This article presents and discusses advanced minimally invasive sialoendoscopy and combined methods: endoscopy, endoscopic-assisted techniques, and external-lithotripsy combined procedures. It also presents rare situations and complications encountered during sialoendoscopic procedures. Sialoendoscopy is a relatively novel technique, which adds significant new dimensions to the surgeon’s armamentarium for management of inflammatory salivary gland diseases. Because of the rapid development in minimally invasive surgical techniques, surgeons are capable of more facilely treating complicated inflammatory and obstructive conditions of the salivary glands.
Obstructive sialadenitis, with or without sialolithiasis, represents the most common inflammatory disorder of the major salivary glands. Sialolithiasis is one of the major causes of sialadenitis. Calculi in the salivary glands can be found in 1.2% of the general population. Other common salivary gland pathologies (besides tumors) are sialadenitis, strictures, and kinks. The diagnosis and treatment of this problem has been traditionally hampered by limitations of the standard imaging techniques. Satisfactory management depends on the surgeon’s ability to reach a precise anatomic diagnosis and, in the case of sialoliths, to most accurately locate the obstruction.
Traditionally, sialoliths in the submandibular or parotid ducts and glands were divided into two groups : stones that can be removed by the intraoral sialolithotomy approach, located usually in the anterior part of the duct; and stones that cannot be removed by the intraoral approach necessitating extirpation of the entire gland (sialadenectomy). Another pathology that required gland removal was concurrent or recurrent sialadenitis.
Why minimally invasive procedures for the treatment of sialolithiasis?
The morbidity following traditional surgery for parotid and submandibular sialadenectomy includes a number of complications. Neurologic damage following superficial parotidectomy is of primary concern, because between 16% and 38% cases suffer temporary nerve weakness and 9% suffer permanent damage. During submandibular gland removal there is a 7% risk of permanent marginal mandibular nerve damage and a 3% risk of damage to the lingual nerve. Frey syndrome, facial scarring, greater auricular nerve numbness, sialocoeles, and salivary fistula also contribute to the morbidity of the traditional procedure.
During the past decade, rapid developments in medical technology, such as optical miniaturization, lithotripsy equipment, microinstruments, and the influence from other surgical specialties, pushed development of new methods of analogous noninvasive and minimally invasive treatment. Although it is possible to successfully treat salivary stones with traditional techniques, the use of the new methods was applied to advanced ductal cases. Because of the innovations, a surgeon became able to solve more complicated cases without major surgery and to perform the cases with less morbidity assuming the return of the gland to function.
The endoscopic system armamentarium requires an endoscope with at least 6000 pixels, a focal depth of 2 to 15 mm, and at least a 70° wide field of view. The diameter of one endoscope system (Modular Salivascope; PolyDiagnost, Pfaffenhofen, Germany) is 0.5 mm and uses four different disposable sleeves: 0.9, 1.1, 1.6, and 2 mm ( Fig. 1 A–C). The 0.9-mm sleeve has an irrigation channel and port for the telescope and is designed only for diagnostic purposes. The 1.1-mm system has three channels for the telescope, irrigation, and a special channel for surgical instruments. The 1.6- and 2-mm have the same number of channels but can accommodate large-size instruments to the working channel. The optical part, the telescope, is autoclavable. Other endoscope models offered for advanced cases are Polydiagnost Salivascope flex, Type PD ZS 2001 1.1 mm (PolyDiagnost, Pfaffenhofen, Germany); Sialoview MDI 1.1 mm (Millennium, Islandia, New York); and Erlangen model (Karl Storz, Tuttlingen, Germany).
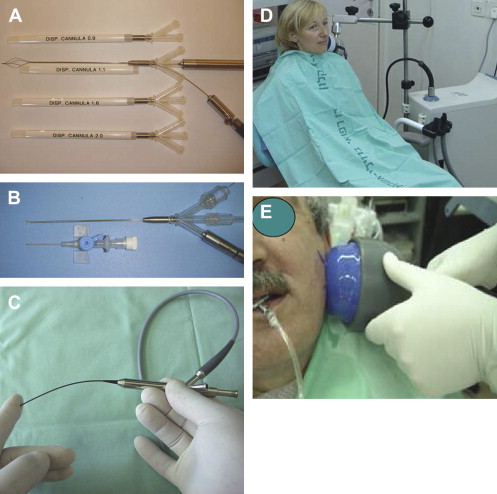
The endoscopic systems used in the author’s study were the Modular Salivascope (PolyDiagnost, Pfaffenhofen, Germany); Polydiagnost Salivascope flex, Type PD ZS 2001 1.1 mm (PolyDiagnost, Pfaffenhofen, Germany); and the Sialoview MDI 1.1 mm (Millennium, Islandia, New York). The instruments used in his studies were microbaskets, miniforceps, minibiopsy forceps, high-pressure balloons, and microdrills for dilatation; brushes for cytology; and microneedles for injection (PolyDiagnost, Pfaffenhofen, Germany; and Sialotechnology, Ashkelon, Israel).
Recently, a miniature extracorporeal shock wave lithotriptor (ESWL) (Sialotechnology, Ashkelon, Israel) ( Fig. 1 D, E) was developed to assist in sialolithiasis management. It has a miniature generator and applicator, focal point depth of 15 × 15 × 25 mm, large focus zone at 50% of 35 mm, and a penetration depth of 120 mm. The size of the generator is 52 cm height × 42 cm length (20 kg weight) and the working head is reduced to fit the dimensions of the head and neck region. The usual technique delivers 1000 to 1500 shock waves per session. The miniature lithotripter can use an ultrasonic aiming system, or can be directed to the stone using endoscopic identification with the transillumination effect and also clinical findings.
This article assesses the value of and strategies for using the multitude of newly developed instruments and combinations of use, such as lithotripsy-sialoendoscopy methods, for advanced salivary gland sialolithiasis cases.
Advanced techniques for advanced cases
When to Use Combined ESWL and Endoscopic Techniques?
In the past 2 years, 94 patients (43 males and 51 females, aged from 6–87 years) have been enrolled into the combined treatment. Sixty had pathology of the submandibular gland and 34 had pathology of the parotid gland.
Inclusion criteria for submandibular gland cases were (1) small (<5 mm) stone in secondary ducts or intraparenchymal stone (14 patients were selected); (2) small (<5 mm) fixed stone in the main duct in the hilus region (20 patients were selected); and (3) medium to large (>5 mm) hilar stone attached to the surrounding tissue, immobile or difficult to palpate (26 patients were selected).
Inclusion criteria for parotid gland cases were (1) small (<5 mm) stone in the main or secondary duct proximal from the middle part of the duct (eight patients were selected); (2) small (<5 mm) stone in secondary ducts or intraparenchymal stone (11 patients were selected); and (3) medium to large (>5 mm) hilar stone attached to the surrounding tissue, immobile or difficult to palpate (15 patients were selected). Exclusion criteria (same for both locations) were small (<5 mm) mobile stones in the main duct and medium to large (>5 mm) hilar mobile palpable stone.
Surgical Approach
Ultrasound and endoscopy assisted in location of the stone. The endoscope was then used to instill the salivary gland with lidocaine 2%. Lidocaine helps to numb the entire gland and the subsequent isotonic saline inflation is needed to protect the salivary parenchyma. In all patients, external lithotripsy was first applied at low energy levels up to 130 atm with 1000 to 1500 shockwaves for each session. Three sessions of ESWL per patient are usually administered with 1-month interval between each session.
Following lithotripsy, an assessment is made to determine the outcome using plain radiograph, sialogram, ultrasound, CT, or sialoendoscopy. Thereafter, a purely endoscopic procedure or endoscopy-assisted open approach is chosen to finish treatment of the stones. Three types of treatment might be performed: (1) lithotripsy; (2) lithotripsy plus intraductal endoscopic approach (pure endoscopy); and (3) lithotripsy plus endoscopic-assisted extraductal open approach (stretching procedure for submandibular stones or extraoral approach for parotid stones). The second and third methods are used in cases when a salivary stone is not eliminated by lithotripsy alone.
Advanced techniques for advanced cases
When to Use Combined ESWL and Endoscopic Techniques?
In the past 2 years, 94 patients (43 males and 51 females, aged from 6–87 years) have been enrolled into the combined treatment. Sixty had pathology of the submandibular gland and 34 had pathology of the parotid gland.
Inclusion criteria for submandibular gland cases were (1) small (<5 mm) stone in secondary ducts or intraparenchymal stone (14 patients were selected); (2) small (<5 mm) fixed stone in the main duct in the hilus region (20 patients were selected); and (3) medium to large (>5 mm) hilar stone attached to the surrounding tissue, immobile or difficult to palpate (26 patients were selected).
Inclusion criteria for parotid gland cases were (1) small (<5 mm) stone in the main or secondary duct proximal from the middle part of the duct (eight patients were selected); (2) small (<5 mm) stone in secondary ducts or intraparenchymal stone (11 patients were selected); and (3) medium to large (>5 mm) hilar stone attached to the surrounding tissue, immobile or difficult to palpate (15 patients were selected). Exclusion criteria (same for both locations) were small (<5 mm) mobile stones in the main duct and medium to large (>5 mm) hilar mobile palpable stone.
Surgical Approach
Ultrasound and endoscopy assisted in location of the stone. The endoscope was then used to instill the salivary gland with lidocaine 2%. Lidocaine helps to numb the entire gland and the subsequent isotonic saline inflation is needed to protect the salivary parenchyma. In all patients, external lithotripsy was first applied at low energy levels up to 130 atm with 1000 to 1500 shockwaves for each session. Three sessions of ESWL per patient are usually administered with 1-month interval between each session.
Following lithotripsy, an assessment is made to determine the outcome using plain radiograph, sialogram, ultrasound, CT, or sialoendoscopy. Thereafter, a purely endoscopic procedure or endoscopy-assisted open approach is chosen to finish treatment of the stones. Three types of treatment might be performed: (1) lithotripsy; (2) lithotripsy plus intraductal endoscopic approach (pure endoscopy); and (3) lithotripsy plus endoscopic-assisted extraductal open approach (stretching procedure for submandibular stones or extraoral approach for parotid stones). The second and third methods are used in cases when a salivary stone is not eliminated by lithotripsy alone.
Case presentations
Lithotripsy (Sole Treatment)
A 45-year-old woman failed attempt in removal of a right submandibular stone using sialoendoscopy. The patient had suffered from multiple swellings of the right submandibular gland for 5 years. Panorex (Morita, Tokyo, Japan) radiograph demonstrated a 5-mm stone in the hilum region, which was difficult to palpate and which was attached to the surrounding tissues. Endoscopic exploration could not demonstrate the stone in the ductal system so the diagnosis of an intraparenchymal stone in the hilum region was made ( Fig. 2 A).
ESWL with the miniature lithotripter was applied with low energy levels up to 130 atm. A total of 1000 shockwaves per session was administrated for three sessions with a month interval between. Following the third session, the stone was still clinically palpable and the patient was to be scheduled for an endoscopic-assisted extraductal approach. Just before the endoscopic procedure, however, a sialogram was performed and surprisingly it demonstrated exfoliation of the stone, which was very easily removed by massage of the gland (see Fig. 2 B, C). Endoscopic exploration following the removal of the stone showed dilated ducts but no additional stones or strictures were noted. In follow-up for over 16 months the gland remained asymptomatic and secretion of clear saliva could be noticed from the gland orifice.
Lithotripsy Plus Intraductal Endoscopic Approach (Purely Endoscopy)
A 62-year-old man had a sialolith of the left parotid gland. Clinical examination revealed swelling of the left parotid gland with purulent secretion from the left Stensen duct ( Fig. 3 A). Facial CT demonstrated a 4-mm stone located in the right parotid hilum ( Fig. 3 B). Endoscopic diagnostic exploration of the gland revealed the same 4-mm stone located in secondary duct without any possibility to reach the stone endoscopically.
ESWL with the miniature lithotripter was applied with low energy levels up to 130 atm. A total of 1000 shockwaves per session was administered for three sessions with a month interval between. Following the third session the stone was located with CT scan in the anterior third of the Stensen duct ( Fig. 3 C). Endoscopic removal of the stone was carried out under local anesthesia using a four-wire basket ( Fig. 3 D). Sialodrain (Sialotechnology, Ashkelon, Israel) was introduced into the duct for 1 month. During a 12-month follow-up, the gland was asymptomatic and secretion of clear saliva could be noticed from the duct orifice.
Lithotripsy Plus Endoscopic-Assisted Extraductal Open Approach (Submandibular Stretching Procedure)
A 45-year-old man presented a deep left submandibular stone. The patient suffered from multiple episodes of swelling. Clinical evaluation revealed a very deep stone located inside the gland and fixed to the surrounding inflamed tissues. Imaging including Panorex, sialogram, and CT scan demonstrated a round 7-mm stone extraductally compressing the Wharton duct ( Fig. 4 A–C). Endoscopic exploration of the Wharton duct revealed the stone to be posterior to the hilar region in one of the secondary branches of the duct. Only the upper part of the stone could be observed (the tip of an iceberg); the main part of the stone was located inside the salivary parenchyma ( Fig. 4 D).
Three sessions of ESWL were administrated with 1000 shock waves per session at low energy levels up to 130 atm. After the third session, the stone was better palpated and seemed to be mobile. Under local anesthesia, a diagnostic endoscopy demonstrated the stone within the main duct but because of the narrow diameter of the duct it was not possible to use the intraductal approach. Endoscopic assistant technique (stretching technique) was indicated and the stone was removed ( Fig. 4 E, F). Sialoendoscopic exploration following the sialolithtomy revealed a small sialolith in the secondary duct and a stricture posterior to the stone. The stone was retrieved with the aid of a microbasket and the stricture dilated with a microdrill and a high-pressure balloon ( Fig. 4 G–I). Sialodrain was inserted for 1 month. Follow-up 8 months later revealed an asymptomatic gland with a clear salivary secretion.
Lithotripsy Plus Endoscopic-Assisted Extraoral Approach
A 52-year-old man had a long-standing swelling of his left parotid gland. The patient suffered from multiple episodes of swelling and was hospitalized three times for IV antibiotic treatment and drainage.
CT demonstrated two stones ( Figs. 4 J–N) in the left parotid gland, the first stone located in the hilar region and the second stone located anterior to this region. The duct was totally obstructed in the anterior part to the second stone. Two attempts for endoscopic stone removal were unsuccessfully performed at another clinic.
On physical examination, a hard swelling of the left parotid region was noticed from the retroauricular region to the middle cheek area. Intraoral examination revealed complete obstruction of the Stensen duct, located a few millimeters posterior to the orifice. The patient was scheduled for superficial parotidectomy at another hospital.
Three sessions of ESWL were administrated with miniature lithotripter. Following the third session of lithotripsy there was a remarked reduction of the swelling in the parotid region. The patient was scheduled for sialolithotomy by external open parotid approach.
Under general anesthesia, the hilar stone was located with the aid of ultrasound and was marked with biopsy marker and injection of methylene blue into the stone location ( Fig. 4 K). By way of a rhytidectomy approach the first stone in the hilar region was explored and removed with the aid of a small dental excavator ( Fig. 4 L). Following the removal of this stone, a Salivascope flex, 1.1 mm, was inserted from the previous stone location to locate the anterior stone. The second stone was located and removed with the aid of the endoscope using the transillumination effect ( Fig. 4 M).
The next step was to create a new ductal opening to the gland. An 18-gauge veinline was inserted from the location of the second stone toward the mouth into the original location of the Stensen duct.
Parotid duct drain (Sialotechnology, Ashkelon, Israel) was inserted from the mouth with the aid of the veinline toward the location of the hilar region. The drain was fixed with 3/0 Vicryl sutures to the cheek mucosa and the incisions of the stones’ regions were sutured thoroughly with 4/0 Vicryl sutures. The rhytidectomy flap was sutured with 5/0 nylon ( Fig. 4 N). Pressure dressing was applied for 24 hours. After 4 weeks, the parotid duct drain was removed. Follow-up 3 months later revealed an asymptomatic and normally functioning gland. The cosmetic result was satisfactory.
Lithotripsy Plus Endoscopic-Assisted Extraductal Open Approach for Giant Stones
A 68-year-old woman had constant swelling of her right submandibular gland. On physical examination, a large, hard swelling was detected, fixed to the surrounding tissues. Lateral radiographs demonstrated exceptionally significant stone occupying the location of the submandibular gland ( Fig. 5 A).




