Fig. 9.1
This is a slit lamp photograph of a failed graft after several repeat corneal transplants, which would be high risk for another standard penetrating keratoplasty
According to the WHO criteria, the patient should be either monocular or blind in both eyes. Although, more and more surgeons support the legitimacy of keratoprosthesis surgery despite intact vision in the contralateral eye, due to the potential for improved visual function, possible restoration of binocularity, and enhanced cosmesis in patients postoperatively (Aldave et al. 2009; Pineles et al. 2010). It has been previously believed that a candidate should have a minimum vision of light perception with projection in all four quadrants; yet, this notion has also been refuted by surgeons achieving excellent visual outcomes in patients with preoperative vision as good as 20/50 (Aldave et al. 2009). The patient should have no appreciable evidence of retinal or optic nerve dysfunction and no known history of dense amblyopia. To optimize outcomes, patients must have adequate lid anatomy and good blink function with no evidence of severe keratoconjunctivitis sicca.
Autoimmune disease (such as Stevens-Johnson syndrome (SJS) or ocular cicatricial pemphigoid (OCP)) had once been deemed a relative contraindication, due to their propensity for corneal melts (Colby and Koo 2011). More recently, advancements in postoperative management have expanded the realm of keratoprosthesis surgery to include these complicated patient populations (Colby and Koo 2011; Sayegh et al. 2008).
Prior to surgery, the patient must understand the need for indefinite postoperative prophylactic topical medications and must be committed to frequent follow-up visits. The procedure should be performed by a surgeon well experienced in penetrating keratoplasties, who has direct access to an eye bank, and a multidisciplinary ophthalmology team (glaucoma, retina, and oculoplastics specialists) (Aldave et al. 2009; Ament et al. 2009).
9.3 Design
The Boston type I keratoprosthesis is available for order from the Massachusetts Eye and Ear Infirmary (Boston). The threadless Boston type I keratoprosthesis consists of a central clear front plate and stem (manufactured from medical-grade polymethyl methacrylate, or PMMA), a corneal allograft button with the center trephinated and discarded, a large back plate, and a titanium locking ring (Fig. 9.2). The front plate is either 5 mm or 6 mm in diameter, with a smaller attached posterior stem that is segmented into three parts. The first segment of the stem, which accommodates the corneal graft, is 0.62 mm in height and 3.35 mm in diameter. The second segment, which accommodates the back plate, is 0.84 mm in height and 3 mm in diameter. There is a single-groove anterior to the innermost segment. The locking ring will eventually snap tightly into this furrow, and its dimensions are 0.33 mm in height and 2.74 mm in diameter.


Fig. 9.2
This photo displays the front plate, the PMMA and titanium 8.5 mm back plate options, and the locking ring of a Boston type I keratoprosthesis
The back plate is available in either PMMA or titanium. There are two size options for the diameter of the back plate: 7 mm or 8.5 mm. The smaller back plate has 8 holes, each 1.3 mm in diameter, and the larger back plate has 16 holes, each 1.17 mm in diameter. These holes allow the aqueous to deliver nutrition and hydration to the corneal graft to lessen the possibility of corneal melts (Harissi-Dagher et al. 2007). The back plate thickness is 0.8 mm centrally and 0.6 mm peripherally. Both types of back plates have a central 3 mm hole. The titanium locking ring has an outer diameter of 3.6 mm and an inner diameter of 2.8 mm with a uniform thickness of 0.23 mm (Harissi-Dagher and Dohlman 2007).
9.4 Surgical Procedure
The appropriate technique for the assembly and implantation of the Boston type I keratoprosthesis has been described (Dohlman et al. 2002). The host cornea should be examined carefully and calipers should be utilized to determine the size of the host trephination which will encompass the diseased cornea, without encroaching upon the anterior chamber angle. The donor cornea is trephinated in the usual fashion to be 8.0–9.0 mm in diameter, on average, so as to oversize the recipient bed by 0.25–0.5 mm. A 3 mm handheld dermatological punch is carefully centered over the endothelial side-up graft and twisted carefully with constant downward pressure, so as to leave behind a central hole. The 3 mm corneal button can be set aside and later discarded. The donor corneal donut is placed over the stem of the front plate, which is anterior side down on a sterile table, and gently pushed down into place. Viscoelastic may be applied to the endothelial surface of the donor cornea. The selection of the appropriate back plate is largely determined by the size of the host trephination created. For example, a smaller sized trephination would necessitate the 7 mm back plate, as it would be difficult to securely insert the 8.5 mm back plate with an 8 mm donor cornea into a host trephination of 7.5 or 7.75 mm. The selected back plate is then centered over the stem of the front plate and placed on top of the endothelial side of the donor cornea. No rotational movements are needed. Finally, the titanium locking ring is the last and most posterior component of the Boston type I keratoprosthesis. The locking ring, which clicks into place with downward pressure and the use of a hollowed pin that accompanies the set, should be placed so as to exactly fit the central stem of the front plate within the opening of the ring. The final composition should be examined to ensure the security of all components (Fig. 9.3).
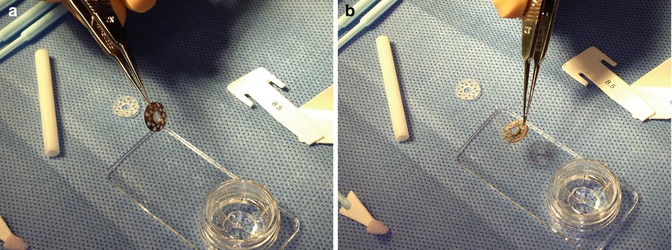
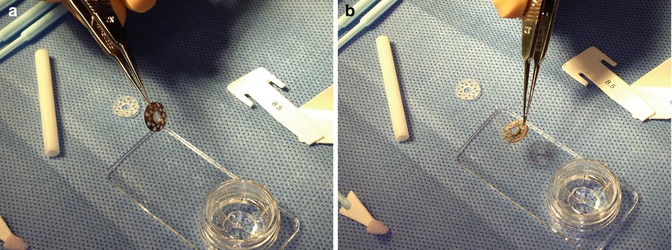
Fig. 9.3
This photograph demonstrates an anterior (left) and posterior (right) view of the final composition of the Boston type I keratoprosthesis, fastened into the donor cornea
The approach to the preparation of the recipient bed is not unlike that of a standard penetrating keratoplasty. The patient’s eye should be prepped in the usual sterile fashion for intraocular surgery. The recipient trephination should be 0.25–0.5 mm smaller than the selected diameter of the donor corneal button size. If the patient is phakic, a lensectomy must be performed. The posterior capsule should be preserved; yet, if the vitreous presents, then an anterior core vitrectomy should also be executed. Alternatively, if the patient is already pseudophakic with a posterior chamber intraocular lens, the lens implant may remain in place. It is imperative that the status of the lens be determined preoperatively, as the Boston type I keratoprosthesis must be ordered with the appropriate refractive power. If the patient is (or will be) aphakic at the time of transplantation, the axial length of the eye is needed in order to calculate the refractive power of the Boston type I keratoprosthesis. Multiple (12–16) interrupted 9-0 or 10-0 nylon sutures are passed through the corneal donor button portion of the apparatus to secure the Boston type I keratoprosthesis into the recipient bed with all knots buried, as would be done when performing a traditional penetrating keratoplasty. The graft–host junction should be inspected to be watertight. At the completion of the surgery, a plano soft contact lens (Kontur Kontact Lens Co., Hercules, CA) 16 mm diameter with 9.8 mm base curve is placed on the eye (Fig. 9.4).
Fig. 9.4
This slit lamp photograph shows the keratoprosthesis after implantation, along with the Kontur soft contact lens
9.5 Intraoperative Complications
Intraoperative complications, although rare, may happen. These events include vitreous loss, disassembly of the Boston type I keratoprosthesis components, anterior chamber bleeding, suprachoroidal hemorrhage, and perforation of thin host corneas (Zerbe et al. 2006; Aldave et al. 2009). It is imperative to remain cognizant of these possible occurrences and to always be prepared with a surgical approach to these intraoperative events should they spontaneously arise.
9.6 Postoperative Management
In the immediate postoperative period, the preferred antibiotic regimen recommendation includes a combination of topical fortified vancomycin (typically in a concentration of 15 or 25 mg/cc) and a fourth-generation fluoroquinolone, both one drop four times daily (Zerbe et al. 2006; Durand and Dohlman 2009). According to the International Boston Keratoprosthesis Protocol, an alternative acceptable course of therapy consists of a drop of chloramphenicol 1 % four times daily along with ciprofloxacin 0.3 % (or ofloxacin 0.3 %, levofloxacin 0.5 %, or moxifloxacin 0.5 % if available) four times daily (Ament et al. 2009). The topical antibiotics may be decreased to a maintenance dose of twice daily at postoperative month one, as patients with keratoprostheses must indefinitely administer prophylactic antibiotic drops (Ament et al. 2009). It is also recommended to instill one drop of povidone iodine 5 % once monthly at follow-up visits (Ament et al. 2009).
Perioperative or postoperative systemic steroids or immediate postoperative periocular steroids are utilized as preventive measure for intraocular inflammation and the development of retroprosthetic membranes (Zerbe et al. 2006; Ament et al. 2009) (Fig. 9.5a, b). After surgery, topical prednisolone 1 % should be dosed at one drop every two hours for 1 week, then four times daily for the remainder of the first month after surgery, and then slowly tapered over the next 1–3 months (Ament et al. 2009). Patients should remain on a maintenance dose of prednisolone one drop daily (Ament et al. 2009).
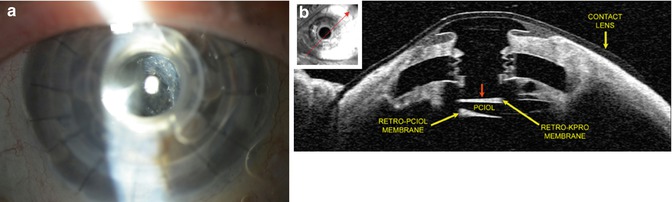
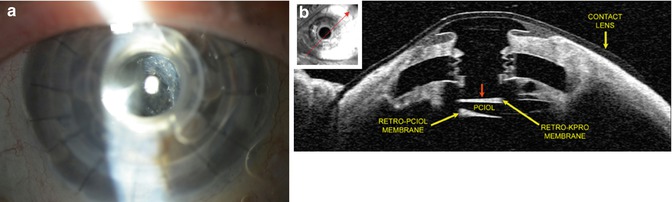
Fig. 9.5
(a) This is a slit lamp photo demonstrating a visually significant retroprosthetic membrane (RPM). (b) This anterior segment OCT of a different eye demonstrates another view of an RPM
Patients must keep a Kontur soft contact lens in the eye after surgery at all times. The primary purpose of this contact lens is to prevent drying of the ocular surface, which had led to dellen formation. Other functions served by this contact lens include increased patient comfort, general protection of the ocular surface, cosmesis and glare reduction (colored contact lenses), and correction of any residual refractive error (Harissi-Dagher et al. 2008). This contact lens should be exchanged for a new contact lens every 3–4 months, and the old lens should be cultured (Ament et al. 2009).
9.7 Visual Acuity Outcomes
Most patients evaluated to be candidates for a Boston type I keratoprosthesis have poor preoperative visual acuities. Visual potential is often difficult to assess, because of the inability to perform an adequate posterior exam due to the presence of severe corneal opacification.
As reported in the Multicenter Boston Type I Keratoprosthesis Study, which analyzed data from 136 eyes undergoing surgery to receive a Boston type I keratoprosthesis, only 3.6 % of patients had best-corrected visual acuity (BCVA) ≥20/200 before transplantation, with no eyes having BCVA >20/100. After an average follow-up of 8.5 months postoperatively, 57 % of eyes had BCVA ≥20/200, with 19 % achieving BCVA ≥20/40 (Zerbe et al. 2006). In another large series reported by Aldave et al., 100 % of eyes attained and maintained a visual acuity of ≥20/100 by 36 months of follow-up time. Even more encouraging, of patients who had a preoperative vision ≥20/50 in the contralateral eye, 47 % of eyes achieved a postoperative vision of ≥20/50 (Aldave et al. 2009).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


