Purpose
To evaluate agreement of flicker chronoscopy for structural glaucomatous progression detection and factors associated with progression.
Design
Retrospective cohort study.
Methods
Two glaucoma fellowship–trained ophthalmologists, masked to temporal sequence, independently graded serial flicker chronoscopy images from 1 eye of a cohort of glaucoma patients for features of structural progression. Agreement between graders was determined, as was accuracy for determining the temporal order of images. After adjudication, simple and multiple logistic models were constructed to determine baseline variables associated with increased odds of progression.
Results
Fifty of 103 included eyes/patients (48.5%) had at least 1 sign of structural progression. Temporal sequence was incorrectly determined in 14 of 206 cases (6.4%). Interobserver agreements for identifying baseline photographs (κ = 0.9), global progression (κ = 0.7), parapapillary atrophy (PPA) progression (κ = 0.7), disc hemorrhages (κ = 0.7), neuroretinal rim loss (κ = 0.5), and retinal nerve fiber layer (RNFL) loss (κ = 0.2) were calculated. Age was significantly associated with global (1.8; 1.3-2.6, P < .001) (odds ratio; 95% confidence interval, significance) and PPA progression (1.7; 1.2-2.4, P = .002). Lower corneal hysteresis was associated with global progression (0.78; 0.56-0.99, P = .049) and RNFL loss (0.5; 0.3-0.9, P = .02). Goldmann-correlated intraocular pressure (1.0, 0.7-1.4, P = .9), visual field mean deviation (1.0, 0.9-1.0, P = .2), and central corneal thickness (0.9, 0.8-1.0, P = .1) were not significantly associated with progression. On multivariable analysis, only age was associated with global progression (1.8; 1.2-2.5, P = .002).
Conclusion
Flicker chronoscopy demonstrated acceptable interobserver agreement in structural progression detection. Corneal hysteresis and age were both associated with progression, but age was the only significant factor on multivariable analysis.
Glaucoma is an irreversible optic neuropathy resulting from retinal ganglion cell death that leads to progressive visual field loss and blindness when uncontrolled. Large prospective glaucoma clinical trials have shown the benefit of early intraocular pressure (IOP)-lowering therapy, now the mainstay of glaucoma treatment. Elevated IOP is recognized as the only modifiable risk factor for glaucoma, and Goldmann applanation tonometry is the current clinical gold standard for IOP measurement. Goldmann applanation tonometry is based on the Imbert-Fick principle, which states that the pressure inside an ideal elastic, dry, thin-walled sphere is equal to the force necessary to flatten its surface divided by the area of flattening. Variations from this ideal in the form of thick or steep corneas result in an overestimation of true IOP, and thin or flat corneas may conversely underestimate IOP. These effects of central corneal thickness and corneal curvature on IOP measurements are well established. The advent of the Ocular Response Analyzer (Reichert Corp, Buffalo, New York, USA) has further enabled the in vivo measurement of additional corneal behavioral parameters such as corneal hysteresis. Recently, corneal hysteresis has been regarded to have a potential role as both an IOP correction factor and a surrogate marker of an individual’s susceptibility to glaucomatous optic neuropathy.
Structural changes in the optic nerve head and retinal nerve fiber layer (RNFL) may precede the development of glaucomatous visual field defects. Clinicians commonly use side-by-side comparisons of serial optic nerve head photographs to detect glaucomatous features such as neuroretinal rim loss, RNFL loss, disc hemorrhage, and parapapillary atrophy. However, the use of side-by-side photographic comparison to detect glaucomatous progression is unsatisfactory. In an investigation where 3 glaucoma specialists concurrently judged and reached a common consensus as to the presence of structural progression in pairs of photographs in side-by-side comparison, Jampel and associates reported that the temporal order of 40% of cases was determined incorrectly, implying improvement instead of progression. Flicker chronoscopy superimposes and aligns 2 optic nerve head photographs such that unchanged regions appear stable while the observer determines changes by perceiving motion. Automated flicker chronoscopy is no more time consuming than side-by-side optic nerve head photograph comparison, yet it has been shown to be more sensitive in the detection of disc hemorrhage, parapapillary atrophy, and global glaucomatous change, thus underlining its potential importance.
Any useful diagnostic modality requires a good level of interobserver agreement. In our study, we aimed to determine the level of interobserver agreement between subjective assessments of structural progression using flicker chronoscopy by independent graders to evaluate its suitability for clinical glaucoma management. We also sought to examine the relationship of corneal hysteresis and other patient characteristics with structural glaucomatous optic nerve progression as determined by flicker chronoscopy.
Methods
Approval for this retrospective cohort study was obtained from the Institutional Review Board at Weill Cornell Medical College (New York, New York, USA), and informed consent was obtained from all patients for their participation in this research. Corneal hysteresis measurements were obtained using the Ocular Response Analyzer machine (Reichert Corp, Buffalo, New York, USA) using a previously described protocol. A digital fundus camera (Topcon TRC50EX Retinal Camera; Topcon Co, Tokyo, Japan) operated by a single trained photographer was used to obtain optic nerve head photographs. Flicker images (1 baseline and 1 follow-up) were created from serial optic nerve head photographs using PerfectView software (Merge Eye Care Solutions [formerly OIS], Chicago, Illinois, USA), and full-screen images were viewed using 13-inch Apple MacbookPro display screens (Apple Inc, Palo Alto, California, USA). Reliable visual field tests had <25% fixation losses and <15% false-positive errors and false-negative errors (24-2 Swedish interactive threshold algorithm standard automated perimetry; Humphrey Field Analyzer II; Carl Zeiss Meditec Inc, Dublin, California, USA).
Individuals aged 18 years and above were considered for inclusion in this study. For inclusion, patients were required to have both ≥2 visual fields within 1 year and ≥2 optic disc photographs taken at least 1 year apart within the Department of Ophthalmology at Weill Cornell Medical College. Clinical patient data obtained from these patients included age, sex, central corneal thickness, corneal hysteresis, Goldmann-correlated IOP, and corneal compensated IOP. Eyes that had a history of corneal disease, keratorefractive surgery, amblyopia, traumatic eye injury, and conditions that compromised the morphology of the optic nerve head and parapapillary area (eg, retinal detachments, giant cell arteritis, chorioretinitis) were further excluded. When such occurrences occurred unilaterally, the normal contralateral eye was retained for inclusion in the study. If both eyes of a subject were eligible, 1 eye was randomly selected for inclusion.
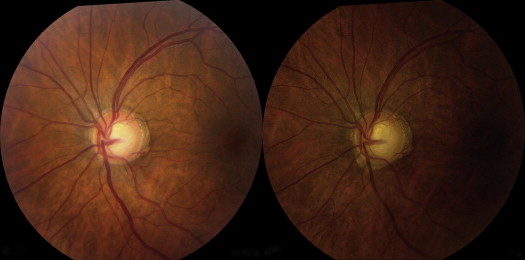
Pairs of baseline and follow-up images from each patient were randomized with respect to the order in which they were displayed for viewing as alternating flicker images, masking graders to the actual temporal sequence of images. Two glaucoma fellowship–trained ophthalmologists (F.S. and N.R.) independently graded images for evidence of structural glaucomatous change. Signs of structural progression assessed by the graders included neuroretinal rim loss, RNFL loss, disc hemorrhage, and parapapillary atrophy ( Figure 1 ; Supplemental Video 1 , available at AJO.com ) using previously defined criteria. Graders were instructed to note the presence of but disregard change attributable to parallax. Patients were deemed to have no structural progression if morphologic changes were absent or insufficient to determine the temporal order of images. Both graders determined the temporal order of images only in cases of progression. Each grader remained unaware of the other grader’s assessment prior to completing his or her personal assessment of the images. The 2 sets of results were then compared to determine the overall agreement between the subjective assessments of flicker images by the 2 masked, independent graders.
A following adjudication was performed where both graders simultaneously reassessed, discussed, and reached a consensus over the images of patients where there had been prior disagreement from independent individual grading. Both graders remained masked to the actual order of the baseline and follow-up images during the adjudication process. The data from the adjudication process were used to define progression and to determine various patient characteristics that were associated with glaucomatous progression.
Statistical analyses were conducted using Stata 11/IC (StataCorp LP, College Station, Texas, USA). Baseline variables were compared between patients with and without evidence of flicker progression using 2-sample t tests and the χ 2 test, as indicated. Interobserver agreement for various forms of progression was evaluated with the Cohen kappa coefficient. Simple and multiple logistic models were constructed to determine variables associated with increased odds of progression; multivariable models were constructed from univariable predictors with P < .2. All statistical tests were 2-sided, with a .05 level of significance.
Results
Of 407 individuals considered for inclusion, 115 patients met visual field and photographic inclusion criteria. Six additional patients had ophthalmic conditions that required the exclusion of both eyes. From these 109 remaining patients, 103 had baseline and follow-up optic nerve head photographs that were of sufficient quality for inclusion in the final group for flicker assessment of glaucomatous structural changes. Follow-up durations ranged from 12 to 74 months, with a mean of 31 months.
Interobserver agreement for features of structural progression in the 103 graded patients was assessed using the Cohen kappa test. Kappa values were classified as excellent, good, moderate, and slight according to the corresponding ranges as previously described by Viera and Garrett. There was excellent agreement (κ = 0.9) between both independent masked graders in identifying baseline photographs from pairs of flicker images based on structural progression. Good interobserver agreement (κ = 0.7) was seen for the detection of parapapillary atrophy progression, disc hemorrhage, and global progression (all variables included). Moderate agreement was observed for the identification of neuroretinal rim loss (κ = 0.5). The kappa value for the interobserver agreement of RNFL loss was 0.2 (slight). The overall rate whereby progression was determined in the wrong temporal order from independent grading was 6.4% (14/206) and 1.9% (2/103) after an adjudication that was masked to temporal sequence. After adjudication, 50 of 103 patients (48.5%) were determined to exhibit at least 1 sign of structural progression. Parallax was noted to be present in 50 of 103 pairs of flicker images (48.5%). The majority of cases of progression (30/50, or 60%) were noted to have no evidence of parallax.
Table 1 illustrates the patient demographics and variables that were compared between patients with and without structural progression. Analysis reveals that older patients (odds ratio [OR] = 1.8, 95% confidence interval [CI] 1.3-2.6, P < .001) and individuals with lower corneal hysteresis (OR = 0.78, 95% CI 0.56-0.99, P = .049) had a greater likelihood of progression. No significant associations with overall progression were revealed for sex (OR = 1.3, 95% CI 0.6-2.9, P = .5), central corneal thickness (OR = 0.9, 95% CI 0.8-1.0, P = .1), Goldmann-correlated IOP (OR = 1.0, 95% CI 0.7-1.4, P = .9), corneal compensated IOP (OR = 1.1, 95% CI 0.7-1.8, P = .6), and visual field mean deviation (OR = 1.0, 95% CI 0.9-1.0, P = .2).
| Variable | 2-Sample t Test/χ 2 Test | Strength of Association | ||||
|---|---|---|---|---|---|---|
| No Progression (n = 53) | Progression (n = 50) | P Value | OR | 95% CI | P Value | |
| Age (y) | 58.3 ± 14.6 a | 67.6 ± 10.0 a | < .001 | 1.8 | 1.3, 2.6 | < .001 |
| Sex (% female) c | 67.9% b | 62.0% b | .5 | 1.3 | 0.6, 2.9 | .5 |
| CH (mm Hg) | 9.6 ± 1.5 a | 9.0 ± 1.4 a | .04 | 0.7 | 0.56, 0.99 | .049 |
| CCT (μm) | 548.6 ± 33.6 a | 535.8 ± 44.8 a | .1 | 0.9 | 0.8, 1.0 | .1 |
| IOPg (mm Hg) | 15.8 ± 4.8 a | 15.6 ± 5.3 a | .9 | 1.0 | 0.7, 1.4 | .9 |
| IOPcc (mm Hg) | 17.1 ± 4.4 a | 17.6 ± 4.5 a | .6 | 1.1 | 0.7, 1.8 | .6 |
| Mean deviation (dB) | −4.5 ± 6.6 a | −6.4 ± 7.8 a | .2 | 1.0 | 0.9, 1.0 | .2 |
a 2-sample t test (mean ± SD).
We subsequently analyzed each parameter of structural progression to determine significant associations with clinical variables ( Table 2 ). No variables were significantly associated with disc hemorrhage or neuroretinal rim loss specifically. Parapapillary atrophy progression was significantly associated only with age (OR = 1.7, 95% CI 1.2-2.4, P = .002), whereas RNFL loss was significantly associated with lower corneal hysteresis (OR = 0.5, 95% CI 0.3-0.9, P = .02) and lower central corneal thickness (OR = 0.8, 95% CI 0.6-0.9, P = .01). Age was the only association that remained significant on multivariable analysis (OR = 1.8; 95% CI 1.2-2.5, P = .002) ( Table 3 ).
| Variable | PPA Progression | RNFL Loss | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P Value | OR | 95% CI | P Value | |
| Age (y) | 1.7 | 1.2, 2.4 | .002 | 1.0 | 1.0, 1.1 | .4 |
| Sex (% female) a | 1.7 | 0.7, 3.8 | .2 | 1.3 | 0.3, 4.8 | .7 |
| CH (mm Hg) | 0.8 | 0.6, 1.1 | .2 | 0.5 | 0.3, 0.9 | .02 |
| CCT (μm) | 1.0 | 0.9, 1.1 | .4 | 0.8 | 0.6, 0.9 | .01 |
| IOPg (mm Hg) | 1.0 | 0.9, 1.1 | .7 | 0.9 | 0.4, 1.7 | .7 |
| IOPcc (mm Hg) | 1.2 | 0.8, 1.9 | .4 | 1.2 | 0.6, 2.4 | .7 |
| Mean deviation (dB) | 1.0 | 0.9, 1.0 | .2 | 0.9 | 0.9, 1.0 | .2 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


