CHAPTER 10 Anesthesia for cataract surgery
Local anesthesia (LA) techniques
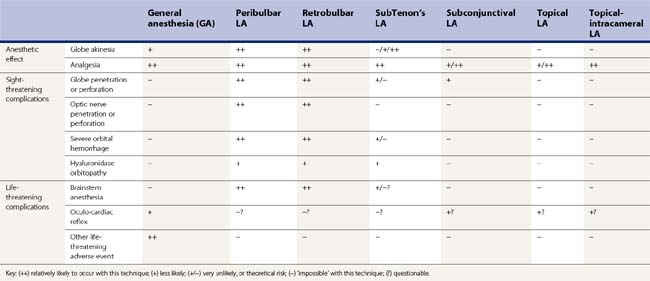
Several techniques of LA have been described for cataract surgery. There are three main categories: (i) sharp needle blocks (retrobulbar, peribulbar)1, (ii) blunt cannula blocks (subTenon’s)2, and (iii) minimal anesthesia (topical, topical-intracameral)3. These techniques are compared in Table 10.1. Other techniques have been described, including subconjunctival LA, and subTenon’s LA using a sharp needle. For any LA procedure, the patient should be warned what to expect beforehand. If sedation is not used, most patients find it reassuring to hold the hand of an assistant, who also monitors the patient during surgery. Guidelines for safe practice have been published4,5.
Sharp needle blocks
Retrobulbar and peribulbar LA injections1 (Figs 10.1, 10.2) give excellent akinesia and analgesia, although they are associated with sight-threatening and life-threatening complications. The needle may penetrate the globe or optic nerve, and this can result in blindness. Long myopic eyes, particularly those with a staphyloma, are at particular risk of this complication. If the needle penetrates the meninges around the optic nerve, the LA may enter the subdural space and track back to the brainstem; brainstem anesthesia may present with apnea, fitting, unstable blood pressure, and possibly death1,6. While these complications are rare, they are of course devastating. Therefore, it is recommended that these techniques are only used after suitable training, consideration of the anatomy and eyeball size/shape for each case, and with back-up available in case of an inadvertent brainstem injection1,4,5. Even in the best hands, these complications can occur with sharp needle blocks1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree