7 Facial Plastic and Reconstructive Surgery
Section Editor
Contributors
7.1 Craniomaxillofacial Trauma
For ear and temporal bone trauma, see Chapter 2.1.2. For laryngeal fractures, see Chapter 4.1.2. For neck trauma, see Chapter 5.1.1.4.
7.1.1 Nasal Fractures
Key Features
• Nasal fractures are the most common head and neck fracture.
• They have aesthetic and functional implications.
• Closed reduction has limited application.
• Septal hematoma should be recognized early and managed.
• Define the injury precisely and anatomically before planning any intervention.
• Even if no surgical intervention is planned, reevaluate the patient after any traumatic swelling has resolved (usually 1–2 weeks)
Nasal fracture clinical presentation may include epistaxis, change in external nasal appearance, nasal airway obstruction, and infraorbital ecchymosis.
Epidemiology
Nasal fractures are cited as the most common type of facial fracture, accounting for approximately half of all facial fractures. These injuries occur largely in the younger, physically active segments of the population and predominantly in males. The most common mechanism is blunt trauma; these fractures also occur via penetrating and high-energy injuries. Finally, nasal fractures occur not only in isolation but also frequently in conjunction with more extensive facial fractures.
Evaluation
Physical examination is facilitated if the nose is decongested. Visual inspection, manual palpation, and anterior rhinoscopy are essential. If possible, nasal endoscopy can be performed to increase the acquisition of meaningful clinical data.
The integrity of the nasal skin should be assessed. Globally, the examiner should determine if the nose is straight, if there is a deviation, or if there is a C-shaped deformity. Via visual inspection and palpation, the integrity of dorsal support can be determined. Has the nose maintained normal midline support, or is there an acute saddle deformity and if so what anatomic disruption is contributing? The nasal bones should be examined. Based on visualization and palpation, are there fractures of the nasal bones?
The tip and lower two thirds of the nose should be examined. Is there an injury to the cartilaginous framework? Determining the status of the septum is frequently underemphasized; however, appropriate appreciation and management of septal injuries is essential to the restoration of optimal nasal function and appearance. And finally, the examiner should look for and document the presence or absence of a septal hematoma. If present, it should be expeditiously and appropriately managed.
Photographs should be done similar to the views obtained for rhinoplasty evaluation. Planar radiographs and computed tomography (CT) rarely add more valuable data than that obtained through the physical examination and medical history.
Treatment Options
Observation
When it has been determined that there is minimal displacement of the nasal bones, minimal soft tissue injury, and minimal compromise of the nasal airway, recommend observation and undertake no active surgical or manipulative intervention.
Closed Manipulation
Under local or general anesthesia, the patient’s fractured nasal bones and septum are mobilized and reduced digitally. This may be aided with the use of blunt instruments such as the Boise elevator or Ashe forceps. Traditional closed manipulation is best applied in patients who have actual subluxation or displacement of the nasal bones without significant fracture of the nasal bones themselves.
Modified Open Reduction with Osteotomies
The modified open technique is a limited version of an open technique in which intranasal incisions are made for the introduction of osteotomes. Such patients frequently benefit from manipulation of the nasal bones into position after undergoing bilateral microosteotomies. As with closed manipulation, the position of the septum may impede the success of this technique. A secondary procedure may then be necessary or other treatment offered.
Open Nasal/Septal Repair
The open nasal/septal repair refers to an aggressive approach to the acute management of complicated injuries using existing lacerations or external and intranasal incisions. With this approach the surgeon can reduce, graft, and fixate fractured anatomic components under direct visualization.
Formal Septorhinoplasty
Formal septorhinoplasty after nasal fracture is employed in two general clinical situations: when there has been minimal displacement and treatment is delayed until swelling has resolved, and as a secondary procedure after initial acute management.
Outcome and Follow-Up
Externally stabilizing dressings should be applied similarly to rhinoplasty care. When there have been significant septal injuries, internal soft silastic splints may provide stabilization and aid in the prevention of synechia. Packing is only occasionally necessary.
ICD-9 Codes
471 | Deviated nasal septum |
802.0 | Closed fracture of nasal bone |
802.1 | Open fracture of nasal bone |
Further Reading
Fedok FG, Ondik MP, Preston TW, Goldenberg D. Management of trauma to the nasal bones and septum. In: Stucker FJ, De Souza C, Kenyon GS, Lian TS, eds. Rhinology and Facial Plastic Surgery. Heidelberg/New York/Berlin: Springer-Verlag; 2009
Oeltjen JC, Hollier LH. Nasal and naso-orbital-ethmoid fractures. In: Stewart MG, ed. Head, Face, and Neck Trauma: Comprehensive Management. Stuttgart/New York: Thieme; 2005:39–51
Rohrich RJ, Adams WP Jr. Nasal fracture management: minimizing secondary nasal deformities. Plast Reconstr Surg 2000;106(2):266–273
7.1.2 Naso-Orbito-Ethmoid Fractures
Key Features
• A naso-orbito-ethmoid (NOE) fracture is a severe injury involving depression of nasal bones into ethmoids with associated medial orbital wall fracture.
• It is secondary to a high-energy injury; often associated with intracranial and other injuries.
• It requires open reduction with internal fixation
Epidemiology
Injury results from severe trauma to the frontal and midface region. The most common mechanism is a motor vehicle accident with an unrestrained driver. Seatbelt and airbag use has reduced its incidence in recent years.
Clinical
Signs and Symptoms
Often, patients with NOE fractures have life-threatening injuries and require initial trauma evaluation and stabilization. Eye and brain injuries are common. Concurrent ocular injury, such as globe rupture, lens dislocation, retinal detachment, or vitreous hemorrhage, occurs in ~30% of patients. Patients may have cerebrospinal fluid (CSF) leakage, due to disruption of the anterior skull base. Typical associated signs and symptoms include severe epistaxis, CSF rhinorrhea, diplopia, epiphora, and severe facial pain. The typical facial deformity resulting from disruption of the ethmoids and medial canthal tendon attachments includes flattening of the nasal dorsum, upward tip rotation and loss of projection, and increased interpupillary distance (traumatic telecanthus).
Differential Diagnosis
It is important to differentiate NOE fractures from isolated nasal fractures (see Chapter 7.1.1), orbital fractures (see Chapter 7.1.3), and fractures that involve only the ethmoid labyrinth. CT imaging allows rapid, definitive diagnosis.
Evaluation
History
Mechanism of injury will help determine possible injuries and severity. Often, the patient may be unable to provide history.
Physical Exam
Exam, as with all traumas, begins with ABCs (airway, breathing, circulation). Care must be taken to protect the cervical spine until it has been cleared. Head and face are inspected and palpated for ecchymoses, soft tissue injuries, and bony step-offs. Telecanthus results from NOE fractures. The average intercanthal distance for women and men ranges from 25 to 35 mm; this is usually 50% of interpupillary distance. A distance of ≥40 mm is considered diagnostic of telecanthus. The medial canthal tendon attachment is easily evaluated with the “bowstring” test. While palpating the tendon insertion at the lacrimal crest, the lower lid is retracted laterally. If the tendon insertion is intact, the examiner will feel it tighten like a bowstring. Ideally, the nose should be decongested to allow for an intranasal exam. With use of a headlight and speculum or rigid endoscope, clots and blood are suctioned and mucosal tears, position of the septum, and possible hematomas are noted. Clear fluid may represent a CSF leak. A drop of this fluid on gauze may reveal a “halo sign,” indicative of CSF.
Imaging
Thin-cut axial and coronal CT is the most useful imaging study. Fractures of the facial and nasal bones are readily visualized, with excellent detail of the medial orbital walls and lacrimal region. The integrity of the skull base may be assessed, as well as the presence of pneumocephalus or other intracranial injury. NOE fractures can be categorized according to the degree of comminution at the medial canthal tendon insertion:
• Type I: Large central fragment
• Type II: Comminution of central fragment but not involving the tendon
• Type III: Comminution involving lacrimal fossa and tendon attachment site with tendon laceration
Labs
Routine trauma and preoperative lab studies are necessary as indicated, including complete blood count (CBC), prothrombin time (PT), partial thromboplastin time (PTT), electrolytes, and possibly a toxicology screen.
Treatment Options
Treatment of an NOE fracture requires open reduction with internal fixation. For relatively limited fractures, external ethmoidectomy incision may afford adequate exposure. Often, the surgeon may take advantage of large lacerations for bony exposure. However, a coronal (often termed bicoronal) incision is generally used. Stabilization of the central fracture fragment, to which the medial canthal tendon is attached, is achieved with plating to stable bone, especially in types I and II injuries. Occasionally, intercanthal wiring is necessary to achieve an adequate result, especially in type III injuries, in which severe comminution is present. Many surgeons advocate slight initial overcorrection. Bone grafting may be necessary.
Outcome and Follow-Up
Admission and perioperative antibiotics are required. Frequent vision examinations are performed following repair of orbital fractures. Infection, hematoma, or vision change requires prompt attention to correct underlying issues.
ICD-9 Codes
802 | Fracture of face bones |
802.0 | Nasal bones, closed |
802.1 | Nasal bones, open |
802.7 | Orbital floor (blowout), open |
802.6 | Orbital floor (blowout), close |
802.9 | Other facial bones, open |
Further Reading
Oeltjen JC, Hollier LH. Nasal and naso-orbital ethmoid fractures. In: Stewart MG, ed. Head, Face, and Neck Trauma: Comprehensive Management. Stuttgart/New York: Thieme, 2005;39–51
Strong EB. Frontal sinus and naso-orbital-ethmoid complex fractures. In: Papel ID, ed. Facial Plastic and Reconstructive Surgery. 3rd ed. Stuttgart/New York: Thieme; 2009:977–990
7.1.3 Zygomaticomaxillary and Orbital Fractures
Key Features
• Zygomaticomaxillary complex (ZMC) fractures involve the maxillary face, zygomatic arch, and orbital rim and floor.
• Features of an orbital floor blowout fracture may include enophthalmos, V2 numbness, diplopia, and possibly an orbital rim fracture.
• The fractured ZMC is most often displaced posteriorly and inferiorly.
A ZMC fracture may be called a tripod fracture because there are three sites of fracture—the frontozygomatic suture, the maxillary face, and the zygomatic arch. Isolated fractures of the orbital rim, floor, maxilla, or zygomatic arch can also occur. Surgical repair is indicated in most displaced ZMC fractures, with fixation of one or more fracture sites.
Epidemiology
ZMC fractures are the most common malar bone fractures and the second most common facial bone fracture after the nasal bones. Zygomatic arch fractures are most common in men (in the third decade) and are caused by sports injuries, motor vehicle accidents, or assault.
Clinical
Signs and Symptoms
Patients suffering ZMC or orbital fractures may present with epistaxis, periorbital edema, lacerations, pain, vision change, diplopia, or step-off deformities at the site of fractures. Numbness of the ipsilateral upper lip, gum, nostril, and cheek is common due to fractures through the infraorbital foramen (V2). Orbital signs include chemosis, subconjunctival hemorrhage, immediate proptosis, and enophthalmos. Entrapment of the inferior rectus muscle in the orbital floor fracture can result in diplopia due to impaired extraocular muscle function. Malocclusion may result from either a mobile midface (LeFort) fracture or a concomitant mandible fracture. A depressed zygoma fracture may cause trismus by compressing the coronoid.
Differential Diagnosis
The spectrum of fractures in the zygoma, maxilla, and orbital bones can range from isolated to complicated, from severely displaced to greenstick, and from simple to comminuted. Classification should begin with assessing for midface instability, which would indicate a LeFort fracture (see Chapter 7.1.5). Assessment of the seven bones that constitute the orbit (lacrimal, palatine, frontal, ethmoid, zygomatic, maxillary, and sphenoid) most often reveals fractures at the weakest bones—the lamina papyracea (ethmoid) and orbital floor (maxilla).
Evaluation
Physical Exam
The full head and neck examination must include cranial nerve testing. LeFort fractures have palatal mobility, which can be examined by grasping the upper teeth and pulling the maxillary arch forward and inferiorly. Finger palpation for step-off deformities of the orbital rims, zygomatic arches, nasal bones, and frontozygomatic suture can help determine the site of fractures, although edema may make this difficult. The dermatome of V2 should be tested and documented. Extraocular movement and vision testing may demonstrate diplopia, indicating an entrapped inferior rectus muscle. Forced duction testing is performed by topically anesthetizing the conjunctiva with tetracaine drops, grasping the episcleral tissue in the fornix (near the inferior oblique insertion) with fine forceps, and testing the mobility of the globe for restriction that could indicate an impinged inferior oblique muscle in the orbital floor fracture. Facial nerve function should be assessed, especially when overlying lacerations are present. An ophthalmologic consult should be performed prior to fracture repair in all patients with periorbital fractures because findings such as retinal detachment or retrobulbar hematoma may preclude immediate surgery or obviate orbital decompression, respectively.
Imaging
As with any trauma patient, standard ABCs and cervical spine clearance (including C-spine films) should be the first priority. The widespread availability of maxillofacial CT scans with axial and coronal cuts makes plain film obsolete. Both axial and coronal cuts should be ordered to assess the orbital floor and diagnose the exact fracture sites. The pterygoid plates and zygomatic arches are best seen on axial films; the orbital rims, floor, and cribriform plate require coronal cuts. Subcutaneous air is often seen with medial orbital and orbital floor fractures. Foreign bodies or bone fragments near the optic nerve should be identified on CT to prevent damage during fracture reduction. The teardrop sign is seen in a coronal CT scan when orbital fat protrudes through a trap door orbital floor fracture. Indications for orbital floor fracture repair include a defect >1 cm3, muscle entrapment, and enophthalmos.
Treatment Options
Mildly displaced fractures can be managed with closed reduction. Moderate to severe ZMC fractures should be repaired with open reduction through a combination of approaches that may include transoral (to address the maxillary buttress), eyelid (orbital rim and floor), and upper blepharoplasty (frontozygomatic), or, less frequently, a bicoronal approach (associated supraorbital, frontal, or comminuted zygoma fractures). Fracture fixation usually includes plating at least one or two fracture sites for stability with 1.7-mm titanium plates (often L or J shaped) on the zygomaticomaxillary buttress and a 1.2-mm plate on the orbital rim and/or frontozygomatic suture. Orbital floor fractures are repaired by reduction of the herniated orbital contents through a transconjunctival approach. An implant such as titanium mesh or porous polyethylene is often used to maintain the reduction of orbital contents. Isolated zygomatic arch fractures can be reduced via a transoral, a temporal (Gilles), percutaneous, or, rarely, a coronal approach (comminuted fractures).
Complications
Increased intraocular pressure from an orbital hemorrhage can cause vision loss from the injury itself or as a complication of repair. Prompt treatment includes immediate lateral canthotomy and cantholysis, intravenous (IV) steroids (methylprednisolone), ophthalmology consult, and an urgent CT scan. Orbital decompression may be necessary. The most common complication of repair is inadequate fracture reduction with subsequent enophthalmos.
Outcome and Follow-Up
Standard perioperative antibiotics and steroids are used at the surgeon’s discretion. Strict precautions for no nose blowing should be enforced to prevent subcutaneous air.
ICD-9 Codes
802.4 | Closed fracture of malar and maxillary bones |
802.5 | Open fracture of malar and maxillary bones |
76.72 | Open reduction of malar and zygomatic fracture |
Further Reading
Costello BJ, Papadopoulos G, Ruiz R. Pediatric craniomaxillofacial trauma. Clin Pediatr Emerg Med 2005;6:32–40
Folkestad L, Westin T. Long-term sequelae after surgery for orbital floor fractures. Otolaryngol Head Neck Surg 1999;120(6):914–921
Kellman R. Maxillofacial trauma. In: Cummings CW, Haughey BH, Thomas JR, et al, eds. Otolaryngology Head and Neck Surgery. 4th ed. Philadelphia, PA: Elsevier Mosby; 2005:602–639
Stanley RB Jr. Use of intraoperative computed tomography during repair of orbitozygomatic fractures. Arch Facial Plast Surg 1999;1(1):19–24
Stewart MG. Zygomatic complex fractures. In: Stewart MG. Head, Face, and Neck Trauma: Comprehensive Management. Stuttgart/New York: Thieme: 2005:68–76
7.1.4 Frontal Sinus Fractures
Key Features
• Frontal sinus fractures represent 5–15% of all craniomaxillofacial fractures.
• A frontal sinus fracture is the third most common facial fracture.
• Its primary cause is high-velocity blunt force found in motor vehicle accidents (60–70% of frontal sinus fractures) and assault.
• These fractures encompass simple nondisplaced anterior table fractures to comminuted ones involving brain injury and CSF leak.
The two sinuses (rarely, one) are housed completely within the frontal bone, if present. Displaced frontal sinus fractures may result in forehead deformities and traumatic injury to the brain. The frontal bone forms the upper facial skeleton and is closely related to the brain. The orbit lies inferolaterally; the dura, cribriform plate, and frontal lobes of the brain lie posteriorly. The sinus outflow tracts communicate with the nose below. The sinus is made up of the anterior and posterior tables. The frontal bone has the highest tolerance of direct blunt force, with the anterior table typically able to withstand 800 to 2200 lb of force. Because of its greater thickness compared with the posterior wall, a force strong enough to fracture the anterior table will usually fracture the posterior table and cause damage to the outflow tracts. The complications of fractures can include deformity, mucocele, brain abscesses, and meningitis.
Epidemiology
Most frontal fractures occur in young males at a higher proportion when compared with women (8:1). Although they can occur at any age, the highest incidence occurs during the third decade of life.
Clinical
Signs and Symptoms
Patients with frontal sinus fractures frequently have other associated facial fractures. Depending on the degree of force, patients may or may not have been conscious during the event and may have suffered significant head trauma. Those who are conscious during the inciting event and remain so will likely complain of frontal pain. Forehead swelling, lacerations, and paresthesia may also be present. Obvious forehead deformity may be present, including significant depression, step-offs, and palpable crepitus, but typically the diagnosis is best characterized via a CT scan. CSF discharge may also be evident from the nose or wound.
Differential Diagnosis
Frontal sinus fractures should be distinguished from simple lacerations and contusions of the forehead. Frontal bone fractures can occur without involvement of the sinus, and CSF rhinorrhea is also seen in other isolated facial fractures. Adjacent facial structures must be evaluated for traumatic involvement (zygomaticomaxillary, orbital, NOE, and skull base fractures).
Evaluation
Physical Exam
The trauma ABCs must be assessed first. Swelling of the oral cavity and pooling of blood in the pharynx can complicate facial trauma by causing airway obstruction. An airway should always be established immediately. Neurologic and visual status evaluation should be done as soon as potentially life-threatening injuries are addressed. Vision loss may be prevented if recognized early via elevated intraorbital pressure or evidence of optic nerve injury. If a patient is either uncooperative or combative, gross evaluation of the facial nerve is recommended when a complete exam is unobtainable. Mobility of the midface, nose, and mandible should be assessed adequately. Lacerations need to be thoroughly irrigated and probed for evidence of any foreign body. CSF rhinorrhea or otorrhea should be considered if any clear discharge is present.
Imaging
All patients with suspected frontal sinus fractures should undergo a fine-cut (1.5–3 mm) CT scan in axial and coronal planes. Axial images will allow good visualization of the anterior and posterior tables of the frontal sinus as well as of evidence of pneumocephalus. Coronal views allow for visualization of the frontonasal tract, the cribriform plate, and the floor of the frontal sinus. In general, a displacement of the posterior table of more than one thickness of adjacent bone is considered significant.
The role of x-rays is limited, although Caldwell’s view can evaluate resolution of fluid accumulation that may be found in the frontal sinus postinjury.
Labs
No specific laboratory tests are required for these patients; however, appropriate screening tests (CBC, chemistry, coagulation studies, drug screening) are often obtained during the initial trauma evaluation and may identify conditions warranting treatment.
Other Tests
When CSF rhinorrhea is suspected, β-2 transferrin testing may be performed on the nasal fluid to confirm the diagnosis. Frontonasal outflow tract obstruction is associated with development of frontal mucoceles, and, although typically best evaluated intraoperatively. Fluorescein, benzylpenicillin solution (white), or methylene blue dye is sometimes used to evaluate the integrity of the nasofrontal duct. Patency is evident when dye is seen intranasally after being introduced in the sinus.
Treatment Options
Antibiotic prophylaxis is recommended for frontal sinus fractures, although some argue that closed fractures and those isolated to a nondisplaced anterior table fracture are not in need of antibiotics. The evaluation of the patients should be directed at an assessment of whether the dura needs to be repaired, whether the outflow tracts have remained sufficiently functional, and whether there is a significant deformity. The concepts of importance in frontal sinus fracture repair are prevention of intracranial infection, prevention of frontal sinus disease such as sinusitis and mucoceles, and a cosmetically acceptable outcome.
Nondisplaced fractures of the anterior table without evidence of nasofrontal duct obstruction and no forehead deformity should be treated nonoperatively. Apart from this fracture, there is no apparent consensus regarding treatment.
The management of frontal sinus injury is evolving, but the goals as listed above have been fairly constant. The management options may include sinus reconstruction and preservation, cranialization of the sinus, and obliteration. The goal is to preserve sinus physiology and consider that the patient will have to be followed closely with serial imaging. Preservation is usually considered in patients with more limited injuries and CT evidence of patent outflow tracts. Cranialization is performed when there has been comminution of the posterior table that necessitates dural repair, and damage to the outflow tracts. Cranialization involves removal of the posterior table of the sinus, removal of the sinus mucosa, and obliteration of the outflow tracts. Obliteration of the sinus is performed in similar situations as cranialization, but rather than removing the posterior table of the sinus, the surgeon “obliterates” the sinus cavity with fat or other biologic material.
Surgical access for frontal sinus fracture is best made with a bicoronal flap approach, supraorbital brow incision, or via an existing laceration. Minimally fragmented and nonfragmented fractures can be sufficiently reduced with miniplates. Technological advancement now allows for the use of endoscopic assistance to avoid external scars and frontal sinus fat obliteration by endoscopically opening the nasofrontal outflow tract widely and permanently.
Complications
Complications may include injury to sensory or motor nerves. It is essential to document nerve function prior to surgery. Most patients with sensory change will see improvement over 3 to 12 months. Prolonged retraction can cause temporary paresis of this branch of the facial nerve, but precise surgical technique can help to avoid permanent injury.
Outcome and Follow-Up
The patient is admitted after surgery and monitored for neurologic change, infection, CSF leak, visual change, hemorrhage, and pain control. The patient should be followed closely for the first several months with particular attention paid to follow-up CT to evaluate for mucocele development. The time frame for mucocele development can range from 2 months to 42 years; thus long-term follow up, though difficult, is paramount.
ICD-9 Code
800 | Fracture of vault of skul |
Further Reading
Bell RB, Dierks EJ, Brar P, Potter JK, Potter BE. A protocol for the management of frontal sinus fractures emphasizing sinus preservation. J Oral Maxillofac Surg 2007;65(5):825–839
Cole P, Kaufman Y, Momoh A, et al. Techniques in frontal sinus fracture repair. Plast Reconstr Surg 2009;123(5):1578–1579
Cummings CW, Haughey BH, Thomas JR, et al, eds. Otolaryngology Head and Neck Surgery. 4th ed. Philadelphia, PA: Elsevier Mosby; 2005
Gossman DG, Archer SM, Arosarena O. Management of frontal sinus fractures: a review of 96 cases. Laryngoscope 2006;116(8):1357–1362
Lalwani AK. Current Diagnosis and Treatment: Otolaryngology Head and Neck Surgery. 2nd ed. New York: McGraw-Hill; 2007
Strong EB. Frontal sinus and naso-orbital-ethmoid complex fractures. In: Papel ID, ed. Facial Plastic and Reconstructive Surgery. 3rd ed. Stuttgart/New York: Thieme; 2009:977–990
7.1.5 Midface Fractures
Key Features
• Midface fractures typically result from high-energy blunt trauma, such as motor vehicle accidents and altercations.
• The mass, density, and speed of the striking object will affect the type and the severity of the facial injury.
• Suspect associated ocular, intracranial, and cervical spine injuries.
The midface transmits masticatory forces to the skull base through a series of three vertical pillars, or buttresses, of thickened bone: the zygomaticomaxillary (lateral), nasomaxillary (medial), and pterygomaxillary (posterior) buttresses (Fig. 7.1). These three buttresses are essential for proper facial form and function. Damage to the midface may be life-threatening.
Proper realignment of the vertical buttresses is critical in establishing premorbid dental occlusion, facial height, and projection. Proper alignment of the orbital rims and maxillary alveolus (palatal fractures) is essential for establishing facial width, while the zygomatic arches play a key role in restoring both facial projection and width.
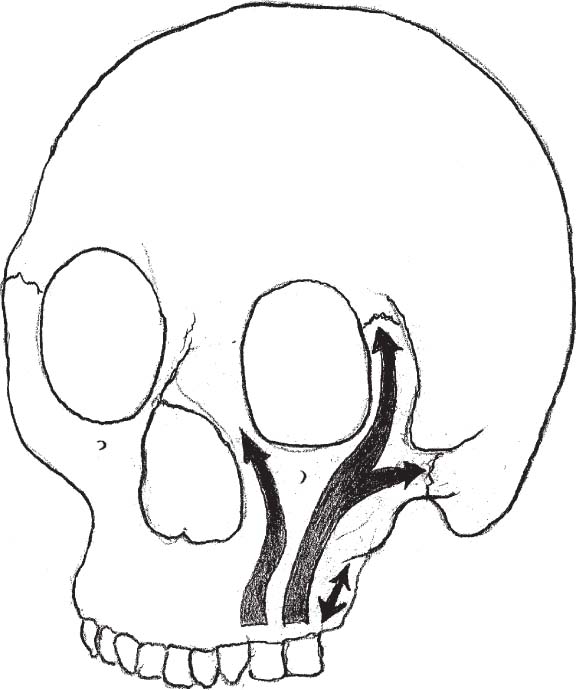
Fig. 7.1 Masticatory forces are transmitted through the zygomaticomaxillary (lateral), nasomaxillary (medial), and pterygomaxillary (posterior) buttresses to the skull base. (From Stewart MG. Head Face and Neck Trauma: Comprehensive Management. Stuttgart/New York: Thieme; 2005:78.)
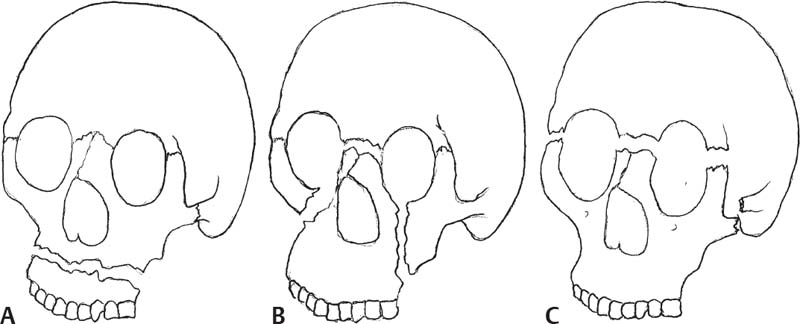
In 1901, René Le Fort described three predominant types of midface fractures (Fig. 7.2), which he classified as follows:
• LeFort I fractures (horizontal) extend above the dental apices from the zygomaticomaxillary buttress through the nasomaxillary buttress, pyri-form aperture, and nasal septum.
• LeFort II fractures (pyramidal) extend through the zygomaticomaxillary buttress, inferior orbital rim and orbital floor, the frontal process of the maxilla, and through the nasofrontal suture.
• LeFort III fractures (aka craniofacial disjunctions) follow a fracture pattern extending from the nasofrontal suture along the medial orbital wall, then traversing the orbital floor and lateral wall before extending through the zygomaticofrontal suture and zygomatic arch.
Epidemiology
Most midface fractures occur in young males and account for some 6–25% of facial fractures.
Clinical
Signs and Symptoms
Patients typically present with a history of traumatic facial injury and may complain of pain, malocclusion, trismus, hypoesthesia, or diplopia. Examination often reveals periorbital ecchymosis, facial and oral mucosal edema, facial asymmetry, epistaxis, mobility of the midface, malocclusion (anterior open-bite deformity), or dental injury. Less commonly, CSF rhinorrhea and changes in visual acuity or restriction of extraocular motion are observed. Airway distress associated with severe injuries and decreased level of consciousness associated with intracranial injury may also be present.
Differential Diagnosis
Malocclusion is also seen in isolated dentoalveolar fractures. Adjacent facial structures must also be evaluated for traumatic involvement (mandible, zygomatico-orbital, nasoethmoid, frontal sinus, and skull base fractures).
Evaluation
Physical Exam
As with all trauma patients, the initial evaluation should include a detailed systemic examination using the advanced trauma life support protocol, and then a complete head and neck examination is performed. Airway compromise secondary to mucosal trauma and edema or profuse hemorrhage is possible, and the airway must be secured. The patient’s facial region should be thoroughly inspected and palpated for any bony step-offs. Midface mobility is assessed by applying traction to the maxillary central incisors and alveolus with one hand while stabilizing the forehead with the other. All teeth should be accounted for, and if any are fractured or missing, a chest radiograph should be performed to make sure the missing teeth did not enter the airway. A complete cranial nerve examination is critical. In the midface, injury to the maxillary division of the trigeminal nerve is common and facial nerve injury is also possible. Any deficits are documented prior to surgery. Visual acuity and extraocular motion are evaluated and ophthalmologic consultation obtained if these are abnormal or if ocular injury is suspected. Intranasal examination should assess for septal hematoma, septal perforation, and CSF rhinorrhea.
Imaging
All patients with suspected midfacial fractures should undergo a fine-cut (1.5–2 mm) CT scan in axial and coronal planes. High-quality reformatted coronal images are acceptable when cervical immobilization prevents direct coronal imaging. Traditional radiographs such as a Waters view are of historic interest only and should not be used for diagnosis and treatment planning. Many surgeons now routinely obtain CT images immediately postoperatively to confirm anatomic reduction and plating of the fractures. This is extremely useful in panfacial or comminuted fractures.
Labs
No specific laboratory tests are required for this patient population; however, appropriate screening tests (CBC, chemistry, coagulation studies, drugscreening) are often obtained during the initial trauma evaluation and may identify conditions warranting treatment.
Other Tests
When CSF rhinorrhea is suspected, B-2 transferrin testing should be performed on the nasal fluid to confirm the diagnosis.
Treatment Options
The goal of treatment is restoration of preinjury function and facial aesthetics. Treatment within the first 7–14 days of injury allows tissue edema to subside and lessens the likelihood of aesthetic and functional deficits that are challenging to correct after delay.
Medical
Midface fractures that are nondisplaced, stable, and accompanied by normal occlusion can be observed, but the mainstay of treatment for all other midface fractures is surgical.
Surgical
Historically, midfacial fractures were managed with a prolonged course of maxillomandibular fixation (MMF) and/or suspension wires. Continued mobility of the fracture lines with this type of treatment led to a high incidence of residual bony and soft tissue deformity. As such, the standard treatment for displaced, mobile, or comminuted midface fractures is now open reduction and internal fixation.
Operative treatment begins with exposure of all fracture lines using surgical approaches that may include gingivolabial (maxillary face and buttresses), transconjunctival, or subciliary (orbital rim and floor), upper blepharoplasty (zygomaticofrontal and zygomaticosphenoid sutures), and coronal (zygomatic arches, frontal bone, and nasoethmoid area) incisions. The maxilla is next disimpacted and proper occlusion reestablished with MMF. Inquiry should be made as to preinjury malocclusion or orthodontic/orthognathic treatment. Internal fixation with titanium miniplates is performed along the medial and lateral buttresses and along the inferior orbital rims, zygomaticofrontal sutures, zygomatic arches, and glabellar region as indicated. Consideration should be given to primary bone grafting when interfragmentary gaps >5 mm are present. Miniplates (typically 1.5–2.0 mm) are used for medial and lateral buttresses. Microplates (1.0–1.3 mm) are used on the inferior orbital rim, and the zygomaticofrontal suture is treated with 1.3- to 1.5-mm plates. Although rigid or semirigid plating has greatly improved our ability to treat these injuries, the surgeon must be meticulous in achieving correct anatomic reduction and use exacting technique when adapting the plate to the bone to avoid “fixing” the patient in the wrong position. Most patients are released from MMF at the conclusion of surgery, although arch bars may be left in place for guiding elastics (occasionally useful with severe edema).
Complications
Complications may include injury to sensory or motor nerves. It is essential to document nerve function prior to surgery. Most patients with sensory change will see improvement over the next 3–6 months. Temporary paresis of the temporal branch of the facial nerve may be seen if prolonged retraction during a coronal approach is required, but with careful exposure and surgical technique, permanent injury is rare.
Malocclusion should be noted postoperatively and surgical technique reviewed. CT may be helpful in determining the cause of the malocclusion, and if fractures malalignment is noted, reexploration should be considered with repeat reduction and plating prior to fracture union. Guiding elastics may assist in very minor dental malocclusions but cannot correct grossly malaligned fractures.
Lower eyelid malposition is largely avoided with gentle tissue handling and meticulous surgical technique. Ectropion is more common after trans-cutaneous than transconjunctival approaches, though entropion may be observed after transconjunctival approaches (rare). Massage is useful in the postoperative period if lower eyelid retraction is noted. More severe malpositions may require surgical intervention.
Other incisional problems include dehiscence, local infection, hypertrophy, and alopecia and are treated as indicated.
Outcome and Follow-Up
The patient is admitted after surgery and monitored for airway status, visual change, hemorrhage, and pain control. Intermittent ice application is useful in decreasing edema, as is elevation of the head of the bed. The patient is instructed in oral hygiene consisting of frequent mouth rinses and gentle brushing, especially after meals. Diet should consist of soft foods for approximately 6 weeks and then a normal diet may be resumed. Cutaneous sutures are removed 5–7 days after surgery. Intraoral incisions are closed with resorbable sutures and do not require removal.
The patient should be followed closely for the first several weeks, with particular attention given to occlusal status and eyelid position. Long-term follow-up should also be scheduled, but this is sometimes challenging in this patient population.
ICD-9 Codes
802 | Fracture of face bones |
802.4 | Closed fracture of malar and maxillary bones |
802.5 | Open fracture of malar and maxillary bones |
802.9 | Open fracture of other facial bones |
804 | Multiple fractures involving skull or face with other bones |
Further Reading
Doerr TD, Mathog RH. Le Fort fractures (maxillary fractures). In: Papel ID, ed. Facial Plastic and Reconstructive Surgery. 3rd ed. Stuttgart/New York: Thieme; 2009:991–1000
Frodel JL, Marentette LJ. The coronal approach: anatomic and technical considerations and morbidity. Arch Otolaryngol Head Neck Surg 1993;119:201–207
Gruss JS, Mackinnoh SE. Complex maxillary fractures: role of buttress reconstruction and immediate bone grafts. Plast Reconstr Surg 1986;78:9–22
Kelly KJ, Manson PN, Vander Kolk CA, et al. Sequencing LeFort fracture treatment (organization of treatment for a panfacial fracture). J Craniofac Surg 1990;1:168–178
Klotch DW, Gilliland R. Internal fixation vs. conventional therapy in midface fractures. J Trauma 1987;27:1136
Manson PN, Hoopes JE, Su CT. Structural pillars of the facial skeleton: an approach to the management of Le Fort fractures. Plast Reconstr Surg 1980;66:54–61
Marchena JM, Johnson JV. Le Fort and palatal fractures. In: Stewart MG, ed. Head Face and Neck Trauma. New York: Thieme; 2005:77–85
7.1.6 Mandible Fractures
Key Features
• Mandible fractures may be found with a history of trauma.
• Pain with or without mastication may be an indication.
• Evaluate concomitant intracranial, airway, and/or cervical spine injury.
• Account for missing teeth.
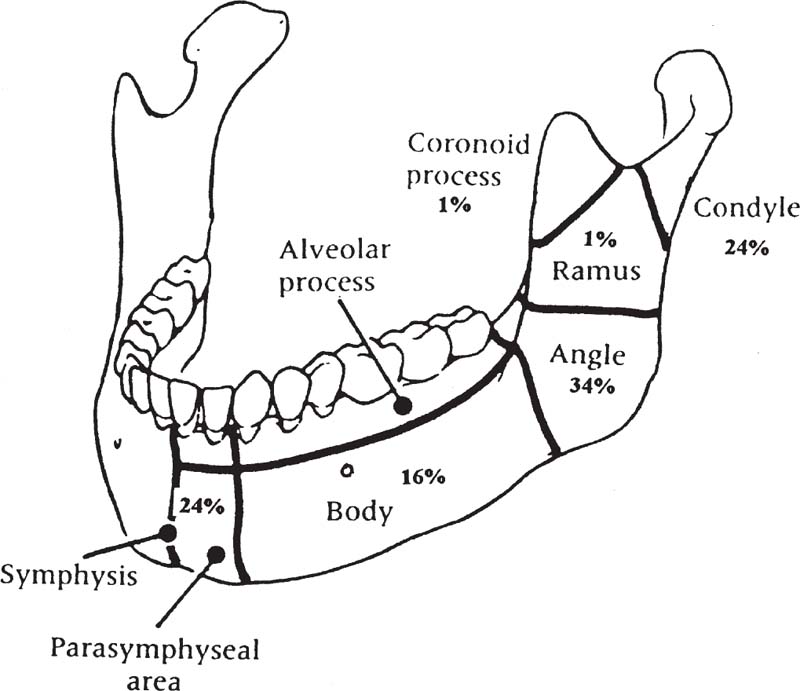
Mandible fractures are common after facial trauma, occurring second only to fractures of the nasal bones. Diagnosis can often be made by clinical exam, although confirmatory x-ray evaluation is required. Fractures often traverse the alveolus, creating intraoral communication with the fracture site, which leads to contamination of the fractures by oral flora. Early initiation of both systemic antibiotics as well as oral rinses should decrease the risk of infection. Repair is aimed at restoring the occlusion, reestablishing anatomic alignment of the bone fragments, and ensuring healing with minimal morbidity. Mandible fractures are classified as favorable or unfavorable for healing (Fig. 7.3).
Epidemiology
Most mandible fractures are the result of interpersonal trauma and motor vehicle accidents; they typically occur in the third and fourth decades of life. In the elderly, falls become a more common cause, and in younger children sports activities and motor vehicle accidents are most prevalent. Most studies indicate that the condylar/subcondylar complex is most frequently fractured, followed by the symphyseal region from canine to canine (Fig. 7.4). The mandibular angle region is next, followed by the body region. Fractures of the vertical ramus (excluding subcondylar fractures) occur less frequently, and coronoid process fractures are distinctly uncommon. There is some controversy regarding location frequency.

Clinical
Signs
Note the presence of malocclusion, with or without trismus. Edema and ecchymosis may be seen both intraorally and extraorally. Loose or fractured teeth should be identified, and attempts should be made to account for missing teeth (intruded teeth may occasionally be mistaken for avulsions). Intraoral lacerations are common at fracture sites. Paresthesia over the chin indicates injury to one or both inferior alveolar nerves.
Symptoms
Most patients with mandible fractures present because of pain or malocclusion, both of which tend to interfere with eating. Some notice oral bleeding and facial swelling. They may also complain of loose teeth.
Differential Diagnosis
If the patient is (or was) unconscious, the nature of the trauma may be difficult to determine. Swelling and muscle injury may masquerade as a fracture. A patient with a serious dental infection, with or without a history of trauma, may have clinical findings of pain, trismus, and malocclusion, which may make it difficult to determine whether a fracture is present.
Evaluation
Physical Exam
Examine for swelling, tenderness, and ecchymosis. Warmth and fever would be signs of infection, usually seen when presentation is delayed. Examination of the mandible itself might reveal mobility of fragments (to bimanual palpation), trismus, and malocclusion. Also look for loose, cracked, avulsed, and/or impacted teeth.
Imaging
Best results will be obtained if plain films, orthopantomogram (Panorex), and CT scans are obtained.
Labs
CBC is indicated to look at hemoglobin if there has been significant bleeding and to look at the white blood cell (WBC) count if presentation is delayed. Coagulation studies should be obtained if the patient has medical comorbidities.
Pathology
Pathology studies are generally not applicable, unless there is a concern about a pathologic fracture in a patient with another underlying disease, or in a case of delayed management or complications of prior management, where there may be concern for posttraumatic mandibular osteitis or osteomyelitis.
Treatment Options
Medical
Nondisplaced, nonmobile fractures without malocclusion can be managed nonsurgically. The patient is maintained on a mechanical soft diet. The patient should be seen after 1–2 weeks to ensure patient compliance and that the fracture is healing uneventfully. Any change in occlusion status will require additional treatment. The occlusion class is based on the relationship of the retrobuccal cusp of the upper first molar to the buccal groove of the lower first molar:
• Class I occlusion (normal): The mesiobuccal cusp of the maxillary first molar occludes exactly with the mandibular first molar buccal groove.
• Class II occlusion: The mesiobuccal cusp is mesial or anterior to the mandibular first molar buccal groove.
• Class III occlusion: The mesiobuccal cusp is distal to the buccal groove.
Subcondylar fractures with minimal displacement and without malocclusion may be managed with physiotherapy and exercises.
For both of the above situations, mouth-opening exercises are important to prevent limitations in mouth opening.
Relevant Pharmacology
Antibiotic prophylaxis is recommended from the time of presentation until oral wounds have sealed after the repair. (Precise duration of antibiotic treatment after fracture repair is controversial.) An antibiotic that covers common oral flora is recommended.
Surgical
There are three basic surgical approaches to mandible fractures: (1) placement of oral appliances and application of rigid MMF (also called closed reduction, rigid fixation); (2) placement of oral appliances and the use of training elastics (nonrigid MMF; also called nonrigid closed reduction); and (3) open reduction of the fractures, generally used with rigid fixation of the fragments (also called open reduction and internal fixation or ORIF).
ORIF may be performed via either intraoral or extraoral approach. “Load-sharing” repairs are generally used when the bone being repaired is solid enough to provide a buttress, so that fixation can be placed in a biomechanically advantaged fashion that takes advantage of the naturally occurring forces of muscle function and mastication. This can be accomplished using the “Champy” technique, with miniplates placed along the “ideal line of osteosynthesis,” using monocortical screws to avoid injury to tooth roots and the inferior alveolar nerve. Two plates or two lag screws are generally used in the symphyseal and parasymphyseal regions, a single plate is commonly used along the mandibular body, and one or two plates (the choice is controversial) are used for angle fractures. Compression plates can be used as well along the symphysis and body (not at the angle), but this requires bicortical screws placed along the inferior border, so tension band plates or arch bars must be applied to avoid distraction of the alveolar portion of the fracture.
“Load-bearing” repairs are used when there is inadequate bone to form a buttress and share in the load. This requires the placement of longer, stronger reconstruction plates fixed with bicortical screws along the inferior border of the mandible. At least three and preferably four screws should be placed on either side of the fracture. Load-bearing reconstruction plate repairs are indicated to span areas of mandibular deficiency, such as defects, areas of comminution, atrophic mandibles (edentulous patients), and areas involved with infection (or previous nonunion). The reconstruction plate is also a fallback technique for any mandible fracture, particularly in the angle region after loss of an impacted third molar. Fractures of the condylar neck should be opened if there is significant foreshortening of the ramus of the mandible or persistent malocclusion. The endoscopic approach allows a mostly transoral repair of selected subcondylar fractures. Open reduction of condylar head fractures remains quite controversial.
Complications
A rigidly fixed malreduction should be reoperated, unless there are extenuating circumstances because MMF cannot repair this. Wound infections should be drained and managed expectantly. Loose hardware must be removed. Failure of fixation requires reoperation, and if infection has developed, a stronger, load-bearing repair will be necessary. Nerve injuries (motor and sensory) should be documented.
Outcome and Follow-Up
Routine wound care is indicated. Oral hygiene must be maintained, and antiseptic oral rinses are commonly used several times daily and after meals. A liquid diet is preferred initially, and this is advanced to a mechanical soft diet as tolerated. Postoperative x-rays should be obtained to ensure satisfactory reduction of fractures. If satisfactory rigid fixation has been accomplished, MMF will not be necessary. After 1 week, trismus should be treated with mouth-opening exercises. Patients treated with rigid MMF are generally sent to the floor and discharged with wire cutters, in case they need to urgently release the MMF.
Patients should be followed closely for the first 6 weeks. At this point, most fractures are stable enough to allow removal of the arch bars. After this, patients should be followed until normal function is ensured.
ICD-9 Codes
802.20 | Fracture mandible |
802.25 | Angle |
802.3 | Open |
802.30 | Open Upper – see Fracture, maxilla |
802.20 | Mandible (closed) |
802.25 | Angle |
802.35 | Open |
802.28 | Body |
802.27 | Alveolar border |
802.37 | Open |
802.38 | Open |
802.26 | Symphysis |
802.36 | Open |
802.21 | Condylar process |
802.31 | Open |
802.23 | Coronoid process |
802.33 | Open |
802.29 | Multiple sites |
802.39 | Open |
802.30 | Open |
802.24 | Fracture; mandible, closed; ramus unspecified |
802.34 | Open |
802.22 | Subcondylar |
802.32 | Open |
Further Reading
Costello BJ, Papadopoulos G, Ruiz R. Pediatric craniomaxillofacial trauma. Clin Pediatr Emerg Med 2005;6:32–40
Davidson J, Nickerson, Nickerson B. Zygomatic fracture: complications of methods of internal fixation. Plast Reconstr Surg 1990;86:25–32
Johnson JV. Mandibular structures: symphysis, body, and angle. In: Stewart MD. Head, Face, and Neck Trauma: Comprehensive Management. Stuttgart/New York: Thieme; 2005:207–116
Kellman R. Maxillofacial trauma. In: Cummings CM. Otolaryngology Head and Neck Surgery. 4th ed. Philadelphia: Mosby; 2005:602–639
Stanley RB Jr. Use of intraoperative computed tomography during repair of orbitozygomatic fractures. Arch Facial Plast Surg. 1999;1:19–24
7.2 Facial Reanimation and Eye Care
Key Features
• No one modality is universally appropriate for all afflictions of facial nerve function.
• Etiology of the paralysis, oncologic status, type of injury, and location of injury all contribute to the selection of the most appropriate reanimation methods.
• Reanimation techniques are classified into four types: neural methods, musculofascial transpositions, facial plastic procedures, and prosthetics.
For patients with facial nerve injuries, realistic expectations must be established at the initial encounter and candidly discussed between the physician and the patient and his or her family. Several points should be emphasized to the patient before the onset of treatment. First, no reanimation technique will restore the face exactly to its preparalyzed condition. The patient should understand that despite the most meticulous surgery some degree of synkinesis and residual weakness may persist. It is also important to stress that the results of these reanimation techniques may be augmented by physical therapy and rehabilitation.
Location of Facial Nerve Injury
Intracranial
Intracranial nerve injuries most commonly occur during resection of acoustic neuroma or other cerebellopontine angle (CPA) tumors. The incidence of facial nerve injury following CPA tumor surgery is reported to be 2.3%. In the event of facial nerve injury during CPA tumor surgery, immediate repair by either direct anastomosis or graft is advisable. If added length is needed, careful rerouting of the tympanic and mastoid segments of the nerve may add enough length for an end-to-end anastomosis.
Intratemporal
Intratemporal facial nerve injury is usually encountered in patients following external head trauma with skull base fractures, or iatrogenic injury during or following otologic surgery. Most temporal bone fractures result from motor vehicle accidents and violent encounters. Seven to 10% of these fractures result in facial nerve dysfunction. In temporal bone trauma, facial nerve injury most often occurs in the perigeniculate and labyrinthine sections, with axonal degeneration extending a variable distance in both directions. Management of facial nerve injury following temporal bone trauma is controversial. Most patients who present with complete paralysis at the time of injury have a poorer prognosis than those with incomplete or delayed paralysis.
Extratemporal
Extratemporal injury to the facial nerve may occur during parotid surgery, temporomandibular joint procedures, or facelift procedures, or following traumatic lacerations of the face. The incidence of facial nerve paralysis after uncomplicated parotid procedures is reported at 20% for temporary palsy and 10% for permanent paresis of either the temporal or mandibular branches. Patients at higher risk for facial nerve injury during parotid surgery include children and those undergoing a total parotidectomy. Inadvertent transection of the nerve that is recognized during parotid surgery should be repaired as soon as possible.
Reanimation Options
The order of preference for restoration of function following total unilateral facial paralysis is as follows:
1. Spontaneous facial nerve regeneration (observation)
2. Facial nerve neurorrhaphy (facial nerve anastomosis)
3. Interpositional graft
4. Nerve crossovers (anastomosis to other motor nerves)
5. Muscle transfer
6. Eyelid procedures and prosthetics
Facial Nerve Neurorrhaphy
If the nerve has been completely disrupted, direct neurorrhaphy is the most effective way to reanimate the paralyzed face. The interrupted neural pathway can be reestablished either by direct anastomosis or by inserting a graft between the disrupted segments. Some of the key points in nerve repair are early identification, evaluation of nerve condition, and tension-free anastomosis. The best time to perform surgery is within the first 72 hours, before degeneration has occurred and while the distal nerve can still be stimulated. The disrupted nerve should be approximated with minimal tension. It may be necessary to reroute the nerve within the temporal bone or to gain extra length by releasing the nerve. Factors that influence the success of repair include tension, the character of the wound, the presence of scar tissue, and time lag to repair.
The surgical suturing technique for nerve repair requires magnification, either with loupes or a surgical microscope. The nerve endings should be freshened with a new scalpel blade. At this point, axoplasm may be seen oozing from the proximal stump. Number 8-0 to 10-0 nylon sutures with a 75- or 100-micron needle should be used.
If possible, three or four simple sutures should be placed about the circumference of the epineural layers to achieve adequate union (Fig. 7.5).
Interpositional Graft
In cases where patients have undergone prior surgery or have had part of their facial nerve sacrificed or avulsed as a result of severe trauma, directnerve repair is impossible and interposition of a nerve graft is required. This technique is reserved for cases in which direct nerve repair would result in excess tension or when there is loss of nerve tissue.
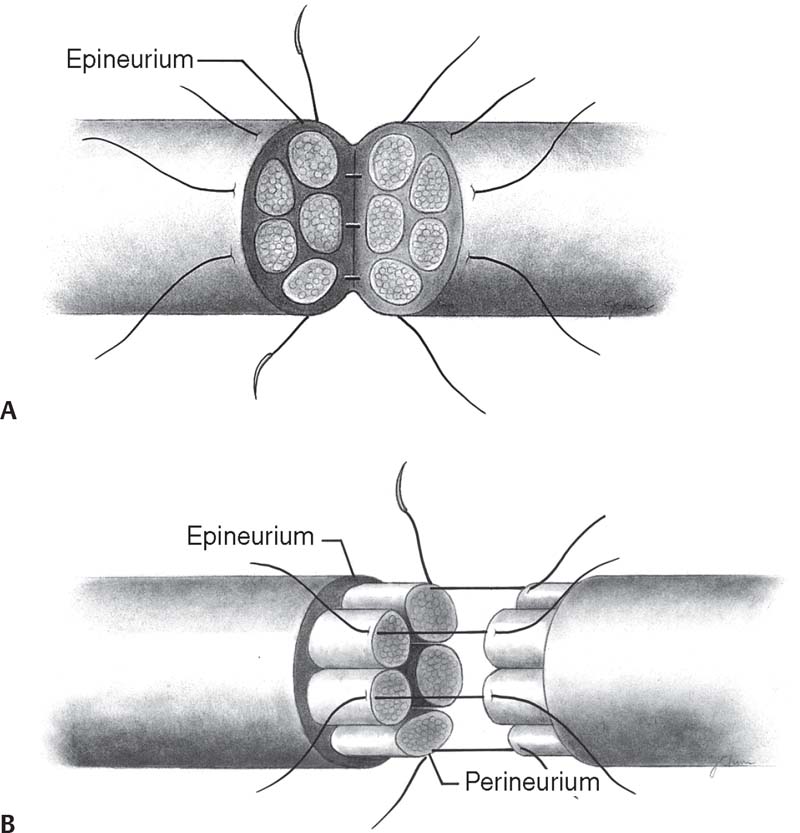
Fig. 7.5 (A) Epineural nerve repair. (B) Perineural (fascicular) repair. (From Burgess LPA, Goode RL. Reanimation of the Paralyzed Face. Stuttgart/New York: Thieme; 1994:13–16.)
The greater auricular nerve is the most commonly used donor nerve especially when the nerve graft required is small. Its advantages are its proximity to the operative field and ease of exposure (Fig. 7.6). It should be remembered that oncological considerations mandate that the ipsilateral nerve not be used. If more nerve tissue is required, the sural nerve may be harvested.
Nerve Crossovers
This technique is used when direct suturing or cable grafting is not feasible as is often the case after removal or obliteration of proximal or intratemporal portions of the facial nerve. It is particularly useful to treat facial paralysis resulting from intracranial or intratemporal disorders or surgery. These techniques are relatively simple and require one suture line. They provide a powerful source for reinnervation although the results are not always consistent or predictable. Nerve crossovers most commonly utilize the hypoglossal nerve.
Another technique is the “babysitter graft.” In this technique, the hypoglossal nerve and facial nerve are anastomosed with the interposition of a free nerve graft, end-to-end to the peripheral facial nerve stump, and end-to-side to the hypoglossal nerve. This technique is typically used in candidates for cross facial nerve grafting.
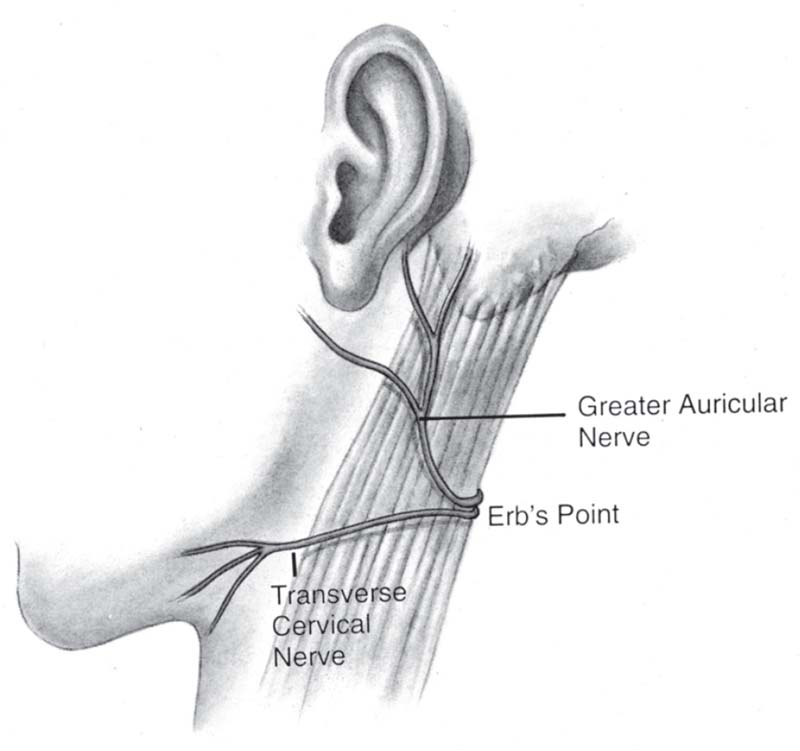
Fig. 7.6 Greater auricular and transverse cervical nerve grafts. (From Burgess LPA, Goode RL. Reanimation of the Paralyzed Face. Stuttgart/New York: Thieme; 1994:18.)
Cross Facial Nerve Grafting
This technique uses the contralateral normal facial nerve to innervate certain facial muscles on the paralyzed side. This technique should be considered an alternative to hypoglossal or accessory nerve grafting. It should not be performed as long as spontaneous regeneration is still possible or in cases in which direct or cable grafting of the facial nerve is possible.
Muscle Transfer Techniques
Muscle transfer techniques are used when neural techniques are unsuitable. Patients with long-standing facial paralysis (>3 years) are unlikely to benefit from any of the previously discussed reanimation procedures. Severe fibrosis occurs in the distal neuromuscular unit along with atrophy of the facial musculature making reinnervation unlikely.
Regional Muscle Transfer
Muscle transfer techniques entail transplanting a new neuromuscular unit into a region of the paralyzed face. This may be done in conjunction with a nerve graft or a crossover implanted in the transferred muscle. The two basic techniques to accomplish this are regional muscle transposition and a free-muscle transfer.
Regional muscle transfer is usually used to reanimate the lower third of the paralyzed face. The new neuromuscular unit is composed of the transposed muscle with its original nerve supply. Muscles available for these procedures include the masseter, temporalis, and digastric. It should be remembered that in all muscle transfer procedures, overcorrection is desired.
Free-Muscle Transfer
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


