Purpose
To evaluate the clinical features and outcomes of patients with recurrent corneal erosion syndrome who underwent anterior stromal puncture.
Study Design
Retrospective, nonrandomized, consecutive case series.
Methods
Database search of patients from 2003-2013 who underwent anterior stromal puncture was conducted at a tertiary care hospital cornea clinic. Charts of 30 patients (35 eyes) were reviewed. Outcome measures included demographics, laterality, history of corneal trauma, prior ocular history, frequency and duration of symptoms, failed treatments, signs on examination, degree of symptom resolution, additional treatments needed, and complications.
Results
Mean patient age at presentation was 37 (± 11.5 SD) years, 60% were male. A total of 83.3% of patients had unilateral and 16.7% had bilateral involvement. In all, 62.9% of eyes had prior history of corneal trauma and 2.9% had prior laser-assisted in situ keratomileusis. Ninety-seven percent of eyes had symptoms of pain upon awakening refractory to conservative treatment. In 97% of eyes, there were findings of microcysts, fingerprint lines, loose epithelium, and/or faint scars. Mean follow-up was 14 months (range: 3-120 months). At final follow-up, 62.9% of eyes were symptom free and 37.1% experienced milder episodes. Seventeen percent required additional treatment: 16.6% superficial keratectomy, 66% repeat anterior stromal puncture, and 16.7% phototherapeutic keratectomy. No complications were observed.
Conclusion
Anterior stromal puncture using a short (5/8 inch) 25 gauge bent needle is a simple, safe, and cost-effective procedure for symptomatic relief in patients with recurrent corneal erosion syndrome refractive to conservative measures. Repeat treatment may be performed prior to additional surgical intervention.
Recurrent corneal erosion syndrome is a disease characterized by repeated episodes of dislodgment of corneal epithelium from the underlying basement membrane because of loosened adhesion between the 2 layers. The first report was published in 1872 by Hansen, where he termed the condition “intermittent neuralgic vesicular keratitis.”
Recurrent corneal erosion syndrome may be either primary or secondary, depending on whether the defect in the epithelial basement membrane is intrinsic or acquired. Abnormalities of epithelial adhesion resulting in recurrent erosions can be associated with previous traumatic abrasions, with anterior corneal dystrophies (eg, map-dot fingerprint dystrophy, Reis-Bucklers, epithelial basement membrane dystrophy [EBMD]), or with degenerations (eg, anterior basement membrane degeneration). In the case of previous trauma, superficial injury to the cornea may cause damage to the epithelial basement membrane.
Patients suffering from recurrent corneal erosion syndrome often experience pain, photophobia, tearing, redness, and decreased vision, classically when they are awakened from sleep, because of friction exerted on the corneal epithelium. This painful attack can recur frequently, hence the name of the disease. Erosions occur along a spectrum; in some cases there is extensive loss of corneal epithelium accompanied by severe symptoms that may take several days to resolve. In other cases there is a small area of epithelial loss; this type of erosion occurs more frequently but is milder and of shorter duration.
There are many reported medical and surgical treatment modalities available for recurrent corneal erosion syndrome. Nonsurgical treatments include topical lubricating drops, gels, hypertonic saline and ointments, inhibitors of matrix metalloproteinase-9 such as doxycycline, corticosteroids, and autologous serum drops. Surgical intervention includes superficial keratectomy with or without a diamond burr, phototherapeutic keratectomy (PTK), and anterior stromal puncture with or without neodymium-doped yttrium-aluminum-garnet (Nd:YAG) laser.
In 1986, McLean and associates were the first to report on using the technique of anterior stromal puncture for patients with recurrent corneal erosion syndrome. The purpose of our study was to investigate the long-term clinical outcomes in a large series of patients with recurrent corneal erosion syndrome refractive to medical management who underwent anterior stromal puncture and to describe their clinical features. Reasons for treatment failure were also evaluated.
Patients and Methods
This retrospective observational case series was Research Ethics Board approved by the Toronto Western Hospital, University Health Network Institutional Review Board (IRB # 13-5976-BE). This study was conducted in compliance with the tenets of the Declaration of Helsinki.
Database search was conducted at a tertiary care hospital cornea clinic (Toronto Western Hospital, University Health Network, Toronto, Canada). Retrospective chart review was conducted for 30 patients (35 eyes) examined from January 2003 to August 2013 that underwent anterior stromal puncture for symptoms and signs of recurrent corneal erosion syndrome. Indication for intervention was symptoms of recurrent corneal erosion refractory to medical treatment. No patients were excluded from the analysis. Outcome measures included patient demographics, laterality, history of superficial corneal trauma, prior ocular history, frequency and duration of presenting symptoms, prior failed treatments, presenting signs on slit-lamp examination, degree of symptom resolution, additional treatments required after anterior stromal puncture, and intraoperative and postoperative complications.
Surgical Technique
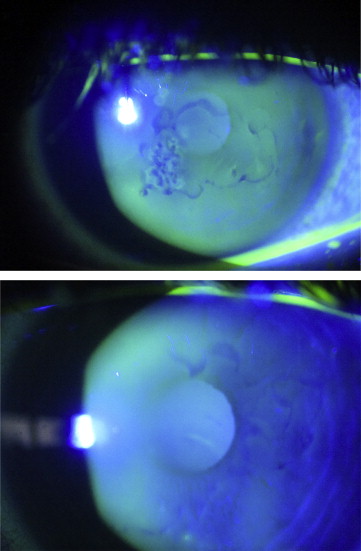
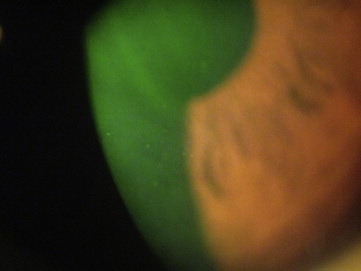
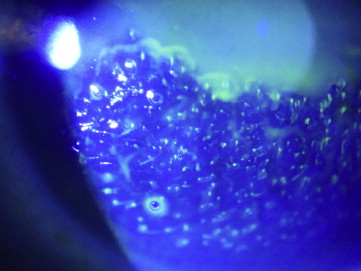
Anterior stromal puncture was performed with the patient sitting at the slit lamp. A few drops of topical anesthetic eye drops (eg, Proparacaine) were administered to the affected eye. The tip of a short (5/8 inch) 25 gauge needle, attached to a 1-mL syringe, was bent near the needle hub using the plastic needle cover, taking care not to dull the needle tip. A lid speculum was sometimes inserted depending on patient cooperation but was often unnecessary. The surgeon then held the syringe and would aim the needle tip 90 degrees to the corneal surface ( Figure 1 ) to gently indent the affected epithelium, creating micropunctures over the area that felt loose on contact. The vertical nature of needle entry created more consistent, small micropunctures as opposed to horizontal, wide scratches with tangential entry that would create a larger and potentially more visually significant scar. Sufficient pressure was needed such that resistance could be felt against the stroma at approximately 5%-10% stromal depth. The epithelium often felt poorly adherent to the Bowman layer on indentation in a focal area, but on occasion the complete corneal surface was abnormal, indicating that the patient likely had EBMD, a bilateral problem ( Figure 2 ), rather than posttraumatic recurrent corneal erosion syndrome ( Figure 3 ). Punctures were made less than 1 mm apart. Performing the procedure with fluorescein staining and under cobalt blue light allowed the surgeon to determine that adequate treatment was complete as bubbles could be visualized ( Figure 4 ). One could distinguish between subepithelial bubbles, which tended to be round, and the desired intrastromal air bubbles, which were more triangular, indicating that the needle tip had sufficiently “tickled” the stromal surface to allow for better epithelial adherence.

Immediately following the procedure, patients were given a drop of topical antibiotics and a bandage contact lens (BCL) was placed over the cornea. The patient was then discharged home with instructions to use a combination of antibiotic and steroid drop (eg, tobramycin 0.3%/dexamethasone 0.1%; Tobradex; Alcon, Fort Worth, Texas, USA) 4 times daily until follow-up at 1 week and then tapered over 1 month. The bandage contact lens was left in situ for at least an additional 6 weeks to allow for the epithelium and basement membrane to heal, and for reestablishment of tight adhesions of regenerated epithelium to Bowman layer. The BCL was replaced at the 1-week follow-up visit if it had debris on it. The patient’s second follow-up visit was usually 5 weeks later, at which time the BCL was removed. The patients were instructed to continue lubrication drops 4 times daily or more as needed (in that case, preservative-free drops) and to use ointment at night (either Muro128 or Lacrilube). Our patients reported high adherence to this treatment regimen, especially the ones that remained symptomatic after the first anterior stromal puncture procedure.
Results
Sixty percent of patients (18/30) were men, 40% (12/30) women. The mean age of patients was 37 (± 11.5 SD) years. A total of 83.3% of the patients (25/30) had unilateral involvement and 16.7% (5/30) had bilateral involvement. Of 35 eyes, 62.9% (22/35) had a prior history of trauma, 2.9% (1/35) had prior laser-assisted in situ keratomileusis (LASIK), 2.9% (1/35) had a known history of EBMD, and 31.4% (11/35) had symptoms consistent with recurrent erosion but had no prior ocular history of surgery, trauma, or other ocular comorbidities; these eyes were given a diagnosis of presumed EBMD. Ninety-seven percent of the eyes (34/35) had pain on awakening in the morning; 40% (14/35) had dry eye symptoms. In 97.1% of eyes (34/35) on slit-lamp examination, there were positive findings of microcysts, fingerprint lines, loose epithelium, and/or faint scars. One eye did not have positive findings on slit-lamp examination; however, this patient did experience recurrent episodes of pain on awakening in this eye and had epithelial basement membrane dystrophy findings in his fellow eye, and therefore he underwent anterior stromal puncture treatment in the symptomatic eye. All eyes were treated with anterior stromal puncture. The mean follow-up was 14 months (range of 3-120 months). Thirty-three percent of patients (10/30) had a minimum of 6 months follow-up and 23.3% (7/30) were followed for more than 12 months. Median duration of follow-up was 3 months.
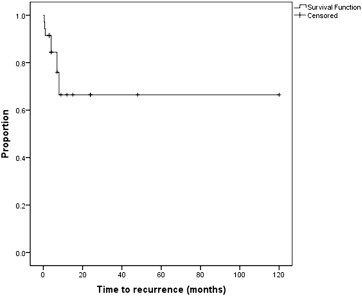
A total of 62.9% of eyes (22/35) were completely symptom free; 37.1% (13/35) suffered recurrent erosion episodes after anterior stromal puncture, but these episodes were reported to be milder. The patients in this group reported recurrent episodes of corneal erosion starting from a few days after the procedure (2 patients) to 6 months after the procedure ( Figure 5 ). Seventy-one percent of eyes (25/35) had signs of EBMD following the treatment. Seventeen percent of eyes (6/35) required additional treatment; from this group of 6 eyes that had an additional treatment, 1 eye had superficial keratectomy, 4 eyes had repeat anterior stromal puncture, and 1 eye had PTK. No adverse reactions such as haze or infections were observed during the follow-up period. None of the patients developed any dense central scarring that was visually significant.
Clinical features of the 6 eyes from 5 patients that had additional interventions after a single anterior stromal puncture treatment are listed in the Table . Two of the 5 patients that underwent repeat anterior stromal puncture had bilateral involvement. The fellow eye had milder symptoms that responded to medical treatment, excluding Patient 2, who had both eyes treated. Four of the 6 eyes that had repeat anterior stromal puncture had a history of trauma; 1 eye had a history of soft contact lens wear. Four of the 5 patients that had additional anterior stromal puncture treatment had resolution of their symptoms. One patient failed repeat anterior stromal puncture treatment because of persistent loose epithelium and thus elected for superficial keratectomy. He remained symptomatic at the time of this manuscript preparation and is contemplating PTK. The repeat treatments were performed between 2 weeks after anterior stromal puncture procedure and 11 months following the procedure.



