Purpose
To compare the clinical outcomes of two treatment approaches for bilateral nasolacrimal duct obstruction (NLDO) in infancy.
Design
Multicenter, randomized clinical trial.
Methods
We studied 57 infants between the ages of 6 and <10 months who had bilateral NLDO. Participants were randomized to receive either (1) immediate office-based probing within two weeks (n = 31) or (2) 6 months of observation and nonsurgical management followed by surgical facility-based probing for unresolved cases (n = 26). Treatment success was defined as the absence of clinical signs of NLDO (epiphora, increased tear lake, mucous discharge) in both eyes on masked examination at 18 months of age.
Results
In the observation and deferred facility probing group, resolution without surgery occurred by 6 months after randomization in both eyes for 14 participants (56%), in one eye for 5 (20%), and in neither eye for 6 (24%). Eight participants in the observation and deferred facility probing group underwent facility probing (one of whom later had a second facility probing). Four participants in the immediate office probing group later underwent an additional procedure in a surgical facility. In the immediate office probing group, treatment success at 18 months of age occurred in both eyes for 19 of 29 (66%) participants and in one eye for 3 (10%); in the observation and deferred facility probing group, treatment success occurred in both eyes for 19 of 25 (76%) participants and in one eye for 3 (12%) (difference in success = −10%; 95% CI = −35% to 14%).
Conclusions
Both the immediate office probing approach and the observation and deferred facility probing approach are successful and reasonable treatment options for infants with bilateral NLDO.
Congenital nasolacrimal duct obstruction (NLDO) occurs commonly in infants and often resolves without surgery. Treatment of infants with symptoms of NLDO persisting beyond 6 months of age generally follows one of two management approaches. One approach is to probe the nasolacrimal duct in the office setting, using topical anesthesia and restraint. Another approach is to continue observation, prescribing nonsurgical treatment with lacrimal sac massage, topical antibiotics or both, because prospective studies have shown that most cases of NLDO that persist to between 6 and <10 months of age (64% to 70% ) resolve within 6 months without surgery. If the NLDO persists, a probing is often performed under general anesthesia in a surgical facility because the older infant would be more difficult to restrain sufficiently so as to complete probing safely in the office setting.
We recently conducted a randomized trial comparing the immediate office probing approach with the observation and deferred probing approach, and we have previously reported results in participants with unilateral NLDO. Although the trial did not find a statistically significant difference in the outcomes between treatment groups, the trial did show that the immediate office-based probing approach was likely to be at least as successful as the observation and deferred probing approach for treating infants with unilateral NLDO. Herein we report the clinical outcomes of participants who had bilateral NLDO in the same randomized clinical trial.
Methods
The study was supported through a cooperative agreement with the National Eye Institute of the National Institutes of Health and was conducted by the Pediatric Eye Disease Investigator Group (PEDIG) at 22 academic and community-based pediatric ophthalmology practices. The protocol and Health Insurance Portability and Accountability Act (HIPAA) compliant informed-consent forms were approved by institutional review boards, and a parent or guardian of each patient in the study gave written informed consent. The study is listed at www.clinicaltrials.gov ( NCT00780741 ). Key aspects of the protocol have been published. The full protocol is available on the PEDIG website ( www.pedig.net ) and is briefly described below.
The trial enrolled 57 participants aged 6 to <10 months who had bilateral NLDO, onset of NLDO symptoms before 6 months of age, no prior nasolacrimal duct surgery, and no Down syndrome or craniofacial anomalies. Bilateral NLDO was defined as the presence of epiphora, increased tear lake, and/or mucous discharge in both eyes, a dye-disappearance test was not required. Each participant was randomly assigned to receive either (1) bilateral probing in the office setting with topical anesthesia and gentle restraint (often including use of a papoose board) within two weeks of study entry or (2) 6 months of observation and nonsurgical management followed by probing in a surgical facility for unresolved eyes. During the 6-month observation period, lacrimal massage was to be performed when discharge was present, and antibiotic eyedrops were to be used when discharge was purulent. Participants’ parents were contacted by phone 3 months (± 2 weeks) after randomization to determine whether NLDO symptoms were present. Participants had follow-up visits 6 months (± 2 weeks) after randomization and a masked primary-outcome examination at 18 months of age (± 4 weeks). At the 6-month postrandomization visit, the participants in the observation and deferred group who had one or more clinical signs of NLDO were to undergo probing in a surgical facility within 4 weeks. After the initial treatment approach of immediate probing of both eyes in the office or 6 months of observation followed by deferred probing for unresolved eyes, further treatment (including reoperation) was performed at the investigator’s discretion.
The primary efficacy outcome was success of the treatment approach, defined as the absence of all clinical signs of NLDO (epiphora, increased tear lake and mucous discharge) in both eyes as assessed by a examiner masked to the previous treatments during a visit at 18 months of age, regardless of whether the patient had received any probing procedures. A secondary outcome was months of NLDO symptoms in one or both eyes between randomization and 18 months of age. For participants who did not complete the primary outcome visit, we attempted to contact parents by phone to ask whether their child had NLDO symptoms.
The analysis followed the intent-to-treat principle. The differences between in the treatment groups in the proportion of eyes with success and a 95% confidence interval (CI) were calculated using binomial regression with generalized estimating equations to adjust for the correlation between the two eyes of each participant. The differences in the proportion of participants in the treatment group who had success in both eyes and a 95% CI were calculated using binomial regression. Participant-level differences in treatment groups in months of symptoms and a 95% CI were estimated using an independent samples t test.
All analyses were conducted using SAS v 9.3. (SAS Institute, Cary, NC).
Results
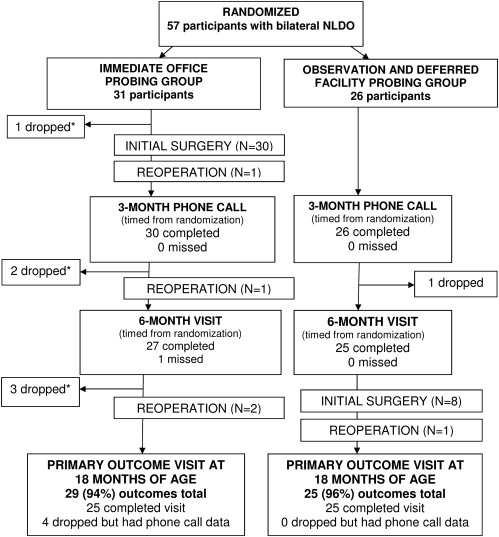
Between November 2008 and September 2010, 57 participants with bilateral NLDO were enrolled as part of a larger randomized trial that included both unilateral and bilateral NLDO. Of the children with bilateral NLDO, 31 and 26 participants were randomized to immediate office probing or observation and deferred facility probing groups, respectively ( Table 1 ). The participants were an average of 7.7 (± 1.3) months of age; 24 (42%) were female, and 40 (70%) were white. Fifty-one (89%) participants had been treated previously with antibiotics, lacrimal massage or both.
| Immediate Office Probing Group | Observation and Deferred Facility Probing Group | |
|---|---|---|
| Participant-Level Characteristics | (n = 31) | (n = 26) |
| Female sex, n (%) | 13 (42) | 11 (42) |
| Race/ethnicity, n (%) | ||
| White | 19 (61) | 21 (81) |
| Hispanic | 7 (23) | 5 (19) |
| African American | 4 (13) | 0 (0) |
| Other | 1 (3) | 0 (0) |
| Age at enrollment, n (%) | ||
| 6 to <7 months | 12 (39) | 11 (42) |
| 7 to <8 months | 3 (10) | 7 (27) |
| 8 to <9 months | 8 (26) | 4 (15) |
| 9 to <10 months | 8 (26) | 4 (15) |
| Mean (SD) months | 7.8 (1.4) | 7.5 (1.2) |
| Eye-Level Characteristics | (n = 62) | (n = 52) |
| Previous treatment, n (%) | ||
| Lacrimal massage and/or topical antibiotics | 36 (58) | 30 (58) |
| Lacrimal massage only | 9 (15) | 12 (23) |
| Topical antibiotics only | 6 (10) | 8 (15) |
| None | 9 (15) | 2 (4) |
| Epiphora present, n (%) | 46 (74) | 38 (73) |
| Increased tear film present, n (%) | 62 (100) | 48 (92) |
| Mucous discharge present, n (%) | 36 (58) | 35 (67) |
In the immediate office probing group, 30 of 31 patients (97%) underwent bilateral office probing. The remaining patient did not have surgery, although the parents later reported by phone that the NLDO had resolved. Of the patients who underwent immediate office probing, 4 (13%) underwent a second surgical procedure at the investigator’s discretion before 18 months of age (1 had bilateral probing, and 3 had bilateral nasolacrimal intubations, all performed in a hospital outpatient operating room under general anesthesia). No surgical complications were reported.
In the observation and deferred probing group, resolution without surgery occurred by six months after randomization in both eyes for 14 participants (56%, 95% CI = 37% to 74%), in one eye for 5 (20%), and in neither eye for 6 (24%). Of the 11 participants whose NLDO did not resolve after 6 months of observation, 7 underwent bilateral facility probing (1 of whom later underwent a second procedure, a bilateral nasolacrimal intubation), 1 underwent unilateral facility probing, and 3 did not undergo surgery. All 9 surgeries were performed under general anesthesia, 6 (67%) in a hospital outpatient operating room and 3 (33%) in an ambulatory surgery center. No surgical complications were reported.
Of the 31 participants in the immediate office probing group, 25 (81%) completed the 18-month visit; 4 (13%) did not complete the visit but were included in the analysis because outcome data were reported by parents via phone contact (NLDO signs were absent in 3 of the 4 patients); and 2 (6%) participants were not included because they did not complete the visit, and phone contact with their parents was unsuccessful ( Figure ). Of the 26 participants in the observation and deferred group, 25 (96%) completed the 18-month visit, and 1 participant was not included because the visit was not completed and phone contact with the parents was unsuccessful.
Treatment success at 18 months of age occurred in 41 (71%) of 58 eyes in the immediate office probing group compared with 41 (82%) of 50 eyes in the observation and deferred probing group. The difference in the proportion of eyes with success (immediate office probing group minus observation and deferred probing group) was −11% (95% CI = −32% to 9%). In the immediate office probing group, treatment success at 18 months of age occurred in both eyes for 19 of 29 (66%) participants and in one eye for 3 (10%) participants. In the observation and deferred probing group, treatment success at 18 months of age occurred in both eyes for 19 of 25 (76%) participants and in one eye for 3 (12%) participants ( Table 2 ). The difference in the proportion of participants with success in both eyes was −10% (95% CI = −35% to 14%).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


