On the other hand, delayed surgical intervention in these children may lead to permanent structural damage to the eye, causing irreversible macular pathology and optic nerve pathology that will limit any future postsurgical ability of achieving a good visual outcome. Delayed intervention also may result in visual loss from amblyopia and strabismus in this patient population. There is a point in the course of the disease where the benefits of surgery outweigh the risks.
The essential element for a successful surgery is careful control of inflammation. Details on control of inflammation during and after surgery are given under specific surgical sections that follow. It is important to work closely with a pediatric ophthalmologist to manage and reduce possible amblyopia. The age of the child at the time of surgery, the presence or absence of amblyopia, and the presence of irreversible retinal or optic nerve pathology are the primary factors influencing the outcome of surgery in the pediatric uveitic patient.
This chapter first discusses diagnostic surgical procedures that may be indicated in the pursuit of the diagnosis of uveitis. The chapter then discusses some of the many therapeutic surgical procedures that are used to treat the complications of uveitis that occur in a recurrent or chronically inflamed eye. The chapter finishes with specific surgical approaches to a few of the more common pediatric uveitides, such as ocular toxocariasis, sarcoidosis, intermediate uveitis, and juvenile rheumatoid arthritis (JRA)–associated uveitis.
Diagnostic surgery may be necessary to arrive at the underlying diagnosis of uveitis. Pursuing a diagnosis is helpful in understanding the natural history of the disease and potential complications of the disease. A surgical procedure for diagnosis is reasonable if (i) noninvasive studies have been performed and have failed to disclose the underlying cause of the patient’s uveitis, (ii) the patient is unresponsive to medical therapy and alternative diagnoses are being considered, (iii) the patient develops significant ocular or systemic complications during therapy and more diagnostic information is needed to guide therapy, or (iv) malignancy is suspected.
Anterior Chamber Paracentesis
Indications
Anterior chamber paracentesis is an easily performed technique that provides a small amount of aqueous humor for analysis. In the inflamed eye, the breakdown of the blood–eye barrier results in antibody titers and immunoglobulin concentrations in the aqueous humor that may be higher than normal. Thus, samples of both aqueous humor and serum must be obtained on the same day for simultaneous measurement of immunoglobulin and antibody to control for the increased aqueous humor values from diffusion from breakdown of blood–eye barriers. The Goldmann-Witmer coefficient is used to help us reasonably conclude whether there is a localized antibody production in the eye ( Fig. 55.1) (6).
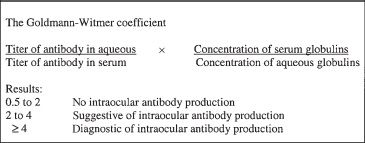
FIGURE 55.1 Goldmann-Witmer coefficient
Procedure
The anterior chamber is entered at the limbus with a 30-gauge needle on a tuberculin syringe, and about 0.2 mL of aqueous humor can usually be obtained. This small amount of fluid must be handled carefully. The aqueous humor usually should be used for cell studies and antibody measurement. However, if an infection is suspected, the aqueous humor can be cultured instead. Use of aqueous humor for cultures will reduce the volume available for cell studies and antibody measurement. If a larger amount of aqueous humor is required to complete the necessary studies, reaspiration of the anterior chamber typically can be performed safely within several minutes of the initial tap, once the anterior chamber has been reformed by production of more aqueous humor. Importantly, if an infectious organism is suspected, the vitreous provides both a higher yield of positive cultures and more material for culture, allowing more types of cultures to be performed.
Vitrectomy
Indications
Diagnostic vitrectomy should be considered when non-invasive methods have failed to establish a diagnosis in severe, sight-threatening uveitis. The goal of diagnostic vitrectomy is to attempt to determine the cause of inflammation, thus modifying and directing medical treatments.
Vitreous specimens may be obtained by either vitrectomy or direct vitreous aspiration. A diagnostic vitrectomy is preferable to a vitreous aspiration. With a three-port vitrectomy, a larger volume of vitreous sample can be obtained under direct visualization. Additionally, there is more control over the amount of vitreous traction produced during the procedure, and the intraocular pressure (IOP) can be controlled during the procedure.
Procedure
A diagnostic vitrectomy is performed using a standard three-port vitrectomy procedure. A longer infusion tip (4 to 6 mm) often is required in an eye with uveitis to accommodate scleral thickening, choroidal edema, or retinal separation that is frequently encountered (6). Direct visualization to confirm proper location of the infusion cannula within the vitreous cavity is essential before turning on the infusion in these patients.
The initial specimen in a diagnostic vitrectomy should be obtained undiluted, before the infusion port is turned on. A small amount of vitreous, 0.5 to 1 mL, should be obtained by using the vitrectomy instrument on low suction with the infusion line turned off. The sample is aspirated directly into a syringe through a three-way stopcock attached to the suction tubing. Next, the infusion line is opened and 10 mL of vitreous washings is aspirated into a separate syringe through the three-way stopcock. A therapeutic vitrectomy may then be performed in standard fashion, if necessary.
Both the undiluted vitreous aspirate and the vitreous washings should be immediately sent for microbiologic and cytologic analysis. Millipore filtration should be performed on vitreous washings to concentrate any microorganisms and cellular elements (2) (a sterile surgical clamp can be used before cutting off the filter that is connected to the tubing to prevent the loss of fluid content and to maintain the sterility). The filter can be cut up and sent for culture or cytology. The washings can be processed for immunohistochemical staining, and cellular specimens can be sorted for monoclonality and cell subtyping. Polymerase chain reaction and cDNA probes may be used to detect DNA from many infectious agents, such as the herpetic viruses and Toxoplasma gondii. If flow cytometry is indicated, Roswell Park Memorial Institute (RPMI) solution should be obtained from the flow cytometry lab on the day of surgery, and the concentrated sample of vitreous cells should be immediately stored in the RPMI solution and sent to the flow lab.
Retinal or Chorioretinal Biopsy
Indications
Occasionally, neither aqueous nor vitreous specimens will provide a useful answer. In certain infectious conditions, the inflammatory process is localized primarily to the retina or choroid. The vitreous may contain few or none of the responsible microorganisms; thus, a diagnostic vitrectomy would provide little information. A retinal biopsy may be indicated when there is a macula-threatening lesion unresponsive to therapy or suspicion of malignancy, and this may be undertaken at the time of retinal detachment repair. Chorioretinal biopsy may be considered in patients with severe, sight-threatening, medically unresponsive inflammation and is an alternative to diagnostic enucleation.
Procedure
The retinal biopsy site should be carefully selected to maximize diagnostic yield and to minimize intraoperative and postoperative complications. If possible, a location in the superior retina will allow for postoperative gas tamponade of the retinal biopsy site. A location posterior to the equator allows easier surgical access. The biopsy site should be at the border of normal retinal and active retinal disease; a biopsy of quiescent retinal disease or atrophic retina will have poor yield for diagnostic information.
A vitrectomy is performed, and the site for retinal biopsy is identified. If the retina was previously detached with a large tear, intraocular scissors can be used to obtain a sample of the tissue. If the retina is not detached, the endolaser is used to surround the identified site with a triple row of laser photocoagulation. A retinotomy is made, and saline is injected under the retina to create a bleb. Intraocular scissors are used to complete the retinectomy. Forceps are used to grasp the specimen and remove it from the eye (6). Care should be taken to not lose the retinal biopsy sample as the forceps leave the eye at the sclerotomy site. The retina is then reattached with pneumatic air–fluid exchange. The retina is inspected, and any retinal breaks are treated with endolaser. The sclerotomies are closed, and gas is exchanged with air.
The chorioretinal biopsy site should be carefully selected with location criteria similar to those used for a retinal biopsy site. However, a location anterior to the equator allows surgical access to the site from the eye wall. A standard three-port pars plana vitrectomy is performed, and the biopsy site is carefully identified with indirect ophthalmoscopy. The area is localized on the surface of the eye with scleral depression and marked with a pen. A triple row of photocoagulation is placed surrounding the biopsy site with the laser indirect ophthalmoscope to reduce bleeding and the risk of retinal detachment (6). The eye is filled with air. A scleral flap, 6 mm × 6 mm, with hinge at posterior aspect, is made as thick as possible. The inner bed is surrounded by diathermy. An inner rectangle of remaining sclera, choroid, and retina, 4 mm × 3 mm, is incised with a needle knife and then is removed with retinal scissors. The specimen is carefully grasped at the corner and removed. The scleral flap is sutured closed. The eye is then filled with gas. Alternatively, the suspicious chorioretinal lesion can be obtained intraocularly without making a scleral flap. The lesion should be outlined with endodiathermy and intense endolaser including the involvement of some normal surrounding tissue. The IOP should be increased to 60 mm Hg temporarily to prevent choroidal bleeding during the biopsy. Bimanual technique should be used with a chandelier to improve visualization. The combined retinal and choroidal biopsy specimen should be cut within the margins of the laser burns and endocautery with vertical-cutting intraocular scissors. While the lesion is being cut for several minutes afterward, the infusion bottle should remain at 60 mm Hg to prevent intraocular hemorrhage. The tissue can be removed from the enlarged sclerotomy site. Care should be taken not to crush the tissue (7).
The retinal or chorioretinal biopsy specimen should be carefully subdivided into three sections. The first section is sent for light and electron microscopy, the second section is sent for viral or fungal culture or polymerase chain reaction analysis, and the third section is sent for immunohistochemical studies to determine the type of predominant immune response (2).
Despite optimal medical therapy to control ocular inflammation, therapeutic surgery may be needed to treat the complications and sequelae of chronic inflammation. The following are therapeutic surgical procedures that may be indicated in the treatment of the complications of uveitis. It must be remembered that operating on an eye that has been repeatedly or chronically inflamed is very different from operating on an eye that has not been inflamed. The alterations in ocular tissue after recurrent inflammation make ophthalmic surgery challenging to even the most accomplished ophthalmic surgeon. The pediatric uveitic eye may respond with explosive postoperative inflammation following the most gentle operation. Maximum control of inflammation preoperatively, intraoperatively, and postoperatively allows the greatest chance of a successful surgery.
Band Keratopathy
Indications
Calcium hydroxyapatite may accumulate in the epithelial basement membrane, basal epithelium, and Bowman membrane in children with chronic uveitis such as JRA, sarcoidosis, or chronic intermediate uveitis (8). These deposits can become densely white with a rough surface that elevates the epithelium and results in pain, foreign body sensation, recurrent corneal erosions, and decreased vision. Indications for surgery are for vision rehabilitation, ocular surface improvement with decreased corneal erosions, or enhancement of the ophthalmologist’s view to perform adequate ocular examinations.
Band keratopathy may be removed by disodium ethyl-enediaminetetraacetic acid (EDTA) chelation and superficial keratectomy. An alternative method of removal of band keratopathy is with excimer laser phototherapeutic keratectomy (PTK) with the plan to operate within a few days; however, this often leaves a highly irregular base due to the nonuniformity of the calcium density in the band across the cornea (9). PTK effectively treats the ocular surface symptoms, but the improvement in visual acuity is variable. Stewart and Morrell (10) reported that of the patients with band keratopathy who underwent PTK for visual rehabilitation, 55% had an improvement or no change in visual acuity, whereas 45% had a decrease in visual acuity. Of the patients who underwent PTK for ocular surface improvement, 83% had an improvement in symptoms. Chelation with EDTA remains the mainstay of surgical therapy for band keratopathy and should be attempted prior to PTK. In chronically inflamed eyes, such as in children with JRA-associated uveitis, multiple recurrences of band keratopathy usually occur, which may require multiple future treatments.
Procedure
Although chelation can be performed with local anesthesia, general anesthesia usually is necessary for these pediatric patients. Foster has described his technique for EDTA chelation and superficial keratectomy (1). The epithelium overlying the calcium deposition is removed with a no. 15 Bard-Parker blade by wiping off the epithelium, ensuring that no cuts are made in the Bowman membrane. After the epithelium is removed, a well, which can be made from a cut back end of a 3-mL plastic syringe, is positioned over the affected area and cut side up. Solution of 0.35% EDTA is placed in the watertight well and held in position for 5 minutes, to chelate calcium in the affected area while protecting the limbal stem cells. The well is removed, and the cornea is irrigated with balanced salt solution. The no. 15 blade is used to scrape the loosened fakes of calcium. The procedure is repeated as many times as necessary to remove the calcium from the central cornea. Care must be taken to avoid scarring of the Bowman membrane in the visual axis. Cycloplegic and antibiotic medications are instilled, a continuous-wear bandage soft contact lens is placed, and the eye is patched. Topical antibiotic and steroid are used postoperatively. Bandage contact lens, cycloplegia, and oral analgesics help with pain control. The epithelium generally has covered the corneal surface within 1 week following surgery, and the bandage soft contact lens can be removed.
Glaucoma
Mechanisms of Glaucoma in the Uveitis Setting
Glaucoma may occur in the uveitic patient as a consequence of severe anterior segment inflammation. The mechanism of IOP elevation in the uveitic eye is complex, and a combination of mechanisms may coexist in the eye with uveitis. The five major causes of secondary glaucoma in patients with uveitis are secondary angle closure from posterior synechiae causing pupillary block and iris bombe, secondary angle closure by peripheral anterior synechiae, blockage of the trabecular meshwork by inflammatory debris, active trabeculitis, or steroid-induced IOP rise. Additionally, active inflammation may suppress ciliary body function with a decrease in IOP. Thus, IOP in the actively inflamed eye may be higher or lower than in the uninflamed eye. Topical steroid administration may relieve trabeculitis and reduce IOP. Topical corticosteroids may increase IOP from either reactivated ciliary body function or a steroid-induced IOP rise. Increased IOP with the addition of corticosteroid may complicate the management of the pediatric uveitic patient who needs the corticosteroid for treatment of inflammation and for prevention of ocular damage from chronic inflammation.
Angle-Closure Glaucoma
Indications
Patients with uveitis may develop posterior synechiae sufficient to produce relative pupillary block, iris bombé, and secondary angle closure. Ordinarily in a patient with nonuveitic pupillary block glaucoma, laser peripheral iridotomy is the therapeutic procedure of choice. However, in the inflamed eye of a pediatric uveitic patient, the laser peripheral iridotomy commonly closes. Moreover, the young age of the pediatric patient makes laser procedures difficult. A large surgical iridectomy under general anesthesia is the procedure of choice in the pediatric uveitic patient with pupillary block and secondary angle closure.
Procedure
Surgical iridectomy consists of five steps: (i) incision, (ii) exteriorization of the iris, (iii) excision of the iris, (iv) repositioning of the iris, and (v) closure of the incision. The incision may be made in the sclera under a conjunctival flap or through clear cornea. Although it is more difficult to prolapse the iris tissue through a clear corneal incision, the conjunctiva will be spared for future glaucoma surgery.
A partial thickness incision is made perpendicularly into clear cornea. Preplaced sutures are then placed on either side of the corneal incision to facilitate spreading of the corneal wound. The corneal incision is then continued perpendicularly until the anterior chamber is entered. Gentle pressure on the posterior lip of the wound usually will prolapse the iris into the wound. The prolapsed “knuckle” of iris is then excised. If the iris does not prolapse, then the anterior chamber must be entered with fine nontoothed forceps to grasp the iris. After iridectomy, the iris usually will spontaneously return into the anterior chamber. If the iris remains prolapsed, radial massage from wound to central cornea with a smooth instrument will result in spontaneous repositioning of iris back into the anterior chamber. The wound is closed with 10-0 nylon suture. Corticosteroid is injected subconjunctivally.
Uveitic Glaucoma
Raised IOP in patients with uveitis may lead to visual loss. Patients with chronic uveitis, who develop intractable glaucoma, are notoriously difficult to treat (11). Medical therapy often proves inadequate in controlling IOP, necessitating surgical intervention. Conventional filtering procedures, such as trabeculectomy, are known to fail more frequently in inflamed eyes than in noninflamed eyes. Although some studies report fairly successful 1-and 2-year results of trabeculectomy, with or without antimetabolites, the long-term success rate of trabeculectomy in patients with uveitic glaucoma is quite poor (12–15). Glaucoma drainage implants have been reported by some studies to have fairly successful 1-and 2-year results, with continued, moderate long-term success at 5 and 10 years (13,16–19).
After trabeculectomy, the extensive inflammatory response of the pediatric eye and the recurrent or chronic nature of inflammation result in fibrous tissue growth and subsequent closure of the filtering bleb over time. Although adjunctive antimetabolites may keep the filtering bleb open in the initial few weeks or months after surgery, recurrent inflammation may later close the filtering bleb. Thus, the long-term success rate of filtering surgery has a decreasing chance of success in these pediatric uveitic patients over time. One- and two-year success rates after trabeculectomy without antimetabolite therapy range from 67% to 92% (12–15). Hoskins et al. (12) reported a 67% success rate at 1 year, Hill et al. (13) reported 81% and 73% success rates at 1 and 2 years, and Stavrou et al. (14) reported 92% and 83% success rates at 1 and 2 years. However, at 5 years, the success rates decrease dramatically. Towler et al. (15) reported that the success rate fell from an 80% at 2 years to 30% at 5 years. With the addition of antimetabolites to trabeculectomy, Towler et al. (15) reported an improvement to 50% of patients still controlled at 5 years.
Some studies report reasonable success rates using glaucoma drainage devices for control of uveitic glaucoma. More importantly, the long-term success rates remain fairly good. Choroidal effusions, hypotony, and cystoid macular edema comprise the most common postoperative complications. The 1-and 2-year success rates after glaucoma drainage devices range from 92% to 94% (13,16–19). A 91.7% success rate at both 1 and 2 years with IOPs of 5 to 21 mm Hg was reported in 24 eyes treated with Baerveldt glaucoma drainage implant (16). A 94% success rate at 1 year with IOP ≤21 mm Hg was reported in 21 eyes treated with Ahmed valve implantation (17), whereas a 79% success rate at both 1 and 2 years with IOP of 6 to 21 mm Hg with Molteno device implantation (13). A 95% success at 27 months and a 90% success at 52 months with IOP ≤22 mm Hg with Molteno device implantation were reported in 27 eyes with secondary glaucoma caused by JRA (18). In a prospective case series of 40 eyes, the probability of the Molteno implant to control IOP ≤21 mm Hg was calculated to be 87% at 5 years and 77% at 10 years after surgery (19).
In the child with uveitis, surgery is best undertaken after the inflammation is maximally controlled with corticosteroid or immunosuppressant medications for as long as possible preoperatively in patients undergoing nonurgent glaucoma surgery. A glaucoma drainage device may be implanted in standard fashion between Tenon fascia and sclera and secured in place. The silicone tube is tied off if the Baerveldt implant is used. The tube is placed through either the limbus or the pars plana in vitrectomized eyes. The tube and its insertion site are covered with a patch of preserved donor sclera. Topical corticosteroids are used postoperatively. Maximum control of inflammation preoperatively, intraoperatively, and postoperatively allows the greatest chance of a successful surgery.
In the pediatric aphakic uveitic patient, postoperative amblyopia therapy is vital with proper spectacles or aphakic contact lens. If a glaucoma drainage implant is placed in a vitrectomized, aphakic, pediatric patient, a pars plana tube placement will better allow contact lens fitting following surgery (1).
Cataract
Cataract is one of the most common complications of uveitis, with a prevalence of up to 50% and can be attributed to chronic inflammation and corticosteroid use (20,21). Cataract surgery in pediatric uveitic eyes is daunting to even the most accomplished cataract surgeon because of the unknown risks faced intraoperatively and the uncertainty of the postoperative course (3,4). The uveitic cataract frequently is technically challenging with posterior synechiae, iris vasculature delicacy, pupillary membranes, miotic pupil, and corneal opacification (5). There may be permanent damage to ocular structures before the cataract surgery such as maculopathy, chronic macular edema, epiretinal membrane, glaucomatous optic neuropathy, or cyclitic membrane with associated hypotony and progressive phthisis, which may limit a good visual outcome after surgery. The combination of the pediatric heightened immune response and a uveitic eye often results in a fierce postoperative inflammatory response following the most careful operation.
Indications
Indications for cataract surgery in the child with uveitic cataract include visual rehabilitation, prevention or treatment of amblyopia, and enhancement of the ophthalmologist’s view of the posterior segment for ongoing assessment of the optic nerve and retina.
Cataract extraction with intraocular lens (IOL) implantation has become increasingly successful over the past 20 years as a result of improved microsurgical techniques and viscoelastics, as well as more rigorous control of recurrent inflammation and chronic low-grade inflammation (1,2). Currently, cataract extraction with endocapsular posterior chamber IOL is an accepted practice in the management of many adults with uveitic cataract, provided the inflammation has been quiescent for a sustained period before surgery (22). However, the decision whether to implant an IOL in a pediatric patient with uveitis remains controversial.
Procedure
The surgical technique for cataract extraction in a child with uveitis should include removal of the cataract, including the posterior capsule, all retrolenticular and cyclitic membranes, and most of the vitreous. Historically, pars plana lensectomy with pars plana vitrectomy was the procedure of choice (23). For the pars plana approach, the lens and posterior and anterior capsules are cut and aspirated with an ocutome/vitrectomy probe. This is followed by a near-total vitrectomy. Removal of the lens capsule and anterior hyaloid must be performed in an attempt to eliminate the “scaffold” along which secondary membranes may subsequently form (20). This reduces the likelihood of subsequent posterior synechiae and cyclitic membrane formation and decreases the need for postoperative neodymium: yttrium–aluminum–garnet (Nd:YAG) laser capsulotomy, which may be difficult in small children and which may often incite further inflammation (23–26). A surgical peripheral iridectomy should be made if recurrent or chronic inflammation is anticipated.
Cataract extraction may be accomplished by a combined limbal approach with phacoemulsification and pars plana vitrectomy. During the limbal approach, synechiolysis, pupillary stretching, and iris hooks are used as needed for adequate exposure. Then a capsulorrhexis, hydrodissection, and phacoemulsification are performed in standard fashion, and the incision is closed. This is followed by a pars plana approach for complete posterior capsule excision, followed by a near-total vitrectomy.
The decision whether to implant an IOL in a pediatric patient with uveitis remains controversial. The decision must be carefully considered and must be tailored to both the patient and the risk of recurrent inflammation. If the disease course predicts recurrent inflammation or chronic inflammation, the child is at extremely high risk of developing thick perilenticular membranes, severe postoperative inflammation, and iris capture. The IOL itself may provide a stimulus for intraocular inflammation and structural support for inflammatory membranes, which can result in ciliary body dysfunction, ocular hypotony, and chronic macular edema. Treatment of these membranes with Nd:YAG capsulotomy can incite further inflammation and reformation of membranes. Even with surgical posterior capsulectomy, retrolental membranectomy, and total vitrectomy, significant perilenticular membranes may persist or recur. In addition, chronic inflammation refractory to therapy or cyclitic membranes can result in hypotony, and ultimately, IOL removal is required (22). Patients at highest risk of required IOL explantations are young patients with JRA, as periodic fare-ups of uveitis were still occurring, and patients with chronic low-grade peripheral uveitis (22). IOL implantation is contraindicated in children with JRA-associated uveitic cataract (1,2,20,27).
The choice of IOL may affect postoperative inflammation and formation of perilenticular membranes. Acrylic lenses may be the least inflammogenic (28,29). In a report (28) of a randomized, double-masked trial of 36 adult uveitic eyes that had implantation with one of four IOLs (silicone, polymethylmethacrylate (PMMA), heparin-coated PMMA, or acrylic lenses), acrylic lenses appeared to provide the best overall result when evaluated for postoperative inflammation, posterior capsular opacification (PCO) rates, cystoid macular edema, and final visual acuity. Of 140 adult uveitic eyes that had implantation with silicone, PMMA, heparin-coated PMMA, or acrylic lens, the acrylic lens resulted in a lower PCO rate (29). The choice of IOL in the pediatric uveitic eye remains to be studied. The use of heparin in the infusion solution for pediatric uveitic cataract surgery is controversial (30,31).
Management of Inflammation
The essential element for successful cataract surgery is vigilant control of inflammation preoperatively, perioperatively, and postoperatively. Cataract surgery has an increased chance for a successful outcome if it is performed after the inflammation has been quiescent for as long as possible, ideally more than 3 months. Surgery in the presence of active inflammation carries a much higher potential for complications. The optimal time to operate is after the active inflammatory phase of the uveitis has burned out (32). This is particularly true in case of intermediate uveitis in which the inflammation may remit without recurring. If this is not practical, the next best time to operate is after the uveitis has been inactive for several months with corticosteroid treatment. This is true in cases of acute intermittent inflammation. In some patients with chronic inflammation, it is impossible to completely quiet the eye. Although attempts should be made to maximally quiet the eye, surgery should not be delayed to the point of leading to irreversible ocular damage. If the level of inflammation cannot be assessed, the eye should be prophylactically treated for a few days as though active inflammation were present (2).
Systemic immunosuppressive therapy in the form of low-dose methotrexate may be needed for adequate preoperative control of inflammation in children with JRA-associated uveitis. In 2003, a favorable outcome was reported in five children (six eyes) younger than 13 years with JRA-associated uveitis who underwent standard phacoemulsification cataract extraction without a posterior capsulectomy and with posterior chamber IOL implantation (33). Postoperative visual acuity was 20/40 or better in all six eyes. Median follow-up was 44 months. Preoperatively, four children (five eyes) were on low-dose methotrexate immunosuppressive therapy for a median length of 1.25 years before surgery. Preoperatively, two children (three eyes) were on additional immunosuppressants or systemic corticosteroids. All eyes received frequent topical corticosteroid therapy for a median of 2 weeks preoperatively and 8.5 weeks postoperatively. Five eyes required Nd:YAG capsulotomy. One eye needed a subsequent surgical posterior capsulectomy and pars plana vitrectomy. The authors concluded that children with JRA-associated uveitis might have favorable surgical outcomes after cataract surgery with posterior chamber IOL implantation provided they had adequate long-term preoperative and postoperative control of intraocular inflammation with systemic immunosuppressive therapy and intensive perioperative topical corticosteroid therapy.
Perioperative control of inflammation is vital, as the pediatric uveitic eye often has an intense postoperative inflammatory reaction. The goal of perioperative medications is to control and reduce the anticipated severe postoperative inflammation. Although specific medications and dosing schedules vary, the concepts are similar. In general, patients should be given oral and topical corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs) for 1 to 3 days preoperatively, even if there is no evidence of active inflammatory disease. Intraoperatively, patients should receive a periocular steroid injection and may receive an intravenous bolus of steroid. Periocular injections may be delivered to the retroseptal space or the subtenon space. In small children, 20 mg of triamcinolone acetonide is effective (34). A study published by Cleary et al. (35) has shown that 4 mg (4 mg/0.1 mL) of intracameral preservative-free triamcinolone (Triesence) used at the conclusion of the cataract surgery can effectively control postoperative inflammation in a safe manner in pediatric population. Postoperatively, patients should receive aggressive topical steroids and NSAIDs, along with oral steroids and NSAIDs. Perioperative steroid remains superior to perioperative cyclosporine in preventing severe postoperative inflammation (2).
Postoperatively, the eye may appear quiet at first but then may respond with a violent inflammatory reaction with significant dense fibrin and an outpouring of protein within the eye. This inflammatory response peaks about 48 hours after surgery and lasts for 5 to 6 days after the surgery, even in the presence of high doses of systemic corticosteroids. Pediatric uveitis patients should be examined every day for the first 5 to 7 days postoperatively (2). Occasionally, a severe dense fibrin that is refractory to steroids and NSAIDs may occur in the anterior chamber within 6 days after surgery. Recombinant tissue plasminogen activator (rt-PA) can be used to clear severe dense fibrin in the anterior chamber. A report on 11 pediatric eyes, 3 with uveitis, who developed dense fibrin clots after cataract surgery that was refractory to intensive prednisolone acetate and cycloplegic agents showed a benefit of rt-PA (36). Injection of rt-PA, 100 µL of 10 µg/100 µL, into the anterior chamber thought a limbal paracentesis resulted in complete resolution of fibrin formation in all eyes except for two eyes in a JRA patient, usually within 24 hours.
Visual Rehabilitation
It is imperative to remember that a successful operation is only part of the visual rehabilitation in a child. Postoperative amblyopia therapy in conjunction with a pediatric ophthalmologist is equally important with proper postoperative spectacles or contact lenses, orthoptic evaluation, and occlusion therapy. Parents must be constantly educated about amblyopia therapy. Despite excellent anatomic outcomes, visual rehabilitation for aphakic eyes may be suboptimal because many patients of this age are unable or refuse to wear aphakic contact lens or aphakic spectacles (37). Among children, contact lens intolerance is reported to range from 17% to 38% (27,38). The frequent concomitant occurrence of band keratopathy makes contact lens fitting difficult. Multiple lost contact lenses carry a substantial expense. Children often are intolerant of aphakic spectacles because of the weight and aniseikonia. The age of the child at the time of surgery, the presence or absence of amblyopia, and the presence of irreversible retinal or optic nerve pathology are the primary factors influencing the outcome of cataract surgery in the pediatric uveitic patient.
Vitreoretinal Surgery
Pars plana vitrectomy may be performed for the many vitreoretinal complications secondary to chronic uveitis. Vitreous removal may have a curative or moderating effect on the clinical course in patients with intermediate uveitis, JRA-associated uveitis, and sarcoidosis. Indications for pars plana vitrectomy include persistent vitreous opacification, medically unresponsive vitreitis, traction retinal detachment, impending retinal detachment, epiretinal membrane creating significant distortion or heterotropia, cyclitic membrane, prevention or treatment of amblyopia, and enhancement of the ophthalmologist’s view of the posterior segment for ongoing assessment of the optic nerve and retina. These patients frequently have cataract, posterior synechiae, and vitreous opacification that must be addressed either prior to or at the time of vitreoretinal surgery. Final visual prognosis often is limited by the presence of macular or optic nerve pathology.
Indications
There are four objectives in pars plana vitrectomy in patients with chronic uveitis. The first is to remove opacities in the visual axis. The second is to remove vitreomacular membranes producing retinal traction or epiretinal membranes causing macular pucker. The third is to remove cyclitic membranes or thickened anterior cortical hyaloid causing hypotony. The fourth is to alter the course of vitreous inflammation refractory to medical therapy or persistent cystoid macular edema.
Remove Opacities in the Visual Axis: In cases of vitreous inflammation refractory to medical therapy, a pars plana vitrectomy is performed to clear the visual axis by removal of media opacities and vitreous debris.
Alter the Course of Vitreous Inflammation Refractory to Medical Therapy: Vitrectomy may alter the course of inflammation and result in stabilization of the disease by removing immunocompetent cells and inflammatory mediators from the vitreous cavity (24,25,39). Vitrectomy may potentially reduce cystoid macular edema either by eliminating the contact between an inflamed vitreous body and the macula or by allowing better penetration or distribution of corticosteroids (23,24,40). However, others have noted that although vitrectomy removes vitreous debris and appears to allow for easier intraocular penetration of corticosteroid, no change in the inflammation process was observed (2).
Remove Vitreomacular Membranes: Membranectomy may be performed after pars plana vitrectomy to remove inflammatory membranes from the retina and ciliary body. Anteroposterior vitreomacular traction from an inflamed vitreous body may result in chronic cystoid macular edema or may create a shallow traction retinal detachment. Tangential traction caused by epiretinal membranes causes decreased vision and secondary cystoid macular edema. These membranes can be removed successfully at the time of vitrectomy by delamination or en bloc techniques. Traction also may lead to retinal breaks in atrophic retina, creating a combined traction–rhegmatogenous detachment, which may be repaired during pars plana vitrectomy.
Remove Cyclitic Membranes or Thickened Anterior Cortical Hyaloid: A cyclitic membrane may occur and may result in hypotony. Chronic traction of the ciliary body from a cyclitic membrane or a thickened anterior cortical hyaloid will result in ciliary body detachment and reduced aqueous humor formation. Pars plana vitrectomy and cyclitic membrane removal can be performed to reattach the ciliary body. A skilled assistant is required to assist in scleral depression in the region of the ciliary body so that the surgeon can dissect and remove the inflammatory membrane or surgically segment it to reduce traction. Alternatively, endoscopic vitrectomy can be performed to remove the cyclitic membrane (40).
Procedure
Vitreoretinal surgery is performed using a standard three-port vitrectomy procedure. A longer infusion tip (4 to 6 mm) is often required in uveitis patients to accommodate scleral thickening, choroidal edema, or retinal separation that is frequently encountered in an eye with uveitis (1). Direct visualization to confirm proper location of the infusion cannula within the vitreous cavity is important before turning on the infusion in these patients.
The infusion is turned on, and the endoillumination probe and vitrectomy cutter are introduced. A complete vitrectomy is performed. Preretinal membranes are dissected or stripped from the retinal surface using a combination of scissors, membrane picks, and forceps. If there is vitreous base exudation or neovascularization, it may be treated with laser scatter photocoagulation or cryopexy. Indirect ophthalmoscopy is used at the completion of the vitrectomy to search for any other retinal pathologies, such as retinal tears. If present, they are treated with retinal laser or cryopexy. Long-acting gas or silicone oil tamponade may be needed. Unless contraindicated, corticosteroids are injected in the vitreous space (4 mg Triesence) and periocularly (40 mg triamcinolone). The corticosteroids greatly assist in controlling excessive postoperative inflammation and fibrin formation. Regional and intraocular corticosteroids are contraindicated in a patient with a possible infectious etiology.
Management of Inflammation
Surgery has an increased chance for a successful outcome if it is performed after the inflammation has been quiescent for as long as possible, ideally more than 3 months. Occasionally, this cannot be obtained, and surgery must be performed while the eye is still inflamed, such as in surgery for medically unresponsive uveitis. Surgery in the presence of active inflammation carries a much higher potential for surgical complications.
Perioperative control of inflammation is vital, as the pediatric uveitic eye often has an intense postoperative inflammatory reaction. Postoperative fibrin and inflammation may promote cyclitic membrane formation and/or proliferative vitreoretinopathy. Final visual acuity will be influenced by the presence of macular scarring, cystoid macular edema, macular ischemia, or retinal necrosis. Patients have better visual prognoses if they presented with a macula-on retinal detachment.
Laser
In the nonuveitic eye, lasers often are used to perform peripheral iridotomy and posterior capsulotomy, to cut pupillary membranes, and to treat retinal or subretinal neovascularization. Any laser procedure may incite an extensive inflammatory response in a uveitic eye. Periprocedural control of inflammation is important, with frequent topical corticosteroid dosing and consideration of periocular or systemic corticosteroids.
Surgical Iridectomy Preferable to Peripheral Iridectomy: Patients with uveitis may develop posterior synechiae sufficient to produce relative pupillary block subsequent iris bombe configuration, narrow angles, and possibly angle-closure glaucoma. Ordinarily, laser peripheral iridotomy is the therapeutic procedure of choice. In the pediatric uveitic patient, the positioning of a child at the Nd:YAG laser is difficult. Additionally, chronic or recurrent inflammation often will result in subsequent closure of the laser peripheral iridotomy. A surgical iridectomy performed with the patient under general anesthesia is preferable to laser peripheral iridotomy in the pediatric uveitic patient.
Posterior Capsulotomy versus Surgical Posterior Capsulotomy
Cataract formation is a frequent complication of uveitis. After phacoemulsification cataract extraction with posterior chamber IOL implantation, thick perilenticular membranes often form in the pediatric population, particularly in patients with chronic or recurrent uveitis. These perilenticular membranes may result in ciliary body dysfunction, ocular hypotony, and chronic macular edema. The thick inflammatory membranes often require multiple sessions of Nd:YAG capsulotomy, which often may incite further inflammation, and they may subsequently reaccumulate. Eventually, surgical posterior capsulectomy, retrolental membranectomy, and total vitrectomy may be necessary. If IOL implantation is attempted in a pediatric uveitic patient, especially a patient with JRA, a posterior capsulectomy with removal of the anterior hyaloid face and a thorough near-total vitrectomy should be considered in attempts to eliminate the “scaffold” along which secondary membranes may subsequently form (20). This reduces the likelihood of subsequent posterior synechiae and cyclitic membrane formation and decreases the need for postoperative Nd:YAG laser capsulotomy, which may be difficult in small children (23–26,41).
Panretinal or Segmental Photocoagulation for Retinal Neovascularization (Sarcoidosis)
Patients with sarcoidosis may develop large areas of retinal capillary nonperfusion and secondary retinal or disc neovascularization. Both retinal and disc neovascularization may regress in patients with sarcoidosis in up to 50% of patients treated by systemic medical therapy alone (42,43). When persistent or progressive peripheral retinal neovascularization causes recurrent vitreous hemorrhage, laser photocoagulation to avascular areas of retina may be required to eliminate the neovascularization. Local grid treatment or cryopexy is applied to the areas of ischemia adjacent to retinal neovascularization. Fluorescein angiography can define the areas of ischemia and help direct photocoagulation. Laser photocoagulation usually is followed by a significant increase in cystoid macular edema (42). Steroid therapy and possibly with additional antivascular endothelial growth factor therapy should be used in combination with laser treatment to blunt the inflammatory response. When disc neovascularization causes recurrent vitreous hemorrhage, panretinal photocoagulation may be required to eliminate the disc vessels.
Peripheral Neovascularization (Intermediate Uveitis)
Patients with intermediate uveitis may develop peripheral retinal neovascularization. These patients have thick ropy neovascularization in the far periphery extending over the ora serrata, which often is obscured from visualization by pars plan exudation and vitreitis. In patients with unremitting chronic pars planitis that is recalcitrant to steroid or NSAID therapy, cryotherapy and scatter laser photocoagulation of the peripheral retina have been reported to be effective in causing regression of peripheral neovascularization and reduction of inflammatory activity. This treatment can reduce the frequency of vitreous hemorrhage and may reduce the severity of the intermediate uveitis and cystoid macular edema. Cryotherapy is thought to reduce inflammation by eliminating the inflammation stimulus in the peripheral retinal tissue (44,45). Reduction in neovascularization may be caused by direct vessel ablation or by destruction of ischemic retinal tissue (45,46).
In children, cryotherapy is performed with general anesthesia. Retrobulbar anesthesia is given for intraoperative and postoperative pain control. Cryotherapy is applied directly to the areas of exudation at the pars plana using a double freeze–thaw technique (26,44). The ice ball should be seen to cover the exudative area and neovascularization. Uninvolved pars plana and retina are treated one CryoTip width beyond the involved area. In areas where the visualization of the ice ball is precluded, freezing should be continued for a time interval similar to that required in adjacent areas with adequate visualization. Periocular steroids are administered following the procedure. The procedure may be repeated in 3 to 4 months if there is residual disease. Cryotherapy was first advocated in 1973 (44) and was later reported to eliminate inflammation in 78% of 27 eyes (47). Visual acuity improved or remained unchanged in 89% of eyes and eliminated the need for corticosteroids therapy in 90% of eyes.
Panretinal scatter photocoagulation has been shown to be effective in the treatment of peripheral neovascularization associated with intermediate uveitis. Regression of neovascularization, improvement of cystoid macular edema, and stabilization of inflammation were reported in 10 eyes with scatter diode or argon photocoagulation treatment, either alone or in combination with pars plana vitrectomy (48).
Three rows of photocoagulation are delivered to the inferior retinal periphery, just posterior to the area of exudation or neovascularization. Treatment may be carried out with either argon endophotocoagulation or an indirect ophthalmoscopic delivery system using argon or diode photocoagulation. Laser photocoagulation appears to be a safe and effective alternative to cryotherapy and is a useful adjunct during a therapeutic pars plana vitrectomy.
SLOW-RELEASE STEROID TREATMENT FOR UVEITIS
Two sustained-release, steroid-based drug delivery devices currently are on the market, as well as another potential product that has not yet been approved for marketing by the United States Food and Drug Administration (U.S. FDA). One device, the Retisert implant, is a reservoir-based, surgically implanted device containing 0.59 mg of fluocinolone acetonide (FA); it is designed to release the drug over a 3-year period. The device initially was developed by Control Delivery Systems (Watertown, MA) and now is licensed by Bausch & Lomb (Rochester, NY) (Fig. 55.2). The device has been shown to be extremely effective for the treatment of uveitis, even in patients who have had poor control of their disease with aggressive systemic therapy (Figs. 55.3 and 55.4) (49). A pilot study by Patel et al. has shown that the Retisert can effectively control posterior inflammation in pediatric patients. A total of six eyes of four children were enrolled in this study. Retisert implants were able to control the inflammation of all six eyes. The safety profile was very similar to what has been described in adult patients. One of the six eyes of the pediatric patients developed visually significant cataract that was surgically removed. Two patients also developed high IOP, which was treated with glaucoma shunting procedures (50).

FIGURE 55.2 FA reservoir device (Retisert, Bausch & Lomb, Rochester, NY) alongside rulers.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


