FIGURE 4.1 Schematic diagram of collagen fibril structure in the human vitreous. (From Bishop PN. Structural macromolecules and supramolecular organisation of the vitreous gel. Prog Retin Eye Res 2000;19:323–344, with permission.)
Type II Collagen
Type II collagen, a homotrimer composed of three identical alpha chains designated as [α1 (II)]3, comprises 75% of the total collagen content in vitreous. When first synthesized as a procollagen and secreted into the extracellular space, type II collagen is highly soluble. The activity of N-proteinase and C-proteinase enzymes reduces the solubility and enables type II collagen molecules to cross-link covalently in a quarter-staggered array. Within this array are likely to be N-propeptides, which probably extend outward from the surface of the forming fibril (5). This may influence the interaction of the collagen fibril with other components of the extracellular matrix. Recent studies (8) combined immunolocalization with Western blot analysis of macromolecules extracted from bovine vitreous collagen fibrils and found that the pN-type IIA procollagen is located on the surface of the vitreous collagen fibril. The findings (9) that type IIA procollagen propeptides bind growth factors such as transforming growth factor-β1 and bone morphogenic protein-2 support the concept that growth factors interact with vitreous fibrils to at times promote enough cell migration and proliferation to result in proliferative vitreoretinal disorders, such as proliferative vitreoretinopathy in adults and retinopathy of prematurity in infants.
Type IX Collagen
Type IX collagen is a heterotrimer that is disulfide bonded with an [α1 (IX) α2 (IX) α3 (IX)] configuration. It is oriented regularly along the surfaces of the major collagen fibrils in a “D periodic” distribution, where it is cross-linked onto the fibril surface. Type IX is a member of the fibrillar-associated collagens with interrupted triple helixes group of collagens. It contains collagenous regions described as COL1, COL2, and COL3 interspersed between noncollagenous regions called NC1, NC2, NC3, and NC4 (10,11). In vitreous, as opposed to cartilage, the NC4 domain is small and not highly charged, thus not likely to exhibit extensive interaction with other extracellular matrix components (12). In vitreous, type IX collagen always contains a chondroitin sulfate GAG chain (10,11), which is linked covalently to the α2 (IX) chain at the NC3 domain, enabling the molecule to assume a proteoglycan form. Electron microscopy of vitreous stained with cationic dyes visualizes the chondroitin sulfate chains of type IX collagen, occasionally found distributed along the surface of vitreous collagen fibrils (13) and often bridged between neighboring collagen fibrils. Duplexing of GAG chains from adjacent collagen fibrils may result in a “ladderlike” configuration (14).
Type V/XI Collagen
Ten percent of vitreous collagen is a hybrid V/XI collagen that is believed to comprise the central core of the major collagen fibrils of vitreous (15). Type V/XI is a heterotrimer that contains α1 (XI) and α2 (V) in two chains, while the nature of the third chain is presently not known (16). Along with type II collagen, type V/XI is a fibril-forming collagen. While the interaction of the fibril with other extracellular matrix components is probably influenced by a retained N-propeptide that protrudes from the surface of the fibril in cartilage (15), it is not known whether this is the case in vitreous (6).
Type VI Collagen
Although there are only small amounts of type VI collagen in vitreous, the ability of this molecule to bind both type II collagen and hyaluronan (HA) suggests that it could be important in organizing and maintaining the supramolecular structure of vitreous gel.
Glycosaminoglycans
GAGs do not normally occur as free polymers in vivo but are covalently linked to a protein core, the ensemble called a proteoglycan. A sulfated group is attached to oxygen or nitrogen in all GAGs except HA. Studies in the rabbit (17) found a total vitreous GAG content of 58 ng with 13% chondroitin sulfate and 0.5% heparan sulfate.
Hyaluronan
Although HA is present throughout the body, it was first isolated from bovine vitreous. HA appears in human vitreous after birth possibly synthesized by hyalocytes (18), although other plausible candidates are the ciliary body and retinal Müller cells. HA is synthesized at a constant rate in the adult. Although there is no extracellular degradation, HA levels are in a steady state because the molecule escapes via the anterior segment of the eye (19).
HA is a long, unbranched polymer of repeating glucuronic acid β-1,3-N,N-acetylglucosamine disaccharide moieties linked by β 1–4 bonds (20), with a molecular weight of 3–4.5 × 106 in adult human vitreous (19). HA is a linear, left-handed, threefold helix with a rise per disaccharide on the helix axis of 0.98 nm (21). This periodicity, however, can vary depending on whether the helix is in a “compressed” or “extended” configuration (22). Changes in the degree of “extension” of HA could be important in retinal disease, since the volume of the unhydrated HA molecule is about 0.66 cm3/g, whereas the hydrated specific volume is 2,000 to 3,000 cm3/g (19). Thus, the degree of hydration has a significant influence on the size and configuration of the HA molecular network. HA also interacts with the surrounding mobile ions and can undergo changes in its conformation that are induced by changes in the surrounding ionic milieu (23). A decrease in surrounding ionic strength can cause the anionic charges on the polysaccharide backbone to repel one another, resulting in an extended configuration of the macromolecule. An increase in surrounding ionic strength can cause contraction of the molecule and, in turn, the entire vitreous body. As a result of HA’s entanglement and immobilization within the vitreous collagen fibril matrix, this mechanical force can be transmitted to the retina, optic disc, and other structures, such as neovascular complexes. This can be important in certain pathologic conditions that feature fluctuations in ionic balance and hydration, such as diabetes (24), especially type I diabetes in children who have a solid gel vitreous firmly adherent to retina.
Chondroitin Sulfate
Vitreous contains two chondroitin sulfate proteoglycans. The minor type is actually type IX collagen, which was described earlier. The majority of vitreous chondroitin sulfate is in the form of versican; concentration = 0.06 mg protein/mL, about 5% of the total protein content (25). This large proteoglycan has a globular N-terminus that binds HA via a 45-kDa link protein (26). In human (but not bovine) vitreous versican is believed to form complexes with HA as well as microfibrillar proteins, such as fibulin-1 and fibulin-2 (6).
Heparan Sulfate
This sulfated proteoglycan is normally found in basement membranes and on cell surfaces throughout the body. It was first detected in bovine vitreous in 1977 (27) and in chick vitreous (as “agrin”) in 1995 (28). However, it is not clear whether heparan sulfate is a true component of vitreous or a “contaminant” from adjacent basement membranes, such as the internal limiting lamina of the retina (29). As pointed out by Bishop (6), this may also be the case for nodogen-1, the aforementioned fibulins, and fibronectin.
Noncollagenous Structural Proteins
Fibrillins
Fibrillin-containing microfibrils are more abundant in vitreous than type VI collagen microfibrils. They are found in vitreous gel as well as in the zonules of the lens, explaining why in Marfan syndrome defects in the gene encoding fibrillin-1 (FBN1 on chromosome 15q21) result in both ectopia lentis and vitreous liquefaction (6). The latter probably plays a role in the high incidence of rhegmatogenous retinal detachment in these patients.
Opticin
The major noncollagenous protein of vitreous is a leucine-rich repeat (LRR) protein, which is bound to the surface of the heterotypic collagen fibrils, known as opticin (30). Formerly called vitrican, opticin is believed to be important in collagen fibril assembly and in preventing the aggregation of adjacent collagen fibrils into bundles. Thus, a breakdown in this property or activity may play a role in age-related vitreous degeneration (31). A recent study (32) attempted to determine the structure, location, and expression of the mouse opticin gene (Optc). The gene was found to be localized to mouse chromosome 1, consisting of seven exons. Additionally, in situ hybridization revealed that opticin mRNA is localized exclusively to the ciliary body during development and to the nonpigmented ciliary epithelium of the adult mouse eye. The researchers concluded that opticin may represent a marker for the differentiation of ciliary body. Besides regulating vitreous collagen fibrillogenesis, it may also have other functions as demonstrated by its continued expression in the adult mouse eye. Indeed, Bishop and colleagues recently demonstrated that opticin is capable of modulating neovascularization in the posterior segment. In their study, an opticin knockout mouse and a wild-type mouse were compared in an oxygen-induced retinopathy model. Although the knockout mouse initially had normal vascular development, following exposure to high oxygen conditions the knockout model developed significantly more preretinal neovascularization. Additionally, intravitreal injections of opticin into the wild-type mouse significantly reduced preretinal neovascularization when exposed to the oxygen-induced retinopathy conditions (33).
Supramolecular Organization
Bishop (6) has emphasized the importance of understanding what prevents collagen fibrils from aggregating and by what means the collagen fibrils are connected to maintain a stable gel structure. Chondroitin sulfate chains of type IX collagen bridge between adjacent collagen fibrils in a ladder-like configuration spacing them apart (34). This arrangement might account for vitreous transparency, in that keeping vitreous collagen fibrils separated by at least one wavelength of incident light would minimize light scattering and allow unhindered transmission of light to the retinal photoreceptors. However, depolymerizing with chondroitinase does not destroy the gel, suggesting that chondroitin sulfate side chains are not essential for vitreous collagen spacing. Complexed with HA, however, the chondroitin sulfate side chains might space apart the collagen fibrils (14,34), although Bishop believes that this form of collagen–HA interaction is “very weak.” Instead, he proposes that the LRR protein opticin is the predominant structural protein in short-range spacing of collagen fibrils. Concerning long-range spacing, Scott (14) and Mayne et al. (35) have claimed that HA plays a pivotal role in stabilizing the vitreous gel via this mechanism. However, studies (36) using HA lyase to digest vitreous HA demonstrated that the gel structure was not destroyed, suggesting that HA is not essential for the maintenance of vitreous gel stability, leading to the proposal that collagen alone is responsible for the gel state of vitreous (6).
Total collagen content in the vitreous gel remains at about 0.05 mg until the third decade (2). As collagen concentration does not appreciably increase during this time but the size of the vitreous increases, the network density of collagen fibrils effectively decreases, potentially weakening the collagen network and destabilizing the gel. However, since there is net synthesis of HA during this time, it likely stabilizes the thinning collagen network (19).
Pharmacologic vitreolysis (1,2) refers to the use of drugs to alter molecular structure and induce liquefaction, vitreoretinal dehiscence, and innocuous posterior vitreous detachment (PVD). Further, pharmacologic vitreolysis may improve intraocular physiology and metabolism (37). To date, investigators have used pharmacologic vitreolysis in diseases such as diabetic retinopathy (38), macular holes (39), retinopathy of prematurity (40), and congenital retinoschisis (41). Since initial attempts all used enzymes as adjuncts to surgery, the term “enzymatic vitreolysis” was prevalent in the early literature (42,43). However, in 1998, the term “pharmacologic vitreolysis” was proposed (2) so that vitreolytic agents could be grouped according to their mechanisms of action as either “enzymatic” or “nonenzymatic.” Furthermore, it was proposed that these agents could be subcategorized as either nonspecific agents, such as tissue plasminogen activator (44), plasmin (45,46), microplasmin (known now as ocriplasmin) (47,48), and nattokinase (49), or substrate-specific agents, such as chondroitinase (18,50,51), dispase (52,53), and hyaluronidase (51,54,55). Since there are only two nonenzymatic agents (urea/Vitreosolve) (56) (no longer under development) and RGD peptides (those composed of amino acids, l-arginine, glycine, and l-aspartic acid) (57), it would seem that an alternative classification might be more useful, especially if based upon biologic activity. Thus, pharmacologic vitreolysis agents have recently been reclassified (Table 4.1) based upon the ability to induce liquefaction (“liquefactants”) or whether they induce dehiscence at the vitreoretinal interface (“interfactants”). Of note is that several agents have both liquefactant and interfactant properties.
TABLE 4.1
Pharmacologic vitreolysis classification based on biologic activity
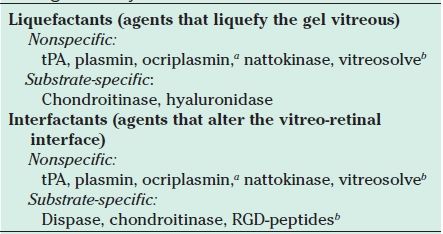
aFormerly known as microplasmin.
bNon enzymatic agents.
Source: Sebag J. Pharmacologic vitreolysis-premise and promise of the first decade. Retina 2009;29(7):871–874.
Note: tPA, tissue plasminogen activator; plasmin, ocriplasmin,a nattokinase, vitreosolve are believed to be both liquefactants and interfactants and RGD, rginine-glycine-aspartic acid.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


