CHAPTER 5
Testing Methods for Inhalant Allergy
The directing physician has decided that both the practice and the patients will benefit if the office provides allergy care. The earlier chapters have emphasized the importance of allergy as a medical problem, outlined the basic material necessary for diagnosing the condition, and set the stage for proceeding to providing therapy.
In previous chapters, basic screening procedures for inhalant allergy, and even an initial limited screening procedure for food sensitivity, were described. Although such screening provides an adequate initial approach to determining the patient’s overall status, more definitive studies are needed before treatment that includes immunotherapy is undertaken.
COMPLETING THE TESTING FOR INHALANT ALLERGY
Although it is axiomatic that the initial diagnosis of allergy is made by history and physical examination, the findings must be confirmed by tests that identify the specific causative antigens if the investigator wishes to be certain of the diagnosis and to treat the patient effectively. Another condition, or group of conditions, known collectively as nonallergic rhinitis, may mimic true allergy so well that even an experienced examiner can be misled. This is discussed in more detail in Chapter 12. Because proper treatment depends on proper diagnosis, definitive allergy tests are appropriate at this point.
In this era of cost control, ordering or performing a nearly unlimited number of tests for allergy is to be studiously avoided. It is wasteful, unnecessarily expensive, and hard on the patient. Before the specific test methods to be used are selected, therefore, it is well to consider the patient and the plan of approach to treatment.
This chapter discusses techniques for completing the identification of inhalant allergens initiated with limited screening tests. Most clinicians adding allergy to their practice begin with the treatment of inhalant allergy only, as this is the best-understood form of allergy at present and offers the best possibility of a clear diagnosis and good treatment results.
Before any tests are initiated, however, the patient’s motivation must be considered. How persistent are the symptoms, and how severe? If the symptoms are of brief duration and limited to a certain location or a particular season, specific testing may not be necessary. Although immunotherapy offers the only proven “cure” for allergy, and although environmental control is the ideal (if often unattainable) means of management, as a rule any control of symptoms that can be obtained by either of these means can also be obtained by proper medication. Thus, if no specific treatment by immunotherapy is planned, it may not be necessary to identify specific offenders. Here, the patient must be consulted. If the patient wants to know the offender, regardless of the treatment plan, reliable testing is available. It is always nice to know where one stands in regard to offenders, but it is difficult to explain to the patient (or insurer) why a wide range of expensive tests were ordered so that offenders could be identified, and then an antihistamine was prescribed. This could have been done by history alone, without the tests. Specific testing is indicated when the patient wishes to know the offenders, when treatment by environmental control is to be undertaken (so as to practice effective avoidance measures), or when immunotherapy is to be considered.
Let’s assume that specific testing is to be performed. Today, a wide range of testing modalities pertaining to inhalant allergy is available to the physician, but no laboratory test available today is reliable for most forms of food sensitivity, although some may be useful for screening. Reliable tests are available for inhalant allergy alone (even these are not 100% reliable, but very nearly so). Because unlimited testing is not an option, how should the situation be approached?
SCREENING: THE FIRST STEP
A good history is the key for selecting allergens to be tested. Usually, third-party payers accept only a limited number of allergens in an initial battery, with anywhere from eight to 15 being a typical number. If the patient’s symptoms are of pollinosis and present only in the fall, an appropriate initial battery of allergens would be a selection of local weeds. If the problems occur in an old house, dust, mold, and probably epidermals should be tested. This allows the physician to customize testing to maximize the range with the best possibility of obtaining positive results. The main purpose of a screen is to establish the presence of allergy in the patient’s makeup. It is not expected to catch all significant allergens. After the presence of allergy has been established, additional testing is indicated. Again, the selection of tests should be dictated by the history. At times, additional tests performed after a positive screening examination will incriminate antigens not initially suspected.
Previously, one popular screening method, especially with physicians seeking to determine which patients to refer for further allergy investigation, was the use of a dipstick technology, in which serum samples were reacted with dipsticks coated with various regional antigens, yielding a qualitative assessment of the presence of specific immunoglobulin E (IgE). Unfortunately, the manufacturer of that technology (Quidel) has discontinued that product. A similar technology is available in Europe as the Xenith Allergen Screening Program, but no U.S. antigen panels are available (www.xenithbiomed.com/allergy.htm).
Although several methods are in use today to identify specific inhalant allergens, they are of two basic types: in vivo tests (for all practical purposes these are skin tests, although provocation tests are used in research centers), and in vitro tests (tests performed on the patient’s blood, usually by a reference laboratory). Most clinicians adding allergy to an already active practice will probably initially opt for in vitro tests, as little or no equipment is required (if a reference laboratory is utilized), and the results are easily applicable to patient treatment. If the treatment to be used is immunotherapy, a certain amount of skin testing will still be needed at some point, but this is not an immediate requirement. The necessary equipment for various forms of therapy is discussed in the section on getting started in Chapter 3.
Although most new allergy practices may benefit from the initial use of in vitro tests, this is not always the case. Many practices have thrived from the beginning using skin testing alone. In addition, in many regions of the country third-party payers may provide a strong incentive not to perform in vitro testing, despite the fact that it has been shown to be cost-effective when screening is done properly. All these factors may influence the type of testing selected.
In vivo screening skin tests may consist of intradermal dilutional testing (IDT) performed for a limited number of antigens, with expansion of the testing panel based on the initial results. Another convenient skin test screen involves the multiple prick-puncture test (e.g., Multi-Test, Quintest) that allows testing to be performed for several antigens with a minimum of effort. Specific details of these tests are presented later in this chapter.
Although allergy testing as a preliminary step to immunotherapy is not always an ideal approach from the physician’s point of view, as a practical matter most patients seeking allergy care are prepared for immunotherapy. Because a large percentage of antiallergic medical products have become available over the counter, and because the public has been bombarded with information in the media regarding allergy, most patients have already tried and rejected, or at least felt dissatisfied with, this approach, and want something more definitive. They may have used these products and information incorrectly, but if the physician merely recommends using correctly a product already tried, the patient might try another physician instead. Patients usually want to try an approach significantly different from the ones already tried.
Regardless of the initial type of screening test for allergy, an understanding of the underlying principles involved and of the risks and benefits of both in vitro and in vivo tests is necessary to make proper decisions and to apply the correct test in a proper manner. There is a close scientific relationship between the two types of test. In the early days of in vitro testing, a popular belief was fostered that the tests were basically completely different in nature, and therefore not comparable. This is not accurate. A simple way to compare the two types of test is to think of the in vitro test as an advanced technologic means of performing the in vivo test. This may be an oversimplification, but it is a useful approach in understanding the principles involved.
IN VIVO TESTS
In vivo testing, or skin tests, are considered first, as these were the first allergy tests to come into practical use. They have been refined and upgraded through the years, and various degrees of quantification have been added. The in vivo tests are the best known and best understood type of allergy test, and understanding in vivo testing makes it easier to understand in vitro testing. The underlying physiologic principle of the two types of test is the same. All that differs is the method of measurement.
Essentially, all inhalant allergy is produced by IgE, a bodily substance present in more than trace amounts in only about 20% of the population. IgE is present in the skin, serum, and most bodily organs. Because the skin contains IgE (including the specific form for all antigens to which the patient is allergic), applying an allergen via injection or even on an abraded area of skin results in a wheal-and-flare reaction in the patient sensitive to that allergen. (The wheal is the raised area in the center of the test site, whereas the flare is the erythematous area surrounding the site.) The specificity and sensitivity of this reaction depend on the strength of the antigen preparation applied and on the method of application. Skin testing is the oldest form of allergy testing, and was first described in 1865. Accurately controlled skin testing that includes some degree of quantitation dates to about 1910.1
Factors Affecting Skin Test Results
The size of a skin test reaction is influenced by several factors, including the volume and potency of the antigen injected, the depth to which it is introduced (precutaneous or intracutaneous), the degree of sensitization of mast cells in the skin, and the reactivity of the skin to histamine and other mediators released as a part of the allergic reaction. Furthermore, the response may be modified by drugs, the presence of blocking antibodies (from previous immunotherapy), the age and race of the patient, the area of the body injected, the distance separating individual skin test sites, and the time of day of testing.
Intradermal testing introduces antigen in a much more quantified way than do scratch and prick tests. In intradermal testing, the size of the initial wheal is related directly to the volume injected. For example, 0.01 mL is said to produce a wheal of about 4 mm in diameter, which enlarges to about 5 mm because of physical spreading. If the volume injected is increased to about 0.05 mL, the resulting wheal size is about 7 to 9 mm.
Because intradermal tests introduce much more antigen than do prick tests, intradermal tests should either be preceded by a screening prick test or (as in IDT) be performed with sequentially more concentrated antigen solutions, starting with a weak and anticipated nonreacting concentration.
The reactivity of the sensitized skin mast cells and the degree of antigenicity of the solution injected affect the amount of histamine and other vasoactive amines liberated as a result of the skin test, and ultimately affect the size of the resultant wheal. The skin of some individuals is overly responsive to trauma, and a wheal-and-flare response (called dermatographia) is seen in these patients even following the injection of an inert substance. For this reason, a negative control of an inert substance, such as diluent, is always necessary in skin testing.
Increasing amounts of allergen exposure have the same effect on skin reactivity as the use of stronger testing antigen solutions: both result in the production of a more intense skin reaction. Thus, patients are usually found to be more sensitive to skin testing performed during the season of the pollen that affects them, or after increased exposure to a perennial antigen. The results obtained during this “coseasonal” testing may often indicate a higher degree of sensitivity than those obtained when testing is performed out of season.
Patients who have undergone previous treatment may have altered skin test responses, resulting from changes in both IgE and IgG formation. As a practical matter, the existing state of the patient’s immune system is generally accurately reflected in the response to skin testing. In vitro studies, which measure only IgE, fail to take into account the effect of IgG “blocking antibody” formed as a response to prior allergy injections.
The skin of some patients, especially infants and the elderly, is said to be less reactive to skin testing than that of the population as a whole. A general decline of skin reactivity after the age of 50 has been described, although in vitro tests have shown that allergy continues to exist unabated in this age group.
The area of the body where skin tests are applied may affect the responses obtained. Decreasing reactivity of skin occurs in the following order: middle and upper back > lower back > upper arm > forearm (ulnar > radial) > wrist. Intradermal testing is performed on the upper arm rather than the back to allow the placement of a tourniquet above the injection site in case of a reaction. Because prick tests are less likely to result in a systemic reaction, they are often performed on the back.
Axonal reflexes may affect the results of a skin test. Positive skin tests (or positive reactions to histamine controls), if placed too near other skin tests, can initiate axonal reflexes that drive the wheal-and-flare response. Thus, the histamine control should be placed well away from other tests, and individual skin tests should be separated by at least 2 cm. The skin is said to be up to 2.5 times more responsive to tests applied between 7:00 and 11:00 p.m. than to those applied at 7:00 a.m. This variable affects only the most conscientious allergist.
Antihistamines suppress the wheal-and-flare response. With almost all common antihistamines, this effect for all practical purposes ceases within 24 hours or less of the delivery of the last medication to the body, and skin testing may be performed if the patient has taken no such drugs for 36 to 48 hours. Short-acting antihistamines such as diphenhydramine (Benadryl) and triprolidine (Actifed) can sometimes be taken even the day before testing without affecting skin test responses. A notable exception was astemizole (Hismanal), which is no longer available in most countries. The presence of normal skin reactivity should be confirmed by a positive histamine control before further testing is performed. It is important to remember (and to remind patients) that antihistamines are also contained in or include soporifics, cough syrups, “cold” remedies, antipruritics, and anxiolytics.
Tricyclic antidepressants, such as doxepin (Sinequan) and amitriptyline (Elavil), have been observed to suppress skin test responses for from 2 to 4 days after the last dose of the compound has been administered. Decongestants, cromolyn, corticosteroids, and bronchodilators do not affect skin test results.
As a practical matter, patients should be advised to omit antihistamines for 48 hours before allergy testing. Patients on tricyclic antidepressants should discontinue them for 4 days before testing, if at all possible.
Forms of Skin Testing
Several forms of skin testing are in common use today. In many cases, a combination of methodologies is used to produce better results. These methods are reviewed individually.
SCRATCH TEST
This is one of the older forms of skin testing. A small drop of a fairly concentrated extract of an allergen is applied to the skin, and the drop is scratched through with a sharp instrument, breaking only the surface layer of skin. In a variation of this technique, the scratch is made first and the drop of allergenic extract is applied to the scratched area. Results are read on a 0 to 4+ scale of reactivity. This test has been evaluated by the American Medical Associations Council on Scientific Affairs, which in 1987 advised that scratch testing resulted in too many false-positive and false-negative responses to be considered a reliable diagnostic test. Although scratch testing is still performed by some practitioners, use of the test has declined precipitously since the late 1980s and will probably be replaced entirely by more reliable tests as time goes on. One specific problem with the scratch test has been that the mechanism of the test is to induce the release of histamine from the skin, and histamine has a triple reaction, one of which is to produce an axon reflex. When several negative tests are performed close together, followed by a strongly positive test, the axon reflex from the positive test may ignite a false-positive reaction in the nearby tests, which were previously read as negative.2 This contributes to the unreliability of the test. Furthermore, in scratch testing, quantification of the amount of antigen introduced is extremely poor. As it can be completely replaced by more comprehensive tests, the scratch test will not be missed.
One invalid use of the scratch test has been in small children. For some time, it has been common practice to perform scratch tests in children under the age of 4 to determine sensitivity to both inhalants and foods. It is rare, but not impossible, to see inhalant allergy in a child of this age. On the other hand, food sensitivity is common in this age range, but it is rarely IgE mediated. Because scratch testing is generally not considered reliable for other than IgE-mediated disease, scratch tests for food sensitivity that did not produce a positive wheal-and-flare reaction were interpreted as negative and the parent was informed that the child was not sensitive to foods. These negative skin reactions often discouraged the parent and the physician from further investigation to show that an adverse reaction to foods might be based on other than IgE production. This in turn often led to a failure to identify a real problem that, had it been identified and corrected, could have prevented future difficulties.
PRICK TEST
The prick test has been in use since about 1910, and today it remains the standard method employed by a large percentage of allergists. In many ways similar to the scratch test, the prick test is nonetheless much more reproducible.
In performing the test, the upper layer of the skin is lifted with the point of a sharp instrument, most frequently a needle, and allowed to drop back. The goal is not to penetrate the skin but to produce a small prick in the upper skin layers (Fig. 5-1). A drop of antigen extract, at a concentration of 1:10 to 1:20 weight/volume (w/v), is then placed on the pricked spot, and after 15 to 20 minutes the result is read. A variation in this technique, which has become more popular, is to place the antigen on marked areas of the skin first, then prick through the drop of antigen. Results are rated on a scale of 0 to 4+, comparing the responses with a positive (histamine) and negative (diluent or glycerine) control.3 In prick testing, the size of both the wheal and the flare produced by the test are measured and recorded.
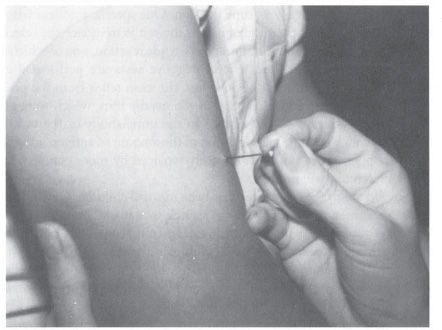
Figure 5-1 Prick test. In the earliest forms of prick testing, almost any sharp instrument, most frequently a needle, was used to prick only into the upper layers of skin, as shown. Before or after the prick, a drop of antigen was placed on the pricked area, and the skin reaction interpreted after 10 to 15 minutes. Accuracy was limited by the variability of skin penetration.
A problem associated with the mechanics of prick testing has been the use of the “prick and wipe” technique. For speed, the test has often been applied with one needle per patient, wiping any antigen off the point between sticks. Of course, cross-contamination with antigens is possible if the needle is not adequately cleaned between pricks. Fears of personnel suffering needle sticks using this prick and wipe method has led to a recommendation by the Occupational Health and Safety Administration that the technique be changed, so that each stick is performed with a needle that is then discarded into a sharps container before a new needle is used for the next stick.4 Although some proponents of the prick and wipe technique continue to use this method, other methods are gaining in popularity.
In the early days of allergy testing, the prick test suffered from a lack of uniformity, both in testing and results. Through the years, the variability inherent in performing a test of this type became evident, and newer and better means of administering the prick were developed. Today, instruments are available to administer the prick in a uniform manner each time, based on a controlled depth of penetration, usually 1 mm (Fig. 5-2). Further advances have produced instruments that apply the antigen at the same time the prick is administered; the drop of antigen is carried in a rosette of tiny needles (Fig. 5-3). These instruments penetrate the skin to a somewhat deeper level than do the single-pointed instruments, delivering a somewhat larger, although uniform, amount of antigen into the skin. This produces a reaction closer to that seen in an intradermal test than with the single-pointed instrument (Fig. 5-4).
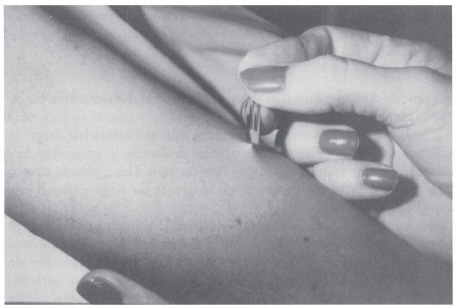
Figure 5-2 The prick test, administered manually. A drop of test antigen is placed on the skin and the skin is “pricked” with a sharp instrument, lifting the skin and releasing it without penetrating through it. The results are more reliable than the scratch test, but still subject to variables ranging from proficiency of administration to individual skin reactivity.
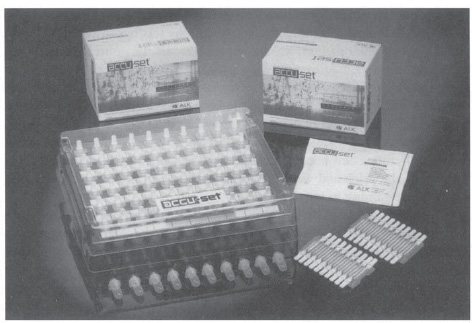
Figure 5-3 Multiple-pointy single-antigen “pricker”: the Greer Pik (Greer Laboratories, P.O. Box 800, 639 Nuway Circle, Lenoir, NC28645). Further refinements in the prick test format resulted in the development of an instrument carrying a larger amount of antigen and containing six points of measured depth. This yields much more reproducible prick test results.
Unfortunately, there is still no uniformity in designating a single method for reading and reporting the results of prick tests. Table 5-1 shows one of the accepted formats for interpreting the prick test results. Another alternative is simply to compare test wheal-and-flare reactions with those obtained from the positive (histamine) control (Fig. 5-5). In this system, a 2 + reaction is half the size of the histamine control, a 3 + reaction is the same size as the control, and a 4+ result is twice that size. A third suggestion has been to measure the resulting wheal in two dimensions, add the diameters, and divide by two, expressing the result in millimeters, or outlining the wheal in ballpoint pen and transferring the marking to paper using clear tape.5 The exact grading system is probably not as important as consistency and familiarity with the system chosen, which should be indicated on any test results. Clearly, although the uniformity of prick testing has greatly improved, interpreting the test results still allows considerable latitude. Attempts to rate the magnitude of a response to a single prick test continue to be open to serious question.
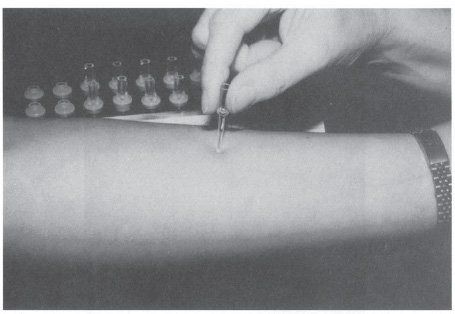
Figure 5-4 Wheal production from the prick test, which characteristically produces both a central area of induration (wheal) and a surrounding area of erythema (flare). Note the responses to the tests already placed.
A variant of the prick test involves a multiple prick-puncture apparatus, such as the Multi-Test device, which consists of two parallel rows of four test heads. Each head contains nine plastic points that are 1.9 mm in length and arranged in a 2 by 2 mm square pattern (Fig. 5-6). Test antigen is applied to the points by a patented applicator and is held to the test head by capillary action. When the device is firmly applied to the skin (with pressure followed by a gentle rolling action), a uniform amount of antigen is delivered to the epidermis and superficial dermis. Positive and negative controls (histamine and glycerine) are applied along with test antigens, and the results are graded on a 0 to 4+ scale as with the prick test. Because of the reproducibility of the amount of antigen delivered, as well as the depth of penetration involved, the Multi-Test may be more comparable with intradermal testing than with a true prick test. Prior studies have confirmed its reproducibility6 and validity as a screening test.7
| Grade | Wheal size | Erythema size |
|---|---|---|
0 | <3 mm | 0–5 mm |
1+ | 3–5 mm | 0–10 mm |
2+ | 5–10 mm | 5–10 mm |
3+ | 10–15 mm | 10–20 mm |
4+ | >15 mm or pseudopods | >20 mm |
* Readings of 3+ and 4+ are considered positive. Wheal and erythema size are the average diameter of the reactions, measured in two axes.
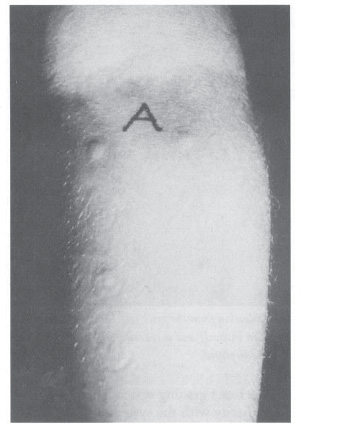
Figure 5-5 Prick test result. A histamine control has been placed (upper left), and the wheal and flare produced by testing with each antigen are compared with the positive control.
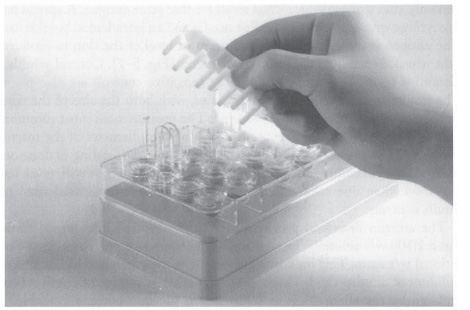
Figure 5-6 The Multi- Test II device. This instrument produces more uniform and reproducible results in comparison with standard prick tests. Testing can generally be performed more rapidly using this device, especially this modification. However, quantification is somewhat more limited than with intradermal titration or RAST. (Courtesy of Lincoln Diagnostics, P.O. Box 1128, Decatur, IL 62525.)
Most allergists do not depend on a single prick test for diagnosis. In the interest of safety as well as accuracy, many initially administer a prick test, which delivers a very small total amount of antigen in comparison with intradermal testing. This initial use of the prick test is a very safe means of screening to identify patients with high degrees of sensitivity. If the prick test result is negative, it is safe to progress to an intradermal test, if indicated. It should be emphasized that stopping testing after a negative prick test result may lead to failure to identify patients with lower degrees of hypersensitivity that may materially contribute to symptom production. To screen fully for inhalant allergy using the prick test requires a follow-up intradermal test for patients who are negative prick reactors.
INTRADERMAL TEST
The intradermal test is a more definitive means of evaluating specific allergic sensitivity. General allergists usually utilize antigen at a 1:100 w/v concentration for single-dilution intradermal testing, testing only with this concentration and only after a negative prick test result for that same antigen. A special testing syringe with an incorporated fine needle and an intradermal bevel is used. The antigen is introduced into the outermost level of the skin to produce a skin wheal, generally 2 to 3 mm in diameter (Fig. 5-7). Control wheals of histamine (positive control) and diluent (negative control) are also placed. The results are read after 15 to 20 minutes, with both the size of the wheal and the surrounding erythema measured. The measurement most commonly used is the average of the maximum and minimum diameter of the reaction produced. The presence of pseudopods is also noted. Grading is done on a 0 to 4+ scale, in comparison with controls.3 Unfortunately, as with prick testing, more than one schema for reporting single-dilution intradermal test results is in use.
The antigen described previously for single-dilution intradermal testing was a 1:100 w/v solution. Today, most antigens may be purchased in the traditional w/v form. This indicates the weight of the antigen in milligrams per milliliter of diluting fluid. This older designation of antigen strength is being replaced by the allergy unit as standardized vaccines become available. To date, the number of antigens for which standardized extract is available is limited, but as it becomes available the standardized form is replacing the w/v form by government regulation. Details in this are presented in Chapter 9; however, for comparison of testing techniques, only the older w/v measurement is used, to avoid confusion.
Like the single prick test, a single intradermal test may present difficulty in interpretation. Furthermore, as in prick testing, several methods of reporting intradermal test results exist. The responses to a prick test followed (if negative) with an intradermal test indicate either a high degree of sensitivity (positive prick test), a low degree of sensitivity (only a positive intradermal test), or no demonstrable sensitivity. This is generally quite adequate if the mode of therapy is to be environmental control, in which case only the major offenders need to be identified, or if pharmacotherapy is to be the treatment approach. (In this case, however, it is reasonable to question the need for specific testing at all.) For immunotherapy, this approach is acceptable and has been in use for many decades, but it is far from optimal. Most otolaryngologists, and many other practicing physicians, have felt dissatisfied with the approach described and wished for greater accuracy and quantification of sensitivity to treat effectively by immunotherapy. This desire led to the development of skin end-point titration (SET), once called serial dilution end-point titration (SDET), and more recently termed intradermal dilutional testing (IDT). In this book, we use the generally accepted term, IDT.
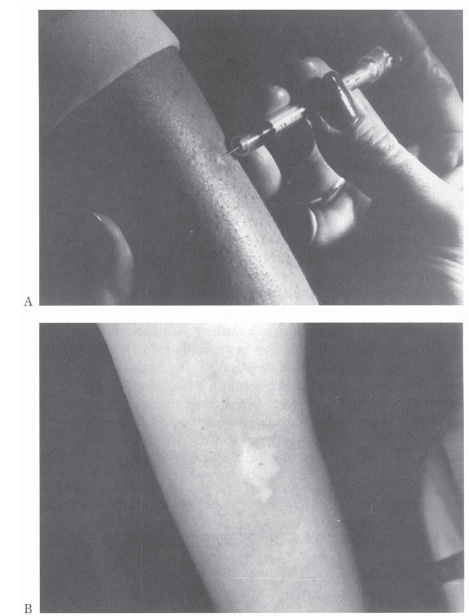
Figure 5-7 A: Intradermal testing: proper technique. The material is deposited in the outer layers of the skin; the wheal produced should be regular and firm. B: Limitations of quantification of a single intradermal test with a strong response. Note the pseudopods and irregular erythema.
INTRADERMAL DILUTIONAL TESTING (SKIN END-POINT TITRATION)
IDT evolved progressively from the 1930s through the early 1960s. In principle, it is not a different approach to skin testing, but rather a refinement of the format described previously, in which testing involves introducing small quantities of antigen initially, followed by larger amounts if necessary. In the IDT method, quantification of the various allergens tested is accomplished by serially diluting concentrated extracts on a 1:5 basis (i.e., 1 mL of antigen diluted with 4 mL of diluent) and administering them in a sequential fashion, starting with an anticipated nonreactive strength. The fivefold dilutions advocated by Rinkel, the father of IDT, were found to provide much more highly reproducible results than the 1:10 dilutional system in general use at the time.
One of the advantages of IDT is that regardless of the source of any given concentrate, a bioassay for sensitivity is performed in each individual patient for that antigen, and the antigens for treatment come from the same material used in testing. The results of IDT testing indicate a safe starting dose for immunotherapy. The technique of IDT involves testing the individual patient with specific antigens, starting with a test dose anticipated to be both safe and nonreactive. This is generally a #6 (1:312,500) dilution, although in specific circumstances (detailed later in this chapter), an experienced and skilled tester may begin at a #4 dilution (1:12,500). Testing involves progressively applying stronger concentrations of the antigen in a controlled manner until evidence of sensitivity is demonstrated. At the point at which a definite sensitivity to the allergen is demonstrated, the testing may stop, with this point indicating a safe level at which to initiate immunotherapy.
NURSE’S NOTE
Several factors influence the dilution at which IDT may begin. These include the following:
1. Experience of the tester
2. Season and circumstances affecting current antigen exposure (the greater the exposure, the greater the expected sensitivity)
3. Antigen involved (grass is especially potent)
4. Status of the patient, A “brittle” patient, such as an asthmatic person or a patient with a history of prior severe reactions, should always be started with a very dilute (#6) antigen.
Antigen Variability and the Benefits of IDT
In a few instances, commercially prepared extracts for some unusual allergenic offenders are difficult to procure. When such extracts are available, the potency may vary significantly between different suppliers and at times between different batches of extract prepared by the same supplier. Two or three decades ago, this variability was the rule rather than the exception. Such variability was often the cause of adverse reactions in patients undergoing skin testing and/or immunotherapy. Because at that time the number of commercially available extracts was much more limited than today, many active clinicians were forced to depend on antigen suppliers with less than optimal quality control, or even to prepare their own extracts. Inevitably, the uniformity of the antigens produced suffered greatly, but with IDT it was possible to compensate for this by comparing the product, regardless of uniformity, with the patient’s own skin response and initiating therapy based on this response level. Provided that the allergenic extract, regardless of the source, had been adequately tested for safety, the results were still successful.
The preceding historical note puts into perspective ongoing developments affecting available concentrations of allergenic extracts, which may in turn have a major effect on established treatment programs. The switch from w/v to standardized extracts is still in progress, and will probably remain so for a prolonged period of time. Converting established immunotherapy maintenance programs to new formats and initiating new treatment programs will present a problem for quite a while. Until the situation is stable, however, no simple conversion pattern can be useful. More about handling this situation is discussed in Chapter 9. To apply the conversion factors as they become available and to understand the changes that must be made as this occurs, it is necessary to understand the previously uniform format of IDT, as all such changes must be applied to this format.
NURSE’S NOTE
Antigen manufacturers are frequently able to be of great help in the conversion from w/v to standardized extracts (from the same antigen supplier). They have information available that indicates the relationship of the previous and new antigens, and they generally share this information to assist in the transition.



