and Mitrofanis Pavlidis2
(1)
Department of Ophthalmology, Uppsala University Hospital, Uppsala, Sweden
(2)
Augencentrum Köln, Cologne, Germany
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-319-20236-5_26) contains supplementary material, which is available to authorized users.
Electronic supplementary material
for this chapter is accessible online at http://extras.springer.com/ by searching via the ISBN.
26.1 General Introduction
The case reports are structured according to the ocular anatomy: They begin with the cornea and end with the retina.
26.2 Surgical Management of a Corneal Perforation
Case Report No. 17: Corneal Perforation and Large Iris Defect
Video: No video available
Figures 26.1, 26.2, 26.3, 26.4, 26.5, 26.6, 26.7 and 26.8

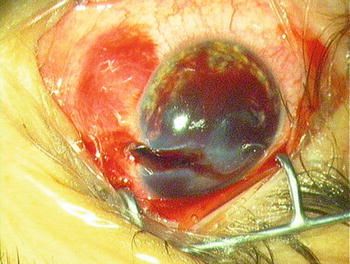
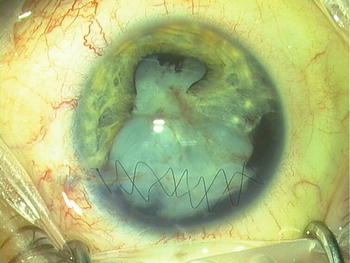
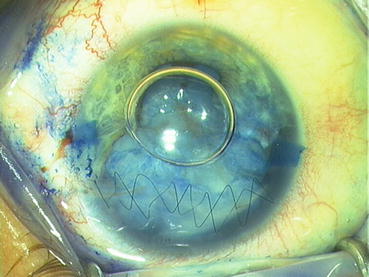
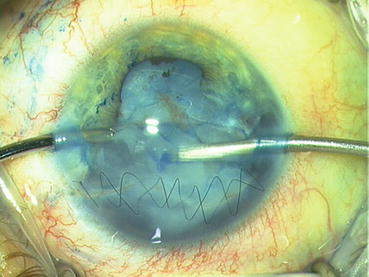
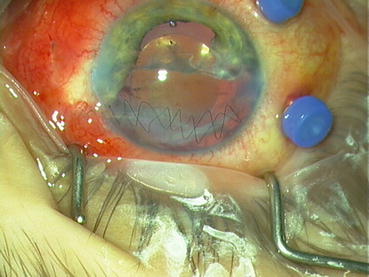


Fig. 26.1
Case report 17: a handyman injured his eye with a screw driver
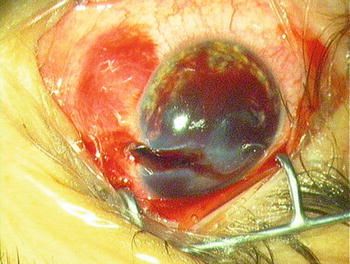
Fig. 26.2
Case report 17: the superior cornea is perforated
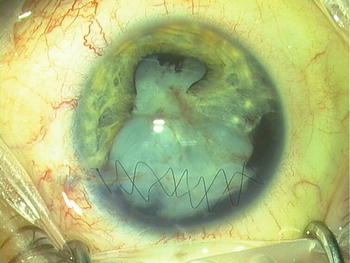
Fig. 26.3
Case report 17: 4 weeks follow-up. A continuous suture of the central cornea was performed. At the limbus, a single suture is used. Continuous sutures are easier to perform and watertight
Fig. 26.4
Case report 17: a drawing for corneal sutures. In the centre: continuous suture. At the limbus: single suture
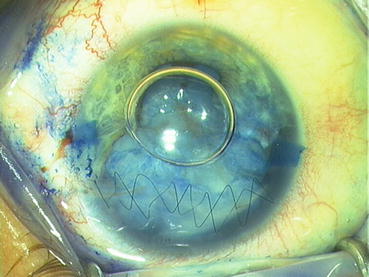
Fig. 26.5
Case report 17: second surgery. 1 month after first surgery: staining with trypan blue
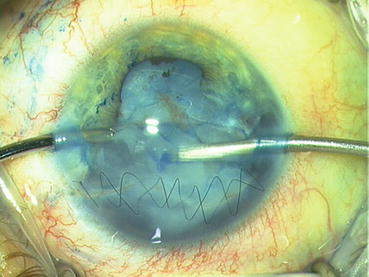
Fig. 26.6
Case report 17: removal of the soft nucleus with I/A
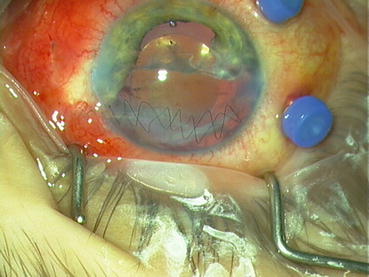
Fig. 26.7
Case report 17: implantation of a three-piece IOL. Note the large iris defect

Fig. 26.8
Case report 17: third surgery—implantation of a customized artificial iris prosthesis (Human Optics)
A 29-year-old male patient who perforated his cornea with a screwdriver during work. Visual acuity was light perception. In a first surgery, only the cornea was sutured. The visual acuity was HM and a vitreous haemorrhage was present. The patient was followed up every week, and in the fourth week, a retinal detachment was detected with B-scan. A second operation with phacoemulsification and vitrectomy + silicone oil was performed. The visual acuity was 0.1 and a silicone oil removal + IOL reposition was performed 1 month later. During the postoperative follow-up, the patient complained of severe photophobia and visual acuity was 0.1–0.2. Eight months later, an iris prosthesis with 11 mm diameter was implanted into the sulcus without sutures. In a follow-up after 6 months, the patient has no complaints. In a follow-up after 12 months, the patient complains of ocular irritation and the IOL is partially dislocated. Visual acuity is 0.1–0.2.
In hindsight: I would not do anything else. Due to the retinal detachment, I had to perform a combined phacoemulsification/vitrectomy. If the retina did not detach, I would only operate the traumatic cataract and perform a vitrectomy 1 month later. The advantage of this stepwise approach is that it is easier to achieve a stable IOL position and you avoid posterior synechiae. The ocular irritation may be caused by the iris prosthesis. I prefer today a 10 mm prosthesis size for sulcus implantation and I use a trephine (Ophtec®, NL).
Case Report No. 18: Corneal Perforation in a Child
Video: No video available
Figures 26.9, 26.10, 26.11, 26.12 and 26.13

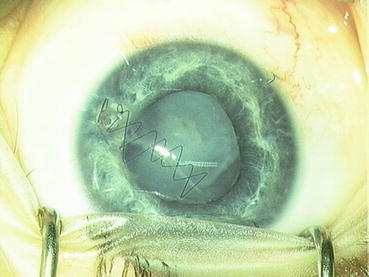
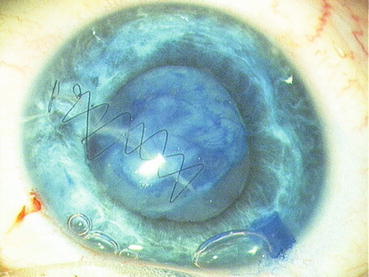
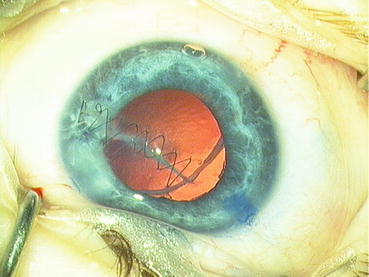
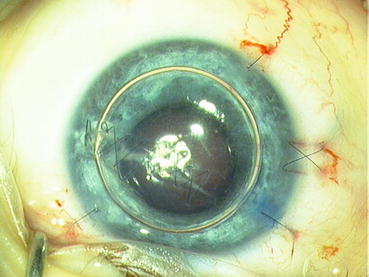

Fig. 26.9
Case report 18: corneal perforation of a 5-year-old girl with a spruce cone
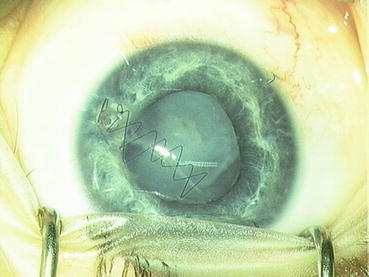
Fig. 26.10
Case report 18: 1 month after first surgery with continuous corneal suture. Note that the corneal wound is fibrotic
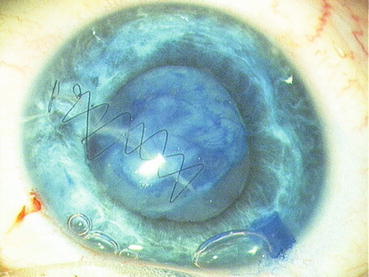
Fig. 26.11
Case report 18: staining of anterior capsule with trypan blue. The anterior capsule is partially defective. Try to make the rhexis as round as possible
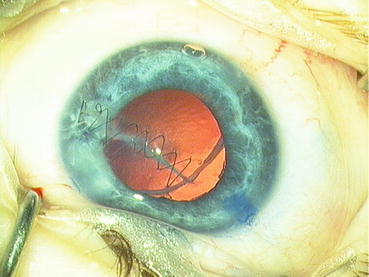
Fig. 26.12
Case report 18: the posterior capsule is intact
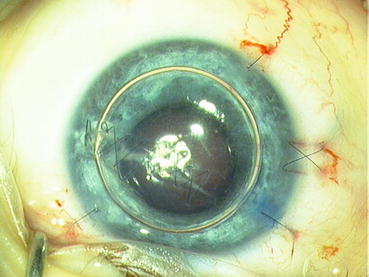
Fig. 26.13
Case report 18: in the bag implantation and an air bubble to stabilize the anterior chamber. The corneal suture was removed 1 month later
A 5-year-old female patient with her friends were jumping on a trampoline and throwing spruce cones at each other. One spruce cone hit her eye and caused a corneal perforation.
She was first operated with suturing of the corneal wound with nylon 10-0. A continuous suture was performed in the centre of the cornea and interrupted stitches at the limbus. One month later, a phacoemulsification + IOL was performed. The visual acuity in the last follow-up after 2 years was 0.9.
In hindsight: This case went very well. I think that a traumatic cataract is easier to operate after 1 month because the inflammation has subsided and the lens capsule is partially fibrotic.
26.3 Surgical Management of a Traumatic Cataract
Bonus video 26.1a: Lens injury after intravitreal injection
Case Report No. 19: Traumatic Cataract
Video 26.1b: Traumatic cataract
Figures 26.14, 26.15, 26.16, 26.17 and 26.18

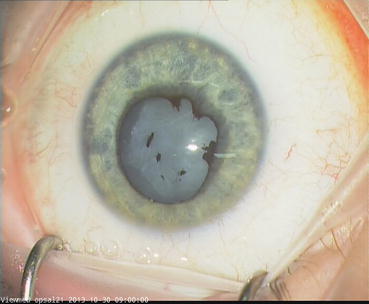
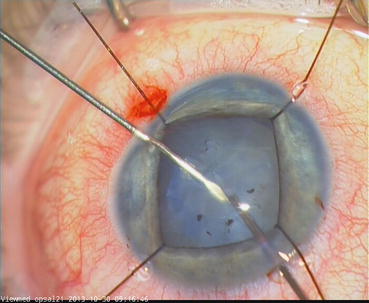
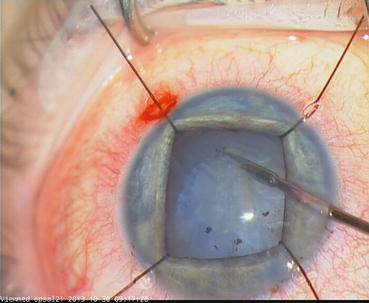
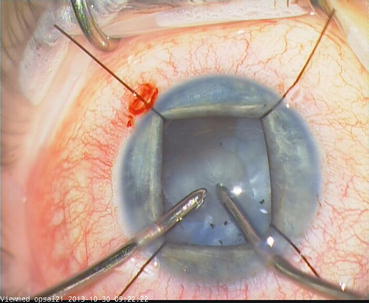

Fig. 26.14
Case report 19: blunt globe injury secondary to a fist punch
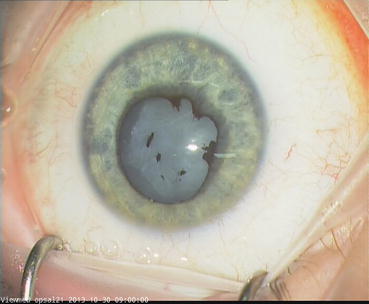
Fig. 26.15
Case report 19: posterior synechiae and a white nucleus
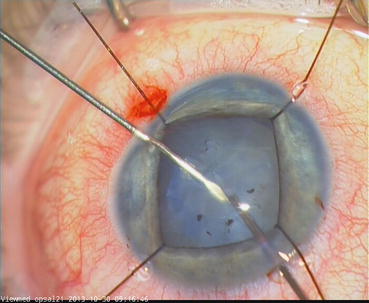
Fig. 26.16
Case report 19: very thick and fibrotic anterior capsule which can only be opened with a sharp cannula
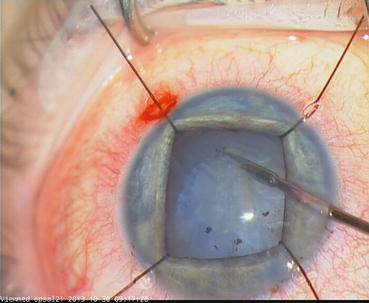
Fig. 26.17
Case report 19: a straight intravitreal scissors is very suitable for cutting a fibrotic lens capsule (23G, DORC)
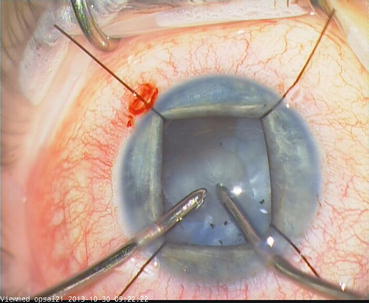
Fig. 26.18
Case report 19: the nucleus is soft and can be removed with I/A
A 35 y/o female with repeated trauma to the left eye due to physical abuse since January 2013. She indicates a gradual loss of vision in that eye, no flash phenomenon, no sudden deterioration indicated, in the past month totally hazy and no vision, and no pain. The visual acuity was light perception. A white cataract was operated with phacoemulsification and IOL. The anterior capsule was very fibrotic and could only be opened with a needle and intravitreal scissors. In addition a total retinal detachment was present and operated (see PVR detachment). The visual acuity in the final follow-up was light perception.
In hindsight: Chronic retinal detachments are surgically very demanding but functionally not rewarding. The patient should be informed about this.
Case Report No. 20: Traumatic Cataract
Video: No video available
Figures 26.19, 26.20, 26.21, 26.22 and 26.23

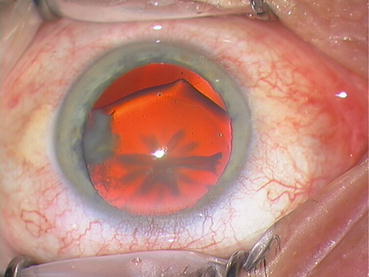
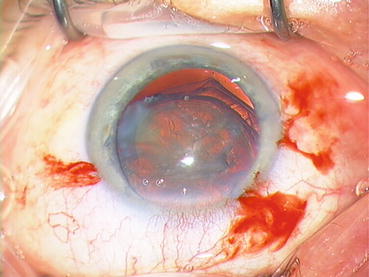
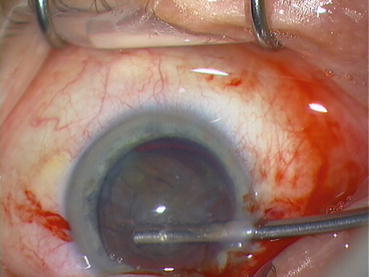
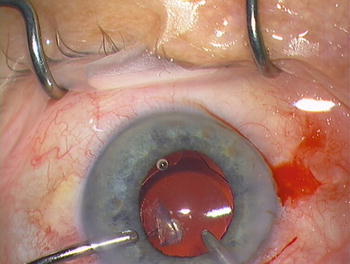

Fig. 26.19
Case report 20: a blunt ocular trauma secondary to an ice hockey puck
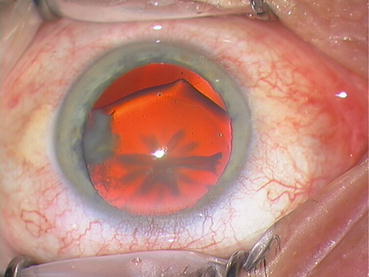
Fig. 26.20
Case report 20: a 44-year-old trauma with star-shaped cataract and large inferior zonular lysis
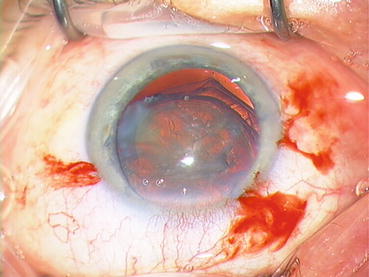
Fig. 26.21
Case report 20: circular rhexis
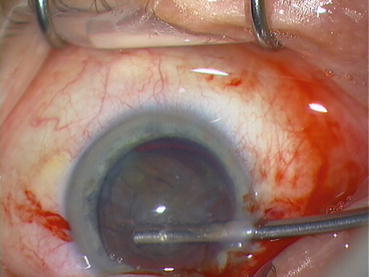
Fig. 26.22
Case report 20: early implantation of a capsular tension ring
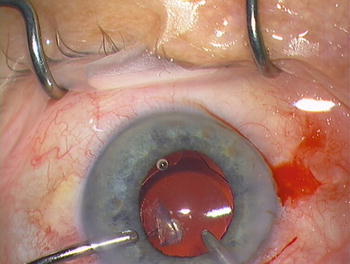
Fig. 26.23
Case report 20: in the bag implantation of a three-piece IOL (ZCB00 Tecnis)
A 70 y/o male patient was hit by a hockey puck against the left eye at the age of 26 years and was since then visually impaired. He has recently been in contact with an optician for renewal of the driving license when a lens opacity in the left eye was discovered. The patient was referred to the local eye clinic where a star-shaped traumatic cataract was detected. The patient was referred to us for further surgical intervention. Visual acuity was 0.2–0.3. A star-shaped cataract and a large inferior zonular lysis were present. A phacoemulsification with implantation of a capsular tension ring + implantation of a one-piece IOL was performed. In the final follow-up, a visual acuity of 1.0 was measured.
In hindsight: It is important to implant a capsular tension ring in order to inflate the lens capsule completely. It is also a good barrier for a vitreous prolapse.
26.4 Surgical Management of a Scleral Wound at Pars Plana
Case Report No. 21: Scleral Wound at Pars Plana Secondary to IOFB
Video: No video available
Figures 26.24, 26.25 and 26.26

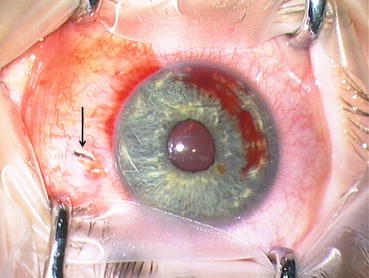
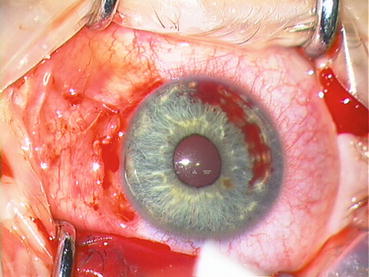

Fig. 26.24
Case report 21: again an ocular perforation when mowing the lawn
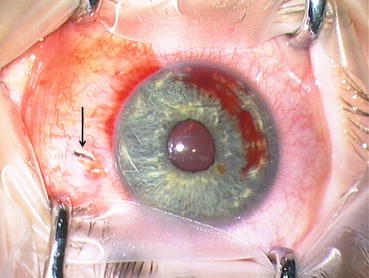
Fig. 26.25
Case report 21: note the scleral perforation at pars plana (arrow)
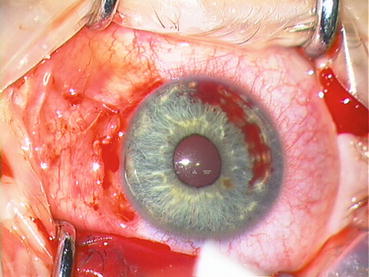
Fig. 26.26
Case report 21: limbal peritomy and Vicryl 8-0 cross suture on scleral defect. Caution: measure the location of the scleral defect with the caliper
A 19 y/o male patient was mowing the lawn when a foreign body hit his eye. Visual acuity was 1.0 and a scleral defect at 3 o’clock was discovered. A limbal peritomy was performed, the distance from the limbus to the scleral defect was 3.0 mm. A retinal damage was therefore not possible. The scleral defect was sutured with Vicryl 8-0. The foreign body was extracted 1 month later. See chapter “IOFB”.
Surgical Pearls No. 97
Measure the distance of the scleral defect from the limbus with a caliper. If the distance is longer than 4.0 mm, then a retinal defect is likely. Add in this case a retinal cryopexy.
Surgical Pearls No. 98
If the same scleral defect is located >4 mm behind the limbus, then perform a (blind) retinal cryopexy around the wound edges and, if you want to be absolutely safe, suture a silicone sponge above the scleral defect.
Surgical Pearls No. 99
Open globe injury: In case of a scleral defect posterior to the pars plana, measure with the caliper if unclear, and then schedule a vitrectomy 2 weeks after the primary closure; see Flow chart 26.1.
Flow chart 26.1
Our treatment algorithm for open globe injuries
26.5 Surgical Management of Aphakia and Distorted Pupil
Case Report No. 22: Aphakia and Distorted Pupil
Video 26.2: Iridoplasty and iris-claw IOL
Figures 26.27, 26.28, 26.29, 26.30, 26.31 and 26.32


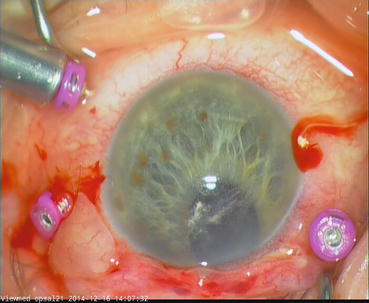
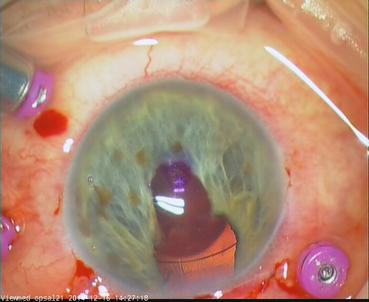
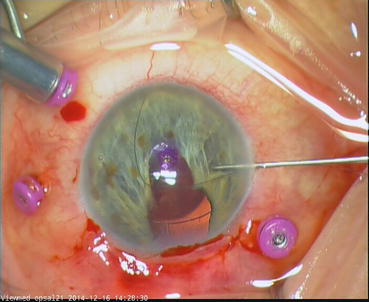


Fig. 26.27
Case report 22: perforating ocular injury with a tree branch

Fig. 26.28
Case report 22: old trauma which was operated with scleral suture and lens removal
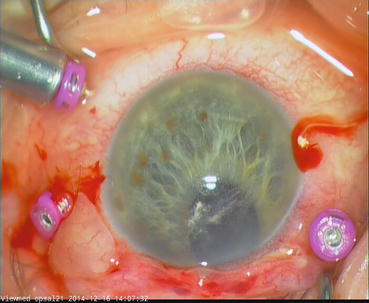
Fig. 26.29
Case report 22: staining of vitreous prolapse with triamcinolone
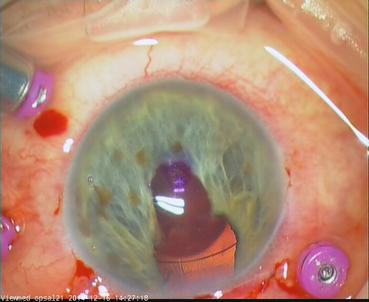
Fig. 26.30
Case report 22: retropupillar implantation of an iris-claw IOL (Verisyse®) and creation of a new pupil with the vitreous cutter
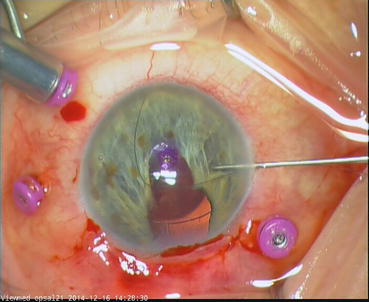
Fig. 26.31
Case report 22: iridoplasty with Hattenbach iris instruments (Geuder, Germany) and an Onatec suture (Geuder, Germany)

Fig. 26.32
Case report 22: closure of the iris defect
A 52 y/o male patient who experienced with the age of 17 years an open globe trauma to the left eye. He was operated with lens extraction and cryopexy. After surgery the pupil was distorted to 12 o’clock. He tried contact lenses for some time but did not tolerate them.
The eye is aphakic since 35 years and has an exotropia. The preoperative visual acuity was 0.1 without glasses and + 8.0sph = 0.6. The patient was admitted to us for a secondary IOL implantation. He was clearly informed that double vision may occur postoperatively. He was operated with iridoplasty, implantation of Verisyse IOL and creation of an artificial pupil. The visual acuity at second last follow-up was 0.3 and no double vision was present.
26.6 Surgical Management of a Traumatic Mydriasis with Suture Net
Case Report No. 23: Suture Net
Video: No video available
Figures 26.33, 26.34, 26.35, 26.36 and 26.37

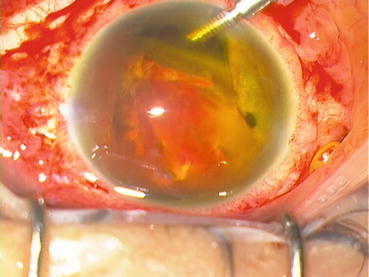
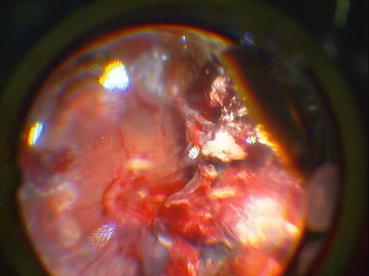
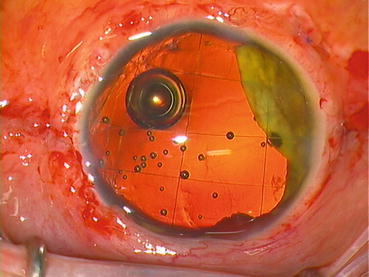

Fig. 26.33
Case report 23: this patient was playing ice hockey without protection when his eye was hit by the puck
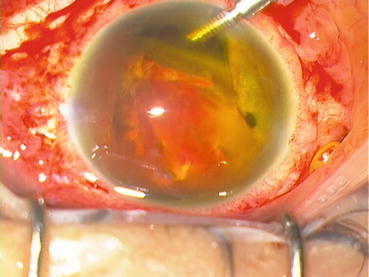
Fig. 26.34
Case report 23: a large scleral defect, dislocated nucleus and severe retinal injury
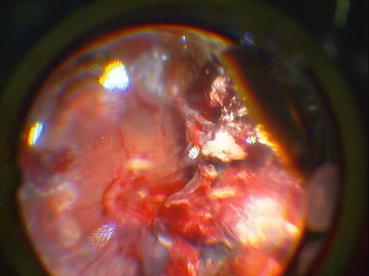
Fig. 26.35
Case report 23: after removal of the attached vitreous, the nasal retina could be reattached; the temporal retina was however severely damaged and difficult to distinguish from the choroid
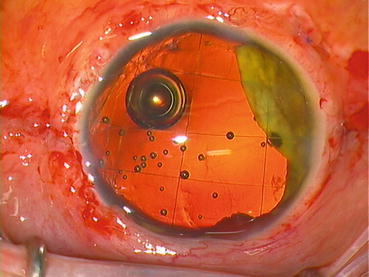
Fig. 26.36
Case report 23: a suture net with polypropylene 10-0 and a straight needle was applied to prevent a prolapse of the silicone oil into the anterior chamber
Fig. 26.37
Case report 23: a drawing of the suture. Start with 1 and end with 12; number 13 is the knot. One continuous suture
A 48-year-old male patient played ice hockey without a helmet just for fun. He stumbled and his eye was hit 20 cm above the ice by a hockey puck. He was admitted to us with a visual acuity of light perception. A scleral perforation at the limbus was sutured and 2 weeks later a vitrectomy was performed. The dislocated nucleus was removed with the vitrector. The vitreous body was still attached to the retina and also removed. A massive subretinal haemorrhage at the posterior pole was not removed. Due to the traumatic mydriasis, there was no natural barrier present to prevent the silicone oil to enter the anterior chamber. Therefore, a suture net with Ethilon 10-0 suture was applied. 5000 cSt silicone oil was used and should be preferred up to 1000 cSt silicone oil.
In the follow-up, the suture net functioned well; there was no silicone oil in the anterior chamber. After 3 months, the suture net had to be revised because fibrin distorted the net. After removal of the fibrin, the net regained its regular pattern.
26.7 Surgical Management of a Traumatic Aniridia and Aphakia with Iris and IOL Prosthesis
Figures 26.38 and 26.39



Fig. 26.38
An IOL–iris prosthesis from Ophtec, Netherlands. The diameter is 9 mm. A large incision is therefore required. The colour of the prosthesis turns out brighter when inserted in the eye. We use only the brown iris. The prize is approximately 500 Euros

Fig. 26.39
A hand-painted and foldable iris (without IOL) prosthesis from Human Optics, Germany. The diameter is 12 mm. The prize is approximately 2000 Euros
Eyes with mydriasis, aniridia and aphakia secondary to trauma can be provided with an iris prosthesis and an IOL prosthesis. The company Human Optics produces a foldable iris prosthesis, which is hand-painted. The companies Morcher and Ophtec produce iris and IOL prostheses. Morcher offers hand-painted iris prosthesis and Ophtec offers a range of four colours. Both prostheses from Morcher and Ophtec are PMMA and not foldable. The Morcher and Ophtec iris and IOL prostheses require a 9.0 mm broad main incision.
The iris prosthesis from Human Optics can be implanted with an IOL injector into the sulcus. For aniridia and aphakia, the iris prosthesis from Human Optics can be combined with a three-piece IOL: The iris prosthesis is fixated into the haptics of a three-piece IOL (MA60AC, Alcon). I call this a combo iris and IOL prosthesis. It is implanted through a 2.4 mm main incision with an IOL injector (Alcon).
There are several important features which determine the surgical planning:
1.
(Partial) aniridia
2.
Traumatic mydriasis
3.
Aphakia
4.
Intact lens capsule
Our surgical management is as follows:
1.
(Partial) Aniridia = > foldable iris prosthesis (Human Optics®)
2a.
Old traumatic mydriasis = > foldable iris prosthesis (Human Optics®)
2b.
Recent traumatic mydriasis = > iridoplasty with iris instruments (Geuder®, Germany)
3.




Aniridia and aphakia: = > combo iris and IOL prosthesis (Human Optics iris + three-piece IOL, Alcon)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


