologic characteristics of the eye are not the causes of the periconus CNV. Although an angiographic closure can be easily attained with or without the treatment, the later development and progression of ChRA can impair vision.
Achoroidal neovascularization (CNV) that is located at the border of the optic disc or next to an adherent atrophy has been described as a peripapillary CNV. A peripapillary CNV typically extends from the disc margin in a “tongue-like” fashion, and it is more commonly found on the temporal side of the disc. This temporal location will more likely cause visual symptoms, and thus the higher incidence of peripapillary CNV located here may be because these patients seek examinations for their visual symptoms.
Information on the clinical characteristics of peripapillary CNV is more sparse than that for macular CNV, probably because of its lower incidence. Silvestri and associates reported that peripapillary CNV accounts for less than 10% of all CNV occurring at the posterior pole of the eye. Browning and Fraser studied 115 eyes with peripapillary CNV and found 45.2% were associated with age-related maculopathy, 39.1% with idiopathic CNV, 4.3% with multifocal choroiditis, 2.6% with angioid streaks, 1.7% with histoplasmosis, 1.7% with choroidal osteoma, 0.9% with optic disc drusen, and 0.9% with congenital disc anomaly.
We noted that highly myopic eyes with a large conus around the optic disc occasionally had CNV that developed at the edge of the conus. However, only 1 of the 50 articles extracted by a PubMed search on December 7, 2010 using keywords “peripapillary” and “neovascular membranes” described a case with peripapillary CNV in eyes with pathologic myopia. In that report, Silvestri and associates studied the natural course of peripapillary CNV in 20 eyes, but only 1 eye had a myopic CNV, and the CNVs of the other eyes were associated with age-related macular degeneration (AMD), idiopathic CNV, and inflammatory disorders. Unfortunately, the details of the patient with peripapillary CNV in the eye with pathologic myopia were not presented.
Thus, the purpose of this study was to determine the incidence and clinical characteristics of peripapillary CNV in eyes with pathologic myopia. Because peripapillary CNV develops around the myopic conus in highly myopic eyes, we have used the term “periconus CNV” in the present study. We shall show that periconus CNV is more often found in eyes with a large conus and has a tendency to regress with or without treatment. However, a secondary enlargement of a chorioretinal atrophy (ChRA) around the CNV to the fovea could impair vision.
Methods
We reviewed the medical records of 260 eyes of 254 consecutive patients with a myopic CNV who visited the High Myopia Clinic at Tokyo Medical and Dental University between April 1990 and December 2008. We selected the medical records of eyes with a periconus CNV. The inclusion criteria were: 1) myopic refractive error (spherical equivalent) ≥6.0 diopters (D) or axial length ≥26.5 mm; 2) presence of a periconus CNV; 3) evidence of leakage from the CNV in the fluorescein angiograms (FA); 4) initial examination within 6 months after the onset of the visual symptoms related to a CNV (metamorphopsia, vision decrease); and 5) minimum follow-up period of 6 months after the onset.
In non–highly myopic eyes, Lopez and Green defined a peripapillary CNV as a collection of new subretinal vessels, any part of which is located within 1 disc diameter of the margin of the optic disc. In our study, a periconus CNV was defined as a CNV that was connected to the myopic conus. To differentiate a periconus CNV from a subfoveal CNV that enlarged to the conus, eyes whose CNV involved the central fovea were excluded.
The best-corrected visual acuity (BCVA) was determined by a Landolt C chart, and the decimal BCVA was converted to the logarithm of minimal angle of resolution (logMAR) for statistical analyses. A comprehensive ocular examination including dilated ophthalmoscopy and macular examinations with a contact lens or a +78-D lens, followed by color fundus photography and FA, were performed during the follow-up period.
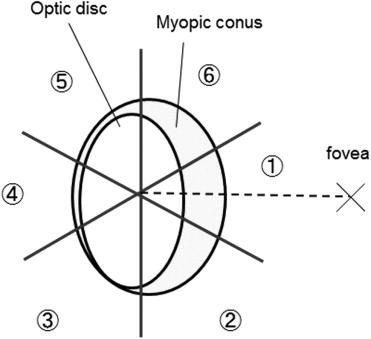
The distribution of CNV in relation to the optic disc and central fovea was determined according to the method shown in Figure 1 . The location of the CNV was divided into 6 distinct zones. Zone 1 was a 60-degree sector that covered 30 degrees above and 30 degrees below a line connecting the center of the optic disc and the central fovea. The remaining 5 sectors of 60 degrees surrounded the conus in a clockwise direction, and are referred to as zones 2 through 6 ( Figure 1 ). Because all of the CNVs were classic CNV, the area of the CNV was determined in the early FA images, 1 minute after dye injection, using the software of the imaging system (PDT/MPS software; Topcon, Tokyo, Japan) based on the data of axial length of each eye. A regression of the CNV was defined as a disappearance of dye leakage from the CNV in the fluorescein angiograms, and the progression of CNV was defined as an increase in the CNV size. The conus area was calculated as the area within the myopic conus minus the area of the optic disc, and the area of the ChRA around a regressed CNV was calculated as the area within the ChRA minus the area of CNV, as we have reported.
Prior to October 2003, all the patients with a myopic CNV were followed without treatment. Between November 2003 and September 2005, patients with a myopic CNV received trans-Tenon’s retrobulbar infusion of triamcinolone acetonide (TA). Between October 2004 and November 2006, patients were treated with photodynamic therapy (PDT) with verteporfin. Since December 2006, all of the eligible patients were treated with an intravitreal injection of bevacizumab (IVB). The treatment protocol for TA, PDT, and IVB has been described in detail.
The clinical characteristics and the anatomic and visual outcomes of the patients with periconus CNVs were evaluated. Also, the clinical characteristics of the eyes with periconus CNVs were compared to eyes with a subfoveal CNV associated with pathologic myopia. Some of the data of the eyes with subfoveal CNV were published in our previous studies. The location of the CNV was classified as subfoveal if the CNV included the central fovea, and was classified as juxtafoveal if the CNV did not include the central fovea but the margin of the CNV was within 200 μm from the foveal center. The other CNVs were classified as extrafoveal.
Statistical Analyses
The significance of the differences in the patients’ age, refractive error, axial length, and visual acuity in logMAR units among the groups was determined by Mann-Whitney U tests. A P value of .05 was accepted as being statistically significant.
Results
The review of the medical records showed that among the 260 eyes (254 patients) with a myopic CNV who visited our High Myopia Clinic between 1990 and 2008, 168 eyes (164 patients) had subfoveal CNV, 77 eyes (75 patients) had juxtafoveal CNV, and 15 eyes (15 patients) had extrafoveal CNV. Among 15 eyes with extrafoveal CNV, 11 eyes of 11 patients had a periconus CNV. Thus, the incidence of periconus CNV in all of the highly myopic eyes was 4.2% (11 of 260 eyes). The clinical characteristics of these patients are shown in Table 1 . The mean age was 60.5 ± 16.6 years. The mean refractive error (spherical equivalent) was −14.5 ± 4.8 D, and the mean axial length was 29.6 ± 1.4 mm. The mean CNV area was 2.8 ± 4.1 mm 2 , and the mean follow-up period was 28.3 ± 35.8 months. A posterior staphyloma was present in 8 of the 11 eyes. Eight eyes had an annular crescent and 3 of these eyes had a temporal crescent.
| Case No. | Age (Years) | Gender | Side | Refractive Error (D) | Axial Length (mm) | Type of Myopic Conus | Area of Myopic Conus (mm 2 ) | Zone of CNV | logMAR | Size of CNV (mm 2 ) | Development of ChRA | Size of ChRA Around CNV (mm 2 ) | Treatment | Follow-up Period After Onset (Months) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| At Baseline | At Final Visit | At Baseline | At Final Visit | |||||||||||||
| 1 | 70 | M | L | −20.0 | 31.4 | Annular | 22.9 | 1 | 0.4 | 1.0 | 0.6 | 0.4 | + | 9.6 | − | 134 |
| 2 | 40 | F | L | −12.0 | 30.5 | Annular | 16.1 | 1 | 0.7 | 0.0 | 4.0 | 2.5 | − | NA | − | 30 |
| 3 | 74 | F | L | −6.5 | 26.8 | Annular | 7.0 | 1 | 1.1 | 1.1 | 2.0 | 1.4 | − | NA | − | 9 |
| 4 | 82 | F | R | IOL | 28.4 | Annular | 12.6 | 1 | 0.7 | 0.7 | 0.6 | 0.2 | − | NA | − | 15 |
| 5 | 45 | M | L | −16.0 | 31.2 | Annular | 13.0 | 1 | 0.0 | 0.0 | 2.6 | 2.6 | − | NA | − | 12 |
| 6 | 78 | F | L | −16.5 | 30.2 | Annular | 39.6 | 1 | 0.4 | 0.1 | 0.8 | 0.6 | − | NA | TA | 26 |
| 7 | 42 | F | L | −11.5 | 28.1 | Temporal | 3.0 | 1,6 | 0.0 | −0.1 | 2.2 | 0.5 | + | 2.6 | PDT | 24 |
| 8 | 71 | F | L | −13.5 | 29.2 | Temporal | 2.4 | 1 | 0.4 | 0.4 | 0.5 | 0.2 | − | NA | IVB | 9 |
| 9 | 59 | F | R | −22.0 | 29.8 | Annular | 23.9 | 1 | 0.5 | 0.4 | 1.6 | 0.4 | − | NA | IVB | 24 |
| 10 | 67 | F | L | −17.0 | 30.7 | Annular | 37.4 | 1 | 0.2 | 1.0 | 1.6 | 1.3 | + | 13.7 | IVB | 18 |
| 11 | 37 | M | L | −9.5 | 28.9 | Temporal | 3.5 | 1,2,3 | 0.7 | 0.8 | 14.7 | 14.9 | − | NA | IVB | 10 |
The BCVA at the onset varied ( Table 1 ), and 2 of the 11 patients (Cases 5 and 7) had a BCVA of 0 logMAR units despite the presence of metamorphopsia. The shape of the periconus CNV was triangular or oval, and the base of the CNV faced the myopic conus in the 11 eyes ( Figures 2 through 4 ). In 9 of the 11 eyes, the entire periconus CNV was within zone 1. In 1 eye (Case 7 in Table 1 ), the periconus CNV was located over zones 1 and 6. In the remaining eye (Case 11 in Table 1 ), the large CNV covered zones 1 to 3. All of the CNVs were the classic type of CNV; thus the CNVs were hyperfluorescent from the early phase until the late phase of FA. No obvious lacquer cracks were detected ophthalmoscopically by FA.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


