Chapter 17
ANTERIOR CHAMBER

The AC is the most anterior compartment of the eye; it is bordered by the cornea, the angle, the iris, and the lens and is filled with a completely transparent aqueous. Injury to the bordering structures and its implications are discussed in the appropriate chapters; here we cover issues related to synechiolysis and the removal from the AC of the following materials:
• blood;
• fibrin and inflammatory debris (including infectious organisms);
• lens (see also Chapter 21);
• vitreous;
• IOFBs (see also Chapter 24);
• air bubble(s); and
• viscous/viscoelastic material.
We also discuss methods of reformatting the AC.
SYNECHIALYSIS AND PUPILLARY MEMBRANES
Anterior synechiae represent iris tissue that is adherent to the cornea or the angle, typically to an area of a former traumatic or surgical wound. The synechia may interfere with vision, deform the pupil, even cause secondary glaucoma (see Chapter 20). Should such complications result, the synechia is best broken: it may be lysed by a sweeping motion using a spatula. Stronger connections require cutting by scissors or the vitrectomy probe. Viscoelastics are also useful. If the scar is vascularized, these may have to be diathermized first to avoid hemorrhage. Adequate attention must also be paid to avoiding damage to the endothelium and Descemet’s membrane. Especially following extensive injury, the scar may be too large and leaving it behind is preferable to causing iatrogenic damage. Rarely, a PK is required.
Posterior synechiae are usually the result of inflammation, “gluing” iris tissue onto the anterior lens capsule. This may cause pupil deformity and inability of the pupil to dilate; secondary glaucoma is much more common than in eyes with anterior adhesion.
PEARL… When breaking posterior synechiae, special attention is required if the lens is clear to avoid breaching the anterior capsule. Strong adhesions between the iris and the anterior lens capsule are therefore better broken with a spatula before viscoelastics are injected, thus avoiding both capsular damage and the entrapment of viscoelastics behind the iris.
If posterior segment surgery is needed, iris retractors may be inserteda to keep the pupil open when all synechiae have been broken.
HYPHEMA
Blood in the AC commonly accumulates in case of (closed as well as open) globe trauma. Consequences include IOP elevation, corneal blood staining, the formation of anterior/posterior synechiae, cataract, and a wide variety of indirectly related pathologic changes. Because traumatic hyphema may lead to a significant reduction in vision, all ophthalmologists must be comfortable with its diagnosis, evaluation, and management. We review the setting, pathophysiology, evaluation, and treatment of hyphema.1
Epidemiology and Prevention
• The estimated incidence rate in North American studies is 17–20/100,000 population/years.2,3
• The vast majority of patients are younger than 20 years of age.4
• The male/female ratio is approximately 3 to 1.
• The most common cause is a blunt object.4–11
• Sports are the source in 60% in the younger population.
The USEIR found that:
• 33% of all eyes with serious injury develop hyphema;
• the risk of hyphema is 31% in open globe and 35% in closed globe trauma;
• 46% of hyphemas occur in eyes with open globe trauma;
• 80% of those injured are males;
• the mean age of those injured is 29 years (median: 30 years).
| Grade | Hyphema Size | |
|---|---|---|
| I | < 1/3 | |
| II | 1/3–1/2 | |
| III | 1/2–near total | |
| IV | Total | |
| Microscopic* | Circulating RBCs only; no gross collection of blood |
*It is difficult to ascertain the true significance of microscopic hyphema because it is not always easy to differentiate it from traumatic iritis. However, as rebleeding may occur in approximately 7% of children with microscopic hyphema,10,11 even small amounts of blood in the AC need to be taken seriously and the patient followed closely.
Wearing proper eye protection (polycarbonate lenses with sturdy frames and posterior retaining lips) could significantly reduce traumatic hyphema.
Classification
Hyphema is graded according to the amount of blood in the AC (Table 17–1).2,4,5,12
Pathophysiology
Mechanism of Injury
Contusion causes anteroposterior globe compression with equatorial scleral expansion, limbal stretching, and posterior displacement of the lens/iris diaphragm. There is an acute IOP elevation, which may be associated with tissue damage in the angle (Fig. 17–1).13 Bleeding generally occurs from tears in the:
• major arterial circle and branches of the ciliary body;
• choroidal arteries;
• ciliary body veins13; and/or (less commonly)
• iris vessels at the pupillary margin or in the angle.
Associated Clinical Findings
• Angle recession. Common following closed globe trauma, it represents a separation between the longitudinal and circular fibers of the ciliary muscle.14
• Cyclodialysis cleft. An important cause of hypotony (see Chapter 19).
• Traumatic iritis, with inflammatory cells in the AC, always accompanies hyphema; the pigmentary changes may persist even after the blood has cleared. It is not uncommon to have focal zones of iris atrophy and pigment on the anterior capsule, sometimes in the form of a Vossius ring.7
• Miosis.
• Mydriasis. Occurs in approximately 10% of eyes.
• Iridodialysis. Occurs in approximately 10% of eyes.2,7
• Corneal changes. May range from minor abrasion to corneal endothelium damage and limbal rupture.
• Cataract. May be a late occurrence.
• Lens subluxation. Less common.
• Concentric rings of ocular tissues have been described as potentially damaged in closed globe trauma (Fig. 17–2).15
• The full spectrum of posterior segment injuriesb (vitreous hemorrhage, retinal edema/hemorrhages/ holes/tears, choroidal rupture etc.). Optic atrophy
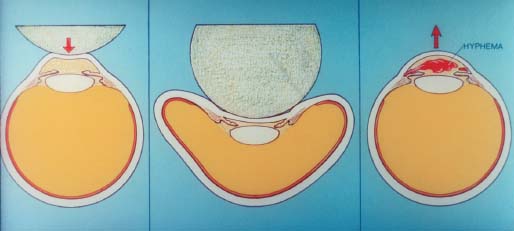
FIGURE 17–1 Mechanism of bleeding resulting from closed globe trauma to the eye: equatorial expansion with posterior displacement of lens/iris diaphragm and tearing of blood vessels. Adapted from Campbell DG. Traumatic glaucoma. In: Shingleton RJ, Hersh PS, Kenyon KR, eds. Eye TraumaSt. Louis: Mosby Year Book; 1991: 118, by permission from Mosby.
PEARL… Angle recession may be significant even in eyes with small hyphemas and is not necessarily correlated with the degree of acute IOP elevation.
Angle recession may occur in 85% of patients with traumatic hyphema235 and be associated with early as well as late onset of glaucoma (see Chapter 20).
may also occur, particularly in the setting of marked IOP elevation.2,7 Even a marginal pressure increase may be associated with significant optic atrophy in patients with sickle disease or sickle trait.
Clot Formation and Dissolution
IOP elevation, vascular spasm, and formation of a fibrin/platelet clot facilitate cessation of the bleeding.16,17 A pseudocapsule may develop with firm attachments to surrounding tissues. Blood may extend from the AC into the PC. Maximum clot integrity tends to occur 4–7 days after injury; fibroblastic activity is not seen at this stage.
PEARL… The AC is fibrinolytically active.18 Plasminogen (profibrinolysin) is converted to plasmin (fibrinolysin) by coagulation cascade activators. Plasmin, in turn, breaks down the fibrin, leading to clot dissolution. Clot degradation products, free blood cells, and inflammatory debris clear through trabecular meshwork outflow pathways and uveal scleral channels.19 Only minimal direct absorption through the iris vasculature occurs.
Evaluation
History
In addition to details of the eye injury’s occurrence, information should be sought on bleeding disorders, sickle cell disease, concurrent anticoagulant therapy, and systemic conditions such as pregnancy and kidney and liver disease, which may be affected by the medical treatment for hyphema. Always question the patient about preexisting ocular conditions (e.g., glaucoma) that may increase the risk of post-traumatic IOP elevation.
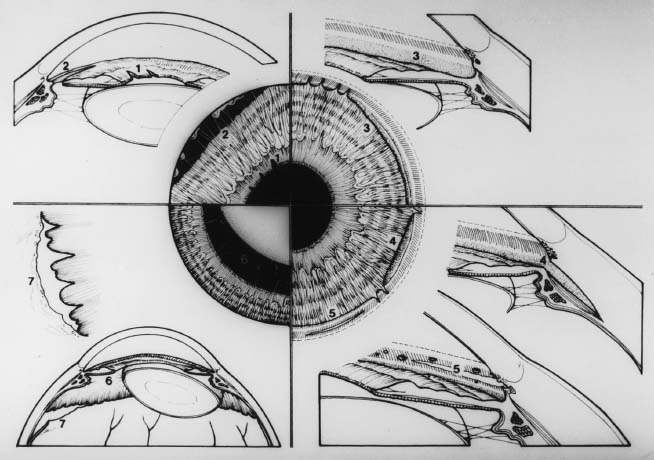
FIGURE 17–2 The seven typical anterior tears that occur following closed globe trauma to the eye. Clockwise from left: 1, Pupillary tears; 2, iridodialysis; 3, angle recession; 4, cyclodialysis; 5, meshwork tears; 6, ruptured zonules; 7, retinal dialysis. (From Campbell DG. Traumatic glaucoma. In: Shingleton RJ, Hersh PS, Kenyon KR, eds. Eye Trauma. St. Louis: Mosby Year Book; 1991:118. Reprinted by permission from Mosby.)
Clinical Examination
A complete eye examination is required for each case; suspect an open globe injury until confirmed otherwise. At all visits, the visual acuity, various tissue injuries, the hyphema’s extent, and the IOP need to be documented.
• The slit lamp should be used to describe carefully all details of blood accumulation. The clot must be differentiated from free, circulating red blood cells. The hyphema’s size may be described in three ways:/
 height (mm);
height (mm);
 grade (see Table 17–1); or
grade (see Table 17–1); or
 clock-hour extent.
clock-hour extent.
• IBO is indicated but the blood may hamper the view. We favor deferring scleral depression until 1 month after the trauma.
PEARL… High magnification with a narrow slit-lamp beam is the most effective way to detect the presence of corneal blood staining by demonstrating yellow granular changes in the posterior corneal stroma and reduced definition of the posterior stromal fibular structure of the cornea.
CONTROVERSY
Gonioscopy can be performed at the time of the initial injury if important information can be gained, for example, to document a site of active bleeding.
It is important not to compress the eye and exacerbate the bleeding. Gonioscopy should be performed in all patients 1 month after injury.
Ultrasonography
The USEIR (2000) found a rate similar to the HEIR’s: 57% of contused eyes with hyphema sustain damage to posterior segment structures. It is therefore crucial to evaluate the nature and extent of posterior segment injuries.
Laboratory Tests
All black and Hispanic patients with hyphema should have their sickle status examined19:
• sickle cell preparation;
• hemoglobin electrophoresis;
• bleeding tests (prothrombin time, partial thromboplastin time, platelet counts, and bleeding time); and
• kidney and liver functions (pending medical treatment decisions, e.g., whether systemic antifibrinolytics will be used).
PITFALL
Homozygotic patients (SS) and heterozygotic carriers (SA, SC) are predisposed to sickling and may be at significant risk.
Radiological Tests
Radiographic studies are not routinely obtained, although CT may be indicated if an IOFB, open globe injury, or orbital fracture is suspected.
Differential Diagnosis
Blood may collect in the AC even after trivial trauma in cases of:
• rubeosis iridis;
• malignant neoplasms;
• juvenile xanthogranuloma; or
• IOL (especially if AC or iris fixated).1
In addition to looking for abnormal clotting factors, occult (open globe) trauma must be considered in the differential diagnosis of “spontaneous” bleeding.
Treatment
Treatment Strategy
Medical and supportive treatment should be directed toward:
• reducing the rebleeding rate;
• clearing the hyphema;
• treating the associated tissue lesions; and
• minimizing the long-term sequelae.
Surgery is generally indicated for:
• IOP elevation not responding to medical treatment; and
• corneal blood staining.
The patient must be closely followed; sickle cell patients require more aggressive management and especially close observation.
The treatment protocols are highly varied and tend to be geographically and institutionally biased. It is important to avoid dogmatism and develop a reasonable, logical, and individualized approach.
Inpatient versus Outpatient Treatment
For the physician, there are advantages in hospitalization:
• ease of follow-up examination;
• increased compliance with medical therapy;
• a more “restful” environment; and
• earlier detection of complications.
Most patients, however, prefer treatment at home, which is also less expensive. In uncontrolled studies,20,21 no significant differences in rebleeding rates and clinical outcomes were noted in patients treated at home versus in a hospital.
Regardless of the site of therapy, the responsibility for adherence to the treatment program and follow-up care remains with the treating physician. Guidelines for medical and surgical management of traumatic hyphema is provided in Table 17–2.
Supportive Care includes the following.
• Moderate vs. strict bed rest: most reports22,23 found no significant outcome difference.
• Bilateral vs. unilateral patching: no difference in clinical results.24
• Reading restrictions: do not appear to be necessary.
• Sedation: rarely needed if activity is restricted to normal levels.
• Metal shield protection: usually indicated to prevent further damage to the eye in the first 5 days after injury.
• Elevation of the head of the bed: sedimentation of the blood facilitates posterior segment examination and visual recovery.
| Supportive care | Moderate activity; may sit and walk | |
| Elevate head of bed to 30° | ||
| Metal shield protection | ||
| Laboratory tests | CBC, PT, PTT, platelet count, BUN, creatinine, electrolytes, liver function tests as necessary | |
| Sickle cell prep, hemoglobin electrophoresis for patients at risk for sickle cell disease | ||
| Medications | Oral acetaminophen as needed | |
| No aspirin or NSAID | ||
| Atropine 1% 2X daily | ||
| Prednisolone acetate 1% 1 drop 4X daily; increase as necessary | ||
| Oral aminocaproic acid 50 mg/kg 4X daily up to 30 g/day for 5 days or prednisone 20 mg p. os 2X daily for high-risk patients | ||
| Surgery | Paracentesis and AC washout for IOP not responsive to medical therapy within 24 hours | |
| Other types of surgery as needed |
Medical Care A wide range of medicines have been proposed. Some of these treatments appear contradictory (e.g., miotics vs. cycloplegics; antifibrinolytics vs. fibrinolytics). Only a few of the recommendations have stood the test of time; these are reviewed in the following.
• Aspirin use has been reported to increase the rebleeding rate significantly in some,25–27 but not in other,28,29 studies. Most clinicians favor avoiding the antiplatelet effect of aspirin and the subsequent prolongation of bleeding time. This may also be an issue for nonsteroidal anti-inflammatory agents.
• Cycloplegics
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


