Minimally invasive alternatives for treatment of salivary duct obstruction are discussed. Radiologically- and endoscopically-guided interventions using wire baskets and dilating balloons, including cutting balloons, are covered as are combined endoscopic and open approaches.
Salivary duct obstruction alternative treatment overview
This article considers the radiologically and endoscopically guided management of benign salivary duct obstruction. Salivary stones and strictures account for most benign duct obstructions. Traditional management has fallen between the conservative approach (gland massage and review) and surgical lithectomy or sialadenectomy. Alternative treatments for these common causes of salivary obstruction have been sought to offer resolution of symptoms without extensive surgery or coexistence with long-term symptoms. Among these minimally invasive techniques, the per-ductal interventions, such as interventional sialography and sialendoscopy, have become firmly established, offering a solution that may be performed as a simple outpatient procedure under local anesthesia in selected cases.
Salivary duct strictures
Problems and Aims of Treatment
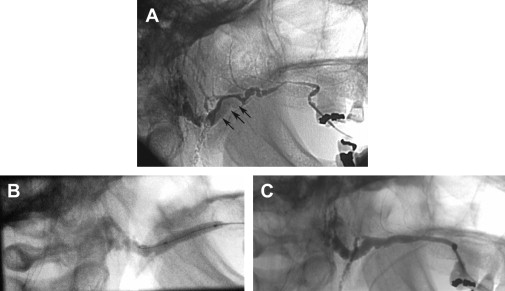
Strictures, most common in the parotid duct, can take several forms: approximately 66% of cases involve a single point lesion; around 33% are multiple point obstructions along the duct (known as sialadochitis) or a continuous band of fibrous tissue forming a diffuse stricture that may extend over a length of several millimeters. The morphology, number, and position of these strictures is best demonstrated by sialography. This imaging forms the basis for interventional treatment planning ( Fig. 1 ).
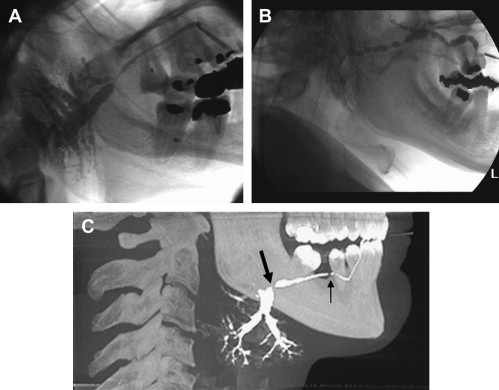
Sialography demonstrates that the common sites of parotid strictures are at the entry to the hilum of the parotid gland and the point where the duct curves over the anterior border of the masseter muscle to enter the oral cavity.
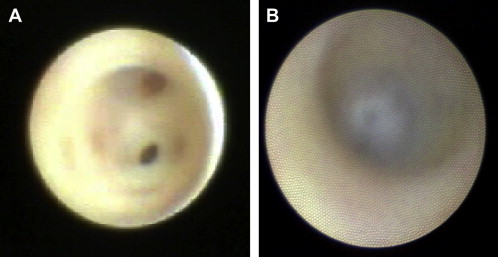
Endoscopic evidence suggests that evolving strictures, which probably equate to sialadochitis ( Fig. 1 B), commence as fibrous rings in the duct wall, giving it a similar appearance to the lumen of the trachea. Endoscopic examination of duct stenosis demonstrates a condensation of scar tissue within the duct wall giving it a pale, opaque, and avascular appearance ( Fig. 2 ).
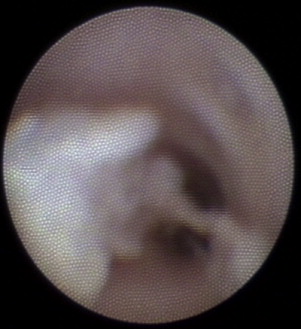
The clinical manifestation of obstruction is the mealtime syndrome (prandial swelling); but the clinical picture of salivary strictures is different from that of obstruction by a stone. Swelling of the gland does not always occur in relation to food intake; frequently, it is worse on waking, and the symptoms may develop over several days. Sometimes the swelling is released with a sudden gush of saliva. The scarred duct has a tendency to backfill and stagnant saliva has a tendency to gel, so that the ducts are seen to be filled with thick mucous plugs on endoscopic examination ( Fig. 3 ). Thus, the probable cause of acute obstruction is a plug washed forward and impacted into a stricture. With time and massage, the plug eventually squeezes through the stricture, followed by a surge of saliva. To minimize the risk of acute obstruction, a constant flow of saliva should be maintained by regular use of sialagogues (chewing gum), supported by regular gland massage. The aim of treatment, however, is to relieve stenosis and thus allow free outflow of saliva, preventing the formation of mucous plugs and allowing any that do form to be expelled readily.
Management of Salivary Strictures
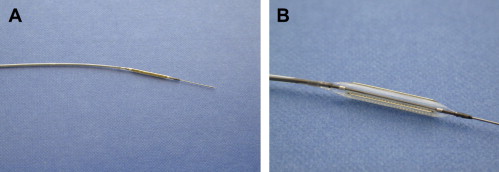
Acute obstructive symptoms can be managed by stricture dilation, which can take several forms. Modest strictures can be dilated by endoscopic irrigation. Point strictures can be released by cutting the fibrous band with a hand drill through an endoscope (PolyDiagnost GmbH, Pfaffenhofen, Germany), after which the lumen springs open. Established strictures (both point and diffuse) can be stretched by intraluminal balloon dilatation. Salivary balloon ductoplasty was first described in 1992 as a potential technique for the nonoperative elimination of benign salivary duct strictures. It has since become the most widely reported technique; several case reports and small case series agree on the benefits of this technique for relieving salivary duct stenosis without the problems of surgical intervention, particularly in the parotid gland where these are most common. This minimally invasive technique may be undertaken under radiological or endoscopic guidance and under local anesthesia. Radiological guidance requires a preoperative sialogram to localize the stricture, followed by insertion of the angioplasty balloon, using the fluoroscopic image to guide the balloon into the stricture before inflating it. A balloon slightly wider than the normal duct lumen is advised. A balloon with high inflation pressure or, alternatively, a cutting balloon, is advocated to release these dense fibrous strictures. Cutting balloons are a new technology and are constructed as conventional angioplasty balloon catheters, but with small microtome blades mounted along the length of the balloon itself. These blades are deployed as the balloon inflates, and are forced out into the vessel or duct wall to make minimal, superficial incisions across the surface of the band of stenotic tissue ( Fig. 4 ). The cutting balloon is a 2-cm long, 3.5F, 90-cm overall catheter, with typical inflation diameter of 2.5 mm. These balloons have been used in vascular and nonvascular interventional radiology as a more conservative and controlled way of incising through circumferential occlusions, and they have been found to reduce damage to vessel walls, yet achieve more precise relief from stenosis.
The technique is essentially the same when used with an endoscope, except that the balloon is positioned under direct vision, passed down the duct beside the endoscope, and forced forward through the stenosis. A postoperative sialogram is recommended to confirm successful elimination of the stricture ( Fig. 5 ).
Technique for radiologically guided balloon sialoplasty
The number and location of strictures is identified on a preoperative sialogram. Digital subtraction sialography is helpful in eliminating large dense superimposed objects, such as teeth and restorations. Local anesthesia may be obtained by infiltration along the anterior parotid duct and by per-ductal instillation of local anesthetic solution, such as 2% lidocaine. With radiographic contrast in situ in the duct and under fluoroscopic guidance, a 2-cm long angioplasty balloon, slightly wider than the desired duct diameter, is inserted over a hydrophilic guidewire that is passed along the main excretory duct. A parotid duct may be dilated with a balloon between 2.5 and 4 mm in diameter (when inflated), dependent on the degree of preexisting adjacent dilatation. The balloon catheter should ideally be on a reasonably rigid shaft to allow it to be pushed through tight proximal strictures, and it should reach pressures of at least 10 to 15 atmospheres on inflation (eg, Symmetry Stiff Shaft Balloon, Boston Scientific Corporation, Natick, MA, USA). Once manipulated into position within the most proximal stricture, the balloon is inflated rapidly, held in place for 2 minutes, and deflated. The procedure can be repeated to eliminate all identifiable strictures, working stepwise distally toward the duct orifice. This technique has the advantage of minimal instrumentation. It involves only the insertion of a 3F angioplasty balloon catheter into the duct, and it is therefore a minimally invasive procedure. The position of the catheter can be monitored throughout the procedure by fluoroscopy. A dense point stenosis may be difficult to dilate fully, and on inflation, the balloon (which is filled with radiopaque contrast media, visible on the radiographic image) shows a “waist” where it is indented by the tight stenosis. The stricture should be dilated repeatedly until it is eliminated. Here, cutting balloons have an advantage.
Technique for endoscopically guided balloon sialoplasty
Preoperative sialography is strongly recommended, even for sialendoscopy, to identify the presence and position of all stenoses and help plan the depth required for insertion of the sialendoscope. As discussed earlier, local anesthesia can be delivered incrementally through the endoscope. The duct orifice is dilated manually until the endoscope can be inserted and advanced to the first stricture. The stricture may respond to pressure applied directly to it by the tip of the endoscope; otherwise, an angioplasty balloon, placed in parallel with the endoscope, can be advanced through the stricture and inflated under direct vision. However, the duct needs to be wide enough to accommodate the combined width of the instruments. The balloon is carefully positioned within the tightest part of the stricture and may be inflated several times. The endoscope is advanced stepwise, treating each stricture as it is encountered, and working proximally toward the hilum of the gland. The process is thus the reverse of the radiologically guided technique.
Salivary duct strictures
Problems and Aims of Treatment
Strictures, most common in the parotid duct, can take several forms: approximately 66% of cases involve a single point lesion; around 33% are multiple point obstructions along the duct (known as sialadochitis) or a continuous band of fibrous tissue forming a diffuse stricture that may extend over a length of several millimeters. The morphology, number, and position of these strictures is best demonstrated by sialography. This imaging forms the basis for interventional treatment planning ( Fig. 1 ).
Sialography demonstrates that the common sites of parotid strictures are at the entry to the hilum of the parotid gland and the point where the duct curves over the anterior border of the masseter muscle to enter the oral cavity.
Endoscopic evidence suggests that evolving strictures, which probably equate to sialadochitis ( Fig. 1 B), commence as fibrous rings in the duct wall, giving it a similar appearance to the lumen of the trachea. Endoscopic examination of duct stenosis demonstrates a condensation of scar tissue within the duct wall giving it a pale, opaque, and avascular appearance ( Fig. 2 ).
The clinical manifestation of obstruction is the mealtime syndrome (prandial swelling); but the clinical picture of salivary strictures is different from that of obstruction by a stone. Swelling of the gland does not always occur in relation to food intake; frequently, it is worse on waking, and the symptoms may develop over several days. Sometimes the swelling is released with a sudden gush of saliva. The scarred duct has a tendency to backfill and stagnant saliva has a tendency to gel, so that the ducts are seen to be filled with thick mucous plugs on endoscopic examination ( Fig. 3 ). Thus, the probable cause of acute obstruction is a plug washed forward and impacted into a stricture. With time and massage, the plug eventually squeezes through the stricture, followed by a surge of saliva. To minimize the risk of acute obstruction, a constant flow of saliva should be maintained by regular use of sialagogues (chewing gum), supported by regular gland massage. The aim of treatment, however, is to relieve stenosis and thus allow free outflow of saliva, preventing the formation of mucous plugs and allowing any that do form to be expelled readily.




