FIGURE 50.1 Adult patient with bilateral iris (A,B) and optic nerve coloboma. The right eye has band keratopathy and chronic retinal detachment.
The tendency for late diagnosis at presentation is an important feature of pediatric retinal detachment, with predictable consequences (20). PRRD typically presents as macula-off (80%) (4,5,12). In contrast, macula-off RRD occurs less frequently in adults. In 342 eyes with RRD from patients with mean age of 52.8 years, the macula was detached in only 56.5% of the eyes (21). Proliferative vitreoretinopathy (PVR) is present at initial diagnostic examination in 20% to 60% of all eyes (Fig. 50.2) (8,10,12,22), in line with reports of RRD after previous ocular surgery in which PVR was observed at initial presentation in 39% and 41% of adult patients, respectively (19,23).


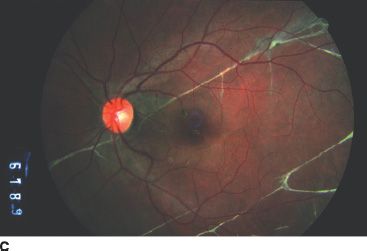
FIGURE 50.2 A: Total retinal detachment with associated PVR. B: Posterior pole image of the same eye shown in panel A following vitreoretinal surgery, completely attached under silicone oil. C: Strands of subretinal PVR, without retinal detachment.
A single retinal break or horseshoe retinal tear is commonly the cause of PRRD. Giant retinal tears (Fig. 50.3) are generally seen in association with syndromes such as Stickler syndrome type 1. Conversely, the vast majority of retinal dialyses occurs as a consequence of trauma. Retinal dialyses occur most commonly following trauma (nonsurgical and surgical).
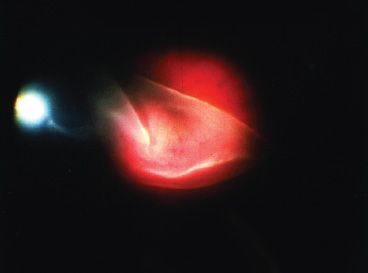
FIGURE 50.3 Retina folded over itself with bare retinal pigment epithelium in an eye with a giant retinal tear.
Many of the conditions associated with PRRD are covered in depth elsewhere (see Chapters 27, 51, 54, and 56). The vasoproliferative retinopathies, particularly retinopathy of prematurity (Chapters 44 and 49) persistent fetal vasculature syndrome (Chapter 53) and familial exudative vitreoretinopathy (Chapter 28), though generally associated with traction–exudative retinal detachment, will occasionally evolve to combined mechanism detachments with a rhegmatogenous component.
Postsurgical
Several published series of PRRD include eyes in which detachment occurred following ocular surgical procedures (3,8,9,10,12,13,24). A variety of limitations (population size, ascertainment bias, and more) preclude accurate determination of the incidence of iatrogenic PRRD. Good incidence data are lacking for iatrogenic adult RRD following ophthalmic surgeries as well, with published series generally discussing specific procedures such as extracapsular cataract extraction (0.02% to 3.6%) (25) or Molteno glaucoma implant surgery (3% to 5%) (23).
Eyes progressing to PRRD following ophthalmic surgical procedures (for cataract, strabismus, corneal transplantation, or glaucoma tube shunt) often fare considerably worse than previously unoperated eyes. In our published series (12), the postoperative subgroup included all eyes with RRD and known antecedent intraocular surgery. This group included eyes with juvenile glaucoma, congenital cataracts, Peter anomaly, juvenile retinoschisis, and the sequelae of these disorders and accounted for 34% (10/29) of eyes in this series. We qualified them by the procedure performed immediately prior to the development of RRD. None of the eyes developed a recognized retinal detachment intraoperatively. Of these 10 eyes, 6 were aphakic, 5 had undergone pars plana vitrectomy, 2 had Molteno tube placement, 1 had trabeculectomy, 1 had suprachoroidal drainage, and 1 had penetrating keratoplasty.
Nontraumatic Inferotemporal Retinal Dialysis (“Juvenile Dialysis”)
Retinal dialysis is defined as a break at the junction of the retina and the pars plana, typically along the course of the ora serrata. Dialyses, in general and following trauma, are more common in the inferotemporal quadrant. However, most dialyses detected in the superonasal quadrant are associated with a history of preceding trauma (26,27). Idiopathic retinal dialyses accounted for approximately 2% of retinal detachments in one series, typically occurring in the inferotemporal quadrant of young adult eyes.
Retinal detachment associated with retinal dialysis often is subclinical. Associated findings include demarcation lines, retinal cysts, peripheral microcystoid degeneration, and yellow-white vitreous opacities (28). PVR is seen rarely, perhaps due to the overlying vitreous base impeding access of cells to the central vitreous cavity.
Retinal detachments from idiopathic retinal dialyses have been a subject of debate, considered by some not to represent a distinct clinical entity (29). Reports of bilateral involvement have been cited to refute this contention (30,31). It is generally described in emmetropic males presenting with dialysis-related retinal detachments in the second decade of life, reportedly affecting multiple family members (32,33). Kinyoun and Knobloch noted peripheral cystoid degeneration in 36 eyes of 32 patients with nontraumatic inferotemporal retinal dialysis. Bilateral nontraumatic retinal dialysis is an indication for examination of family members.
Atopic Dermatitis
Atopic dermatitis, a chronic pruritic skin condition, is an allergic form of eczema primarily affecting infants, children, and young adults. Onset usually is in infancy, often with a positive family history of atopic disease. Prevalence is on the order of 10% in the United States and up to 20% in Japan. The incidence of atopic dermatitis is thought to be rising (34,35), with retinal detachments in such patients representing approximately 3% of RRDs seen in Japan. RRD typically occurs in early adulthood but may be seen in late adolescence (36).
Eyelid dermatitis, blepharitis, conjunctivitis, cataract, and keratoconus are recognized anterior segment associations. Retinal detachment has been reported in 6% to 10% of Japanese patients (37,38). The peripheral fundus is characterized by a “fluffy” appearance, with signs of vitreous base contraction (wrinkling of the pars plana epithelium and oral dialyses) (39). Retinal breaks often are multiple and located at the ora serrata or in the nonpigmented ciliary body epithelium (18). Retinal detachments are generally low lying and asymptomatic, although giant retinal tears occur as well (40). Intense pruritus prompts frequent eye rubbing and face slapping, thought to play a role in causing retinal or ciliary body breaks. Scleral buckle with thorough peripheral retinopexy is advocated for this reason. Maruyama et al. (41) suggest that moderate-to-dense anterior chamber angle pigmentation in patients with atopic dermatitis is a sign of breaks of the peripheral retina or ciliary body epithelium and should be an indication of meticulous peripheral retinal examination.
The office evaluation is the usual starting point in the evaluation of PRRD. Family history and review of systems are particularly important in PRRD, both in the interest of diagnosis as well as relating to discussion of prognosis and clinical course. Examination of the parents and siblings, including fundus imaging (color photos and wide-angle fluorescein angiography), may be indicated (familial exudative vitreoretinopathy, oculoarthropathies, etc.).
Precise determination of visual acuity is the goal, yet is difficult in the very young. Observation of a child’s visually guided behavior as the physician interacts with the parents is useful in this regard.
Thorough examination in infants, juveniles, and most adolescents is accomplished most effectively under anesthesia. The standard examination under anesthesia includes external evaluation (facial features, dermatologic abnormalities, etc.), intraocular pressure measurement, anterior segment examination, extended ophthalmoscopy, wide-field color digital fundus imaging, and fluorescein angiography. Optical coherence tomography, B-scan ultrasonography, and ultrasound biomicroscopy are performed as indicated. Meticulous examination of the companion eye is critical, as clinically important retinal pathology is commonly discovered (5,6,12,9,10). It is not uncommon for treatment of the better seeing companion eye to be the most effective intervention performed for a given child.
General Considerations
While management of PRRD varies with the clinical circumstances, some general principles bear mention.
There is a high likelihood that multiple procedures will be necessary for successful repair for two reasons: reported single-procedure anatomical success rates range from approximately 50% to 90% (22) and silicone oil commonly employed for intraocular tamponade almost always requires removal in a subsequent procedure. Furthermore, amblyopia therapy is an inescapable component of the care regimen following successful retinal detachment repair. Given this, repair of PRRD is more a journey than an event. This reality is discussed in detail with parents prior to surgery.
Though the core tenets of identifying, treating (retinopexy), and supporting retinal breaks apply as they do in adults, traction due to cicatricial fibrovascular proliferation or hyaloidal contraction is more likely to be a contributing factor. For this reason, while it is often preferable to repair PRRDs employing scleral buckle alone, the contribution of tractional pathology to the detachment may require a subsequent vitreous surgery or even a combined scleral buckle and vitrectomy initially.
Every effort is made to spare the lens in the interest of optimizing visual rehabilitation, but not at the expense of successful retinal reattachment. As an example, giant retinal tears are repaired with vitrectomy, endolaser, and silicone oil in most instances, and the lens often is sacrificed to facilitate meticulous vitreous removal. Aphakia is not as amblyogenic as recurrent retinal detachment. When necessary, the lens is sacrificed. In some cases, combined surgery with an experienced cataract surgeon can permit phacoemulsification and placement of an intraocular lens at the time of vitrectomy.
Plasmin enzyme (autologous, heterologous, or recombinant), though not yet widely available, can be useful in eyes requiring dissection of extensive proliferation (42) or diffuse hyaloidal contraction (43).
Silicone oil is the tamponade of choice for many PRRDs repaired by primary or repeat vitrectomy, whether or not in combination with scleral buckle. Complications of silicone oil in children are similar to those seen in adults: secondary intraocular pressure elevation, band keratopathy, oil emulsification (Fig. 50.4), and cataract.
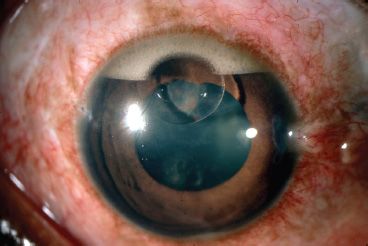
FIGURE 50.4 Emulsified silicone oil accumulated in the superior anterior chamber angle (“inverse hypopyon”) in a child.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


