cough. Subspecialty voice, airway, and swallowing centers (“voice centers”) composed of fellowship-trained laryngologists and cough- and voice-specialized speech-language pathologists often represent this “bottom of the funnel” subspecialty practice, with the treating physician leading the data collection, interpreting prior medical testing results, and directing further workup and treatment.
Any specialist can serve as the knowledgeable point person in a health system or community to direct further workup and care for chronic cough patients. However, most patients who present to voice centers with intractable chronic cough have previously been evaluated and treated unsuccessfully, or at a minimum incompletely, medically and surgically by various pulmonologists, allergists and immunologists, gastroenterologists, primary care providers, and other general or subspecialty-trained otolaryngologists for months, if not years. The reader should understand that the term “voice center” will be used for convenience to define the teritary or quaternary clinician and their team of chronic cough treatment providers, but the reader should also understand that this clinician may not always be a laryngologist or otolaryngologist. This chapter will focus on the final pathway for evaluating and treating chronic cough patients who may have already been seen by multiple providers.
A FLEXIBLE INITIAL APPROACH TO A NEW PATIENT
Chronic cough is a symptom, not a diagnosis. There is almost universally a discoverable etiology for chronic cough, potentially multifactorial, and when all tests and treatments are completed by a willing patient, an idiopathic or unknown cause for the chronic cough will rarely be the diagnosis. It would be ideal to have an algorithm to follow for refractory chronic cough patients. However, patients do not always easily fit into the algorithm, nor do they have only one etiology contributing to their cough. Patients have often tried and failed multiple medications prescribed one or more times by multiple providers at various doses without a clear pattern of escalation or substitution. Similarly, reasons for initiating or terminating the treatments are often vague or fall into the category of “it just didn’t help.” Most patients have been seen by several physicians along the road to the voice center team and have often had many empiric trials of medications for chronic cough and repeated testing, including tests for pulmonary, gastroenterological, and sinonasal etiologies for the cough. Patients express feelings of hopelessness when they are referred to their ultimate chronic cough care team based on the lack of success leading up to the visit. It is often paramount to give them hope at the first visit or at least reveal what can be further evaluated and tried that has not already been done (if anything).
It is not unusual to meet a patient who has been on multiple steroid inhalers for years despite having normal pulmonary function testing (PFT), has never had bronchodilator improvement on PFTs, and has never been offered bronchoprovocation testing such as methacholine challenge testing to rule out asthma (see Chapter 2). It is also not unusual to meet refractory chronic cough patients who have already undergone sinonasal surgery without improvement in their postnasal drip symptoms, despite never having had chronic sinusitis documented. These patients may have met criteria for septoplasty (straightening of the nasal septum to improve breathing), but due to the lack of complete workup for other etiologies of chronic cough, the patients received surgery that did not fix the chronic cough complaint for which they presented. It is not uncommon for chronic cough patients to report partial or temporary relief with topical and systemic steroid treatments. Steroids are nondiscriminatory in treating inflammation and can work on inflamed tissues of the oropharynx, nasopharynx, larynx, and airways regardless of the underlying etiology of the inflammation.
A definitive reflux workup is also often incomplete when chronic cough patients present to a voice center. Patients are often told they do not have reflux or, more commonly, that reflux is not causing the chronic cough because their reflux medication and normal upper gastroesophageal endoscopy (EGD) are sufficient to rule out reflux as a cause of their chronic cough. However, acid suppression has been shown to not control physiologic reflux (see Chapter 4).1 Our understanding of how the digestive enzyme pepsin is the probable culprit in causing laryngopharyngeal reflux (LPR) symptoms is maturing, as is our understanding of what happens when we eliminate reflux and not just acid from the laryngopharynx. Chronic cough often improves after antireflux surgery in patients with chronic cough and positive pharyngeal reflux events demonstrated on impedance probes that cover the entire esophagus and span the upper esophageal sphincter (UES) to the oropharynx (hypopharyngeal-esophageal multichannel intraluminal impedance with dual pH, “HEMII-pH”).2 We can now better understand the pathophysiology of LPR, its role in chronic cough and thus more clearly explain to our patients how traditional modalities (prior gold standards such as dual pH probes) for diagnosing gastroesophageal reflux disease (GERD) are inadequate to rule out reflux as the cause of chronic cough.3 Patients routinely present with normal 24-hour dual probe pH tests and, more recently, normal pharyngeal ph-metry testing results (Restech® Dx-pH probe, Respiratory Technology Corp, San Diego, CA) and dual pH with impedance that only detects liquid events up to 17 cm above the LES and not above the UES as is the case with HEMII-pH.
As discussed in Chapter 4, GERD and LPR are different presentations of a common underlying phenomenon: the physiologic retrograde movement of gastric contents superiorly. Reflux testing with HEMII-pH has the ability to rule in LPR as an etiology for refractory chronic cough and characterize the acidity or lack thereof in the refluxate.2, 4 High-resolution esophageal manometry (HRM) is also a missing component in the workup of the chronic cough patient. Many patients do not have true reflux from the stomach; rather, they present with chronic cough or other LPR symptoms due to comorbid issues from esophageal dysmotility that lead to direct LPR changes in the laryngopharynx or generate cough through vagally mediated mechanisms form within the esophagus (see Chapter 7).
Due to the breadth of knowledge that must be mastered by most primary care clinicians, general pulmonologists, gastroenterologists, and otolaryngologists, simple algorithms to work through a new chronic cough patient are of value. Figure 9–1 is an algorithm that should aid the front line of treating clinicians.5
This algorithm is not realistic and is often impossible to work through in the quaternary referral voice center. Adhering to this and “reinventing the wheel” with every patient leads to time and money wasted, both personal and in health care dollars, for patients who have already been on a long road with a difficult symptom. Collecting previous records, synthesizing the data, and deciding on what options remain for the refractory chronic cough patient is often performed and then options for next steps are determined. If work with a SLP who specializes in cough suppression strategies has never been pursued, this is often prescribed at the first visit to the voice center (see Chapter 8). In addition to the lack of SLP involvement in the management of a patient with refractory chronic cough, the most common omissions from the workup for underlying causes of chronic cough in the author’s experience include: bronchoprovocation challenge testing (eg, methacholine challenge testing), HEMII-pH testing, and, in patients with meal-associated coughing, videofluoroscopic swallow studies (VFSS) or flexible endoscopic evaluation of swallowing (FEES) testing.
A few recent papers have addressed the costs associated with the inappropriate, unnecessary, and/or unrelenting treatments and workup for LPR. It appears the health care system could save billions of dollars annually if PPIs were not empirically prescribed for all patients with LPR symptoms, including chronic cough. When considering patients who have been worked up for extraesophageal symptoms of reflux, a study by Francis et al looked at 281 patients, half of whom had cough as their complaint.6 They found the overall cost per patient improvement (including Medicare costs for diagnosis, treatment, and unnecessary medications, etc) to be $13,700 per patient, most of which came from the prescription of proton-pump inhibitor (PPI) medications. Their initial annual direct cost was $5,154 for the workup of these patients, 5.6 times higher than patients with classic GERD. These data reinforce the trial and error method occurring in the workup and treatment (often empiric trials of PPIs) of chronic cough patients. The overall estimated annual cost in the United States of treating LPR is above $50 billion.6
Figure 9–1. The basic chronic cough treatment algorithm (inspired by Pratter et al.5). An initial treatment algorithm for treating clinicians on the front lines of chronic cough. This is not ideal for the refractory chronic cough patient who has seen multiple providers and has already had multiple tests and treatments. It is not efficient in these cases because a quaternary chronic cough referral center clinician will have more clinical acumen and can often work in a more efficient and cost-saving manner outside this fixed pathway.
More recently, a study by Carroll et al used the Francis et al study’s cost estimates to determine if up-front impedance with dual-pH testing could decrease the cost burden in the reflux workup of patients with LPR.7 The Carroll study reported an estimated 40% average cost savings over empiric high-dose PPI medication trials. With PPIs being the primary driver of cost to the healthcare system and with more data suggesting potential deleterious side effects of PPI use, up-front reflux testing makes sense.8 Many centers (and thus patients) do not have access to HEMII-pH testing, thus the ability to perform a 24-hour reflux test that evaluates acid and nonacid refluxed stomach contents to and above the UES. Using clinical acumen and positive predictive value in the face of patient-reported symptoms beyond chronic cough, more traditional tests for reflux such as capsule pH-metry (BRAVOTM Reflux Testing System, Medtronic Inc, Minneapolis, MN) or dual pH probes may be worth exploring first before prescribing PPIs. If up-front, acid-only reflux testing is unrevealing, it may at least prevent unnecessary PPI prescriptions and lead to further referral to a center where HEMII-pH testing is available for some chronic cough patients.
ASKING FOR THE RIGHT HELP AT THE RIGHT TIME
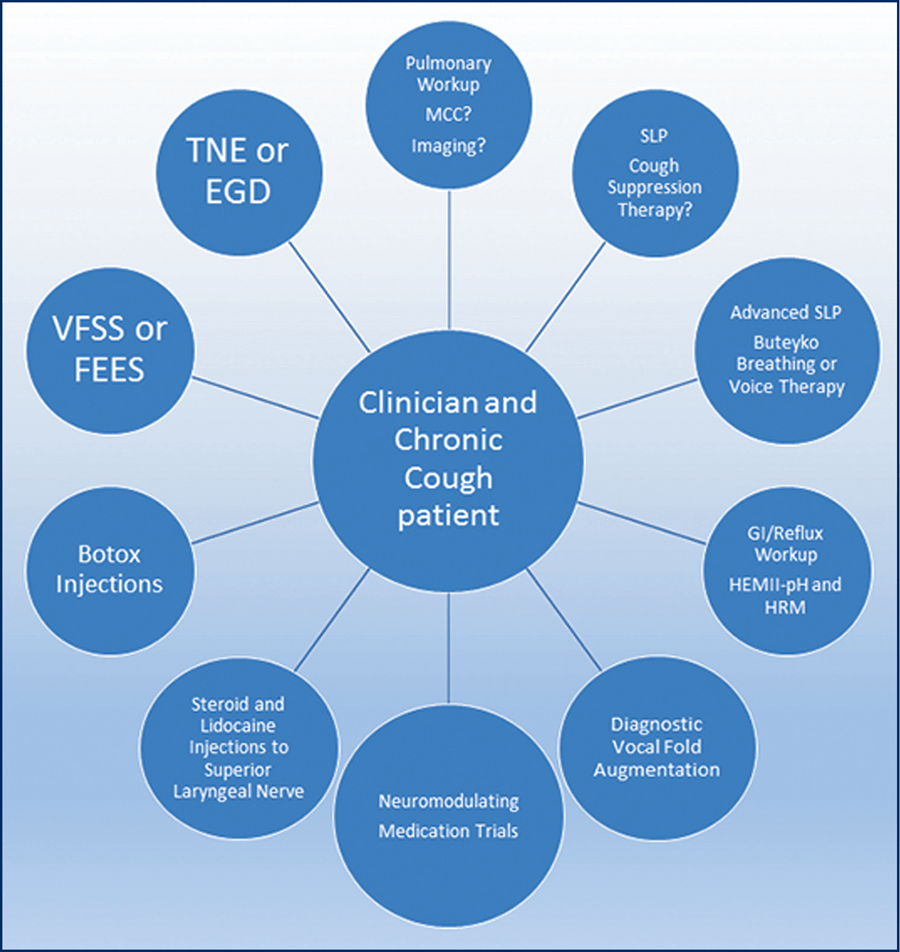
Instead of an algorithm, the diagrammatic approach to the refractory chronic cough patient who has already had a thorough workup by numerous other providers and who has tried prior medical or surgical therapies is more akin to a treatment “wheel” (Figure 9–2). The quaternary chronic cough clinician sits with the patient at the center of the wheel, and all available unexplored options reside at the end of the spokes leading to and from the center. The treating clinician can pull any and all diagnostic and therapeutic options back from the rim individually or in tandem. Depending on the quaternary clinician’s specialty, the spokes of the wheel will vary. For example, if a pulmonologist is the lead, a laryngologist would be at the end of one of the spokes and vice versa. For many patients, the number of spokes will be few due to their prior workup, and thus the potential for improvement is closer at hand. Some patients have had a partial or incomplete workup in numerous areas, and more spokes of the wheel will potentially need to be explored. Any missing pieces, especially of the prior pulmonary and sinonasal workup, are identified, as are treatments that can be offered for chronic cough beyond the big three etiologies. It is important to know what options remain for the patient (ie, they have already had a good neuromodulator medication trial, or they underwent vocal fold augmentation for a known paresis).
Clinical experience and positive predictive value of which etiology is causing the chronic cough will typically direct the order in which patients explore different spokes on the wheel. Etiologies with malignant potential are always explored first, or at least in tandem with the highest nonmalignant potential etiology, especially in smokers. Cancers of the esophagus, airway, lung, and head and neck are always on the radar of the quaternary chronic cough clinician. These concerns seem obvious, but they can easily be overlooked—for example, if the chronic cough patient is a smoker and has yet to see a pulmonologist, or if the patient has solid food dysphagia and a barium swallow, or better yet an EGD, has not been performed in a prior heavy smoker. Chronic cough in the face of persistent hoarseness is often accompanied by benign vocal fold changes, but laryngoscopy is required in patients with persistent hoarseness of 4 weeks or more to rule out laryngeal or other mucosal malignancies of the head and neck. In smokers the 4-week waiting period is ignored when there is no other reason for the voice change (concurrent upper respiratory infection, etc).9 Chronic cough in the face of unilateral middle ear effusion, unremitting nasal obstruction and recurrent epistaxis requires nasopharyngoscopy and nasal endoscopy before treating empirically to rule out sinonasal tumors.
Figure 9–2. The refractory chronic cough wheel. With the patient and quaternary clinician at the center, clinical judgment and patient history guide which spokes of the wheel deserve exploration. The patient is sent “out” the spokes to another specialist, diagnostic, or treatment option then returns “in” for reassessment and further consideration if necessary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree