This article focuses on the facial nerve with additional comments on the recurrent laryngeal nerve as a proxy for the lower cranial nerves. Methods, advantages and disadvantages, and techniques are listed. The article addresses the anatomy of the facial nerve, discusses neurophysiologic testing, the role of electroneurography in preoperative, intraoperative, and postoperative testing, and presents 7 steps to set up for and perform facial nerve monitoring. Details are provided on interpretation of testing, and the pitfalls of interpretation are discussed. Studies are reviewed presenting outcomes of testing.
The facial nerve
One of the primary concerns of the surgeon during resection of an acoustic neuroma (vestibular schwannoma) is injury to the facial nerve. The facial nerve takes a long, winding course from the brainstem into the temporal bone and out to the muscles of facial expression. Any segment of the facial nerve from brainstem to stylomastoid foramen may be injured during the course of surgery, leading to postoperative facial weakness, with potentially devastating functional and social consequences for the patient. The inherent complexity of facial nerve anatomy, made more difficult in the context of a tumor that can stretch the nerve and distort adjacent structures, has prompted methods to minimize facial nerve injury during tumor surgery. Although adoption of the operating microscope and transtemporal surgical approaches have been helpful, it was not until routine use of intraoperative electromyographic facial nerve monitoring that dramatic reductions of postoperative facial palsy were realized. Before monitoring, many publications reported on the anatomic preservation rate of the facial nerve. However, anatomically intact nerves that have undergone trauma from stretching and ischemia may be nonfunctional, which is the only parameter of interest to both patient and surgeon. Facial monitoring helps locate the nerve and provides real-time feedback to the surgeon about its neurophysiologic status. Many studies have shown improved postoperative facial nerve outcomes with its use and its cost-effectiveness. The efficacy of monitoring for routine use during vestibular schwannoma surgery seems clear, with its use being advised by the National Institutes of Health.
Neurophysiology
Neurophysiologic testing of the facial nerve plays an important role throughout the workup and treatment of vestibular schwannomas. Electroneurography (ENoG) may be used to determine the preoperative status of the facial nerve. Electromyography (EMG) is used during surgery to monitor for injury to the nerve. Both of these tests rely on measurements of the compound muscle action potential (CMAP) generated by the muscles of facial expression. Monitoring the CMAP allows a response that is an order of magnitude larger than if a nerve action potential was recorded because of the amplifying effect of the muscle response.
Depolarization of the facial nerve may occur following a mechanical or electrical stimulus, resulting in the generation of a nerve action potential. The nerve action potential is transmitted distally along the facial nerve until it reaches the motor end plates, where it is translated into motor unit potentials emanating from the corresponding muscle fibers. When summed, these motor unit potentials result in the measured CMAP, which reflects the activity of the muscles of facial expression. When the facial nerve is injured, information about the extent of injury can be obtained by examining the CMAP. With respect to electrically evoked CMAPs, the response differs depending on the site of nerve stimulation and extent of injury. When an electrical stimulus is applied proximal to the site of injury, nerves suffering from mild to moderate trauma exhibit reductions in amplitude and prolonged latency. Increasing injury requires an increasing amount of current to elicit a response. Although some nerves may be transected or crushed, many surgically induced injuries are a combination of physiologic conduction block (neuropraxia) and physically injured neural elements (axonotmesis or neurotmesis). An accurate assessment requires stimulation proximal to the anticipated site of injury. When an electrical stimulus is applied distal to the injury in the acute setting, the nerve and muscle still respond, because progressive distal degeneration of the axon (wallerian degeneration) following severe nerve injury takes 48 to 72 hours to reach the nerve ending.
EN o G
ENoG can be used for preoperative assessment of the patient with a vestibular schwannoma to establish the presence of preexisting subclinical facial nerve dysfunction. To perform ENoG:
- •
The electrical stimulus is applied transcutaneously at the main nerve trunk near the stylomastoid foramen
- •
The CMAP is measured via surface recording electrodes placed at the nasolabial crease to assess orbicularis oris function in response to stimulation
- •
The relevant metric is comparison of the peak-to-peak amplitude of the CMAP at a supramaximal stimulus between the side with the tumor and the, presumably normal, contralateral side.
Interpretation of EN o G
Like electronystagmography, there are normal, expected variations from side to side and from person to person. Therefore, there must be at least a 30% difference between the 2 sides before it can be regarded as evidence of facial nerve dysfunction on the side with the smaller amplitude. Care must be taken in the interpretation of ENoG results, because operator error can result in poor test-retest reliability. In particular, ENoG testing requires training and experience for it to be accurate, including the use of an optimized lead placement strategy instead of standardized placement.
ENoG before surgery is useful for multiple reasons. Patients with clinically normal facial function may have subclinical neuropathy. With this knowledge, the surgeon can better counsel the patient with severe preoperative ENoG abnormalities who may be at higher risk of postoperative facial paralysis. Reasons for severe preoperative ENoG abnormalities include:
- 1.
An acoustic tumor being more infiltrative or compressive than typical tumors
- 2.
The presence of another type of tumor that may have a higher risk of facial palsy (eg, facial neuroma).
Preoperative counseling in these circumstances can include a greater emphasis on treatment of facial palsy, subtotal resection, or decompression in lieu of resection. Residual tumor can be followed or treated with stereotactic radiosurgery. Preoperative facial nerve dysfunction can influence intraoperative facial nerve monitoring, making such monitoring less effective because the nerve is often in a hyperexcitable state. ENoG allows the surgeon and monitoring neurophysiologist to be prepared for this possibility.
In contrast, ENoG is not typically helpful in the postoperative setting, even in the case of a delayed facial palsy following surgery. ENoG may be helpful in the context of a complete postoperative facial paralysis to determine when facial nerve decompression is indicated, in the same way that it used for patients with Bell palsy, in which edema at the meatal foramen (the narrowest point of the fallopian canal) is posited to be the epicenter of neural injury. However, abnormal postoperative ENoG does not pinpoint the meatal foramen as the epicenter of injury after it has undergone sustained surgical dissection over a broad segment of the nerve during tumor resection. Thus, the usefulness of surgical reexploration to decompress the nerve after an abnormal electroneurogram is unclear, because there may be multiple causes for facial nerve injury. Our practice is to routinely decompress the meatal foramen during the initial translabyrinthine and middle cranial fossa approaches for vestibular schwannoma to minimize this potential mechanism of postoperative nerve injury. In addition, with a postoperative facial palsy, we institute therapy with steroids and antivirals, because viral reactivation is another potential cause of postoperative facial nerve weakness.
Intraoperative Facial Nerve Monitoring
Facial nerve monitoring is routinely used in surgery for acoustic tumors because:
- 1.
It aids in the early identification of the facial nerve
- 2.
It detects nerve injury during dissection
- 3.
It provides a means for assessing nerve function after dissection is complete.
Intraoperative monitoring should be used only as an adjunct to surgical judgment in the assessment of the facial nerve. False-positives and false-negatives can occur with monitoring, so a knowledgeable surgeon and monitoring team are essential because “poor monitoring is worse than no monitoring.” Operating with poor monitoring is comparable with using a malfunctioning minesweeper: if it cannot be relied on, it is best not used at all. If the monitoring results are not consistent with the surgeon’s assessment of anatomy, tumor, and the perceived position and status of the nerve, the surgeon should proceed with caution and may even choose to reject the monitoring information if it contradicts these parameters.
Numerous facial nerve monitoring systems are in use today. Most systems are EMG based, such as the Medtronic Nerve Integrity Monitor (NIM) (Jacksonville, FL, USA) and the Neurosign system (Carmarthenshire, UK). However, the Silverstein Facial Nerve Monitor (Medical Electronics Co., Stillwater, MN, USA) uses a motion pressure detector attached to the cheek. Several studies have suggested that EMG-based systems are more sensitive than motion detection systems for facial nerve monitoring, and thus should be considered the monitor of choice for vestibular schwannoma surgery. False-positives have been reported with motion detection systems, such as stimulation of the trigeminal nerve resulting in contraction of mastication muscles that can trigger the motion detector, leading to an inaccurate impression of facial nerve stimulation. In contrast, the primary limitation of EMG-based systems is that facial nerve monitoring is disabled during the use of electrocautery, which causes a high-intensity electrical artifact that obscures the true EMG signal. Future generations of commercial facial nerve monitoring systems will address the issue of monitoring during cautery, especially during bipolar cauterization, which is more localized than unipolar cauterization in terms of current spread and interference with EMG monitoring. Research is underway examining other potential avenues for facial nerve monitoring, including use of transcranial magnetic stimulation, optical stimulation, and video monitoring. Numerous multi-modality neurophysiologic monitoring devices are also available for facial nerve monitoring, but because they are intended to perform many other functions, these devices can be complex and require in-depth training before they can be safely used.
Training issues in intraoperative facial nerve monitoring
The successful use of intraoperative facial nerve monitoring requires that the surgeon is trained to understand and interpret the physiologic responses. Furthermore, if the surgeon also takes on the responsibility of the electrode and device setup, specific training in the technical aspects of monitoring is required. Meticulous attention to detail must be paid to anesthesia, the monitoring device, and the electrodes to ensure accurate results. At our institution, the surgeon performs intraoperative monitoring in conjunction with a technologist who has received special training and certification (Certification in Neurophysiologic Intraoperative Monitoring [CNIM]). However, at many institutions, surgeons perform the technical setup. Although this is an appropriate model, many staff physicians have had little or no monitoring training other than a cursory introduction by a sales representative. In academic institutions, monitoring setup is often performed by residents whose only training is cursory, word-of-mouth advice by other residents who themselves typically lack an understanding of the technical aspects of monitoring.
Our review of medicolegal cases, as well as quizzing many residents from around the country, often confirms a lack of monitoring training. Staff surgeons come to rely on the residents, assuming a higher level of knowledge than may be present. To improve monitoring and enhance patient safety, we suggest that a written protocol be established for monitoring at each institution, and that a written curriculum with competency testing be required for all individuals performing monitoring. Furthermore, routine, rather than sporadic, use of facial nerve monitoring during operations in which the nerve potentially is at risk results in staff who are familiar with proper techniques and troubleshooting.
Setup and technique for facial nerve monitoring
Several steps are necessary to reliably perform EMG-based facial nerve monitoring.
Step 1. Ensure that the anesthesiologist avoids the use of long-acting muscle relaxants. Short-acting muscle relaxants such as succinylcholine are typically acceptable for induction, except in the rare case of the patient with pseudocholinesterase deficiency, in whom this drug is broken down slowly and thus experiences prolonged paralysis.
Step 2. Be wary about local anesthesia (eg, lidocaine or marcaine), which can chemically induce a temporary facial paresis, rendering monitoring useless. Most are aware that the injection must avoid the facial nerve at the stylomastoid foramen near the mastoid tip, which is particularly important in children for whom the mastoid tip may be poorly developed. Less well known but of great importance is that care must also be taken to avoid local anesthesia entering the middle ear, which is surprisingly common during chronic ear surgery when injecting the ear canal in the presence of a tympanic membrane perforation.
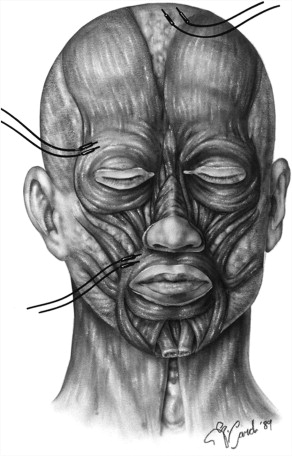
Step 3. Place electrodes carefully. Intramuscular needle electrodes are inserted in a paired manner at the nasolabial groove (orbicularis oris) and near the eyebrow (orbicularis oculi) on the side to be monitored ( Fig. 1 ). Care is taken to direct the electrodes away from the ocular globe to avoid inadvertent trauma to the eye. Our experience over the decades has shown that there is no need to risk ocular injury by placing the needle electrodes inferior to the eyebrow. Two additional electrodes are placed subcutaneously in a distal location such as over the sternum or the ipsilateral shoulder, one serving as a ground for the recording channels and the other as a return for the monopolar nerve stimulator. Fig. 1 shows the ground and anode electrodes placed on the forehand, a location we had used for many years and is used in many centers today. In more recent years, we place these electrodes on the sternum which appears to result in less cautery artifact. Consistency is important to reduce errors. We routinely color code electrodes: blue for eyes, red for lips, green for ground, white for anode, and black for cathode. Our mnemonic for this, which many have adopted internationally, is Blue Eyes, Red Lips, Green Ground. The cathode is used for stimulation rather than the anode because cathodal stimulation is more effective.
Step 4. After the electrodes are connected to the nerve monitor, check the impedances of the different electrode pairs. The independent electrode impedance should be less than 5 kohm, whereas interelectrode impedance should be less than 2 kohm. If the impedance is too high, this suggests that the needle electrodes may be poorly positioned or faulty; the electrodes should be repositioned or replaced and then retested.
Step 5. Perform a “tap test” to check the integrity from the electrode to the recording device. Tapping the skin over each pair of facial recording electrodes should elicit a visual signal on the oscilloscope as well as a concurrent acoustic signal from the loudspeaker. It is important that facial nerve monitors represent responses not just visually on an oscilloscope but also acoustically so the surgeon receives real-time feedback. The surgeon cannot continually observe the oscilloscope and operate. For those who only rely on a technician watching the screen, if the technician looks away for a moment during a lengthy case, an important response can be missed. Conversely, devices that only have an audible response with no oscilloscope lose the opportunity to differentiate some forms of artifact from true responses. Multimodality monitoring increases the need to have a technical assistant. Other increasingly common modalities include laryngeal monitoring, auditory brainstem recording, somatosensory recording, and transcranial motor evoked potentials.
One common misunderstanding about the tap test is that hearing a response means that everything is working perfectly. This is not the case. Performing a tap test on a paralyzed face also creates a response, because tapping adjacent to an inserted electrode elicits an electrical artifact, not a true CMAP. The tap test has benefit in that it checks whether the connections from the recording electrodes to the oscilloscope and loudspeaker are intact, but it provides no information regarding the stimulating side of the system or about the functional state of the facial nerve or muscles. Thus, the setup is not finished after obtaining a positive tap test, but should also include the final 2 steps (described later).
Step 6. After incision and soft tissue exposure, check for current flow using a nerve stimulator. Touching the stimulator to soft tissue or wet bone should result in near 100% conduction of current from the stimulator to the monitor. Most devices display the returned current visually. Others may present an audible tone (eg, warble) or digital voice confirmation (eg, stimulus) that is distinct from a true response tone (eg, beep). The volume of the nerve monitor should be adjusted from the start to ensure that the surgeon can hear it over the ambient sounds in the operating room (eg, the drill, suction, laser, babble).
Step 7. Stimulate the nerve at an early point in the surgery before any significant manipulation of the nerve is performed. Placing the nerve stimulator near the porus acousticus, the root entry zone, or the second genu of the facial nerve after entry into the mastoid antrum during surgical exposure triggers a CMAP that is detected by the facial nerve monitor. The distance from the nerve and the amount of intervening tissues determines the current setting. Even though a normal facial nerve responds to 0.05 mA in the cerebellopontine angle, if the surgeon has 0.5 cm of intervening soft tissue or a few millimeters of bone, the current may need to be temporarily turned up to 1 to 2 mA before a baseline, far-field response can be obtained by volume conduction of the current through intervening tissue. Once a confirmatory baseline response is obtained, we reduce the current intensity to lower levels based on how distal we are from the nerve. In 30 years of using such mapping techniques with modern current settings (eg, pulse durations ∼100 microseconds at ∼5 Hz), we have observed no detrimental effect to the nerve. Conversely, those who neglect to routinely obtain a baseline response before nerve dissection risk monitoring with a system that may be faulty due to set up errors, persistent muscle relaxants or chemical paralysis from lidocaine.
See Box 1 for a summary of steps for facial nerve monitoring.
- 1.
Ensure that the anesthesiologist avoids the use of long-acting muscle relaxants
- 2.
Be wary about local anesthesia (eg, lidocaine or marcaine), which can chemically induce a temporary facial paresis, rendering monitoring useless
- 3.
Place electrodes carefully
- 4.
After the electrodes are connected to the nerve monitor, check the impedances of the different electrode pairs
- 5.
Perform a tap test to check the integrity from the electrode to the recording device
- 6.
After incision and soft tissue exposure, check for current flow using a nerve stimulator
- 7.
Stimulate the nerve at an early point in the surgery before any significant manipulation of the nerve is performed
Interpretation of intraoperative facial nerve EMG monitoring
The surgeon must be knowledgeable not only in anatomy but in the pertinent neurophysiology to make proper use of monitoring. Even flawlessly accrued information conveyed to a surgeon is of little value if the data cannot be interpreted and surgical maneuvers implemented based on the information. Electromyographic responses can:
- 1.
Occur because of trauma or other nonelectric stimuli, or
- 2.
Be electrically triggered.
Continuous free-running EMG
Responses caused by trauma or other nonelectric stimuli are detected during continuous free-running EMG, which monitors for CMAPs in response to any type of nerve irritation. Two types of CMAP activity have been categorized, depending on the type of irritation :
- 1.
A burst potential, which consists of a single polyphasic response caused by near-simultaneous activation of multiple motor units ( Fig. 2 )





