CHAPTER 16
Allergic Fungal Sinusitis
The impact of fungus upon the pathophysiology of chronic inflammatory disease of the nose and paranasal sinuses has received a great deal of attention during the past decade or more. Few aspects of this issue have received more recent attention than the entity known as, allergic fungal sinusitis (AFS). Because of its allergic aspects, AFS is important to all rhinologists, especially to those dealing with allergy. AFS must be differentiated from other pathophysiologic states in which fungal organisms affect the paranasal sinuses. Included in this group are invasive fungal sinusitis (which can be further subclassified as fulminant, indolent, or granulomatous), noninvasive fungus balls (previously known as mycetomas), and saprophytic fungal growth on crusts and purulent exudate within diseased sinuses.1 AFS is the only one of these disorders with an allergic component, which must be understood (and managed) to provide the greatest likelihood of control in this typically recalcitrant disease.
HISTORICAL BACKGROUND
AFS was originally termed allergic Aspergillus sinusitis and was felt to represent the sinonasal equivalent of allergic bronchopulmonary aspergillosis (ABPA). The diagnostic criteria for ABPA include bronchial obstruction, eosinophilia, positive immunologic test results, positive sputum cultures for Aspergillus, and a history of expectoration of brown plugs (representing fungal debris).2 In 1981, Millar et al.3 first termed this entity allergic aspergillosis of the paranasal sinuses.
The most definitive early study in this area was that of Katzenstein and colleagues,4 who retrospectively reviewed specimens from more than 100 sinus operations, finding seven instances of histologic findings similar to the mucoid impactions found in the bronchi of patients with ABPA. It was All-phin et al.5 who finally suggested that many fungi, not just Aspergillus species, were capable of causing this clinical picture, and also suggested the term now used, allergic fungal sinusitis.
PATHOPHYSIOLOGY
There now is little doubt that AFS is truly an allergic disorder, not a fungal infection. These patients have been shown to have markedly increased total levels of immunoglobulin E (IgE) and positive results on allergen-specific IgE assays for both fungal and nonfungal antigens.6 Results of skin tests for fungal antigens have also been noted to be positive in patients with AFS.7
It has been conjectured that AFS occurs in the same manner as ABPA. The process has been described as a vicious cycle in which fungus, trapped in viscid secretions contained in the constricted airway, results in continued exposure to large quantities of antigenic material. One likely scenario for the development of AFS is that proposed by Manning et al.,8 in which obstruction of the sinus ostia and stasis of secretions may be promoted by allergy and bacterial infection, as well as anatomic abnormalities. When this occurs in patients with a genetic predisposition to atopy, prolonged contact between the sinus mucosa and entrapped fungal elements results in both Gell and Coombs type I (IgE-mediated) and type III (immune complex) reactions. These cause further mucosal edema and polyp formation, plus the formation of an eosinophilic debris termed allergic mucin.
CLINICAL DIAGNOSTIC CHARACTERISTICS
Differential Diagnosis
As already mentioned, other forms of fungal involvement of the sinuses occur, and these must be differentiated from AFS. Invasive fungal sinusitis, which generally affects immunocompromised patients, is characterized by tissue invasion and necrosis, neither of which is seen in AFS. Fungus balls, formerly referred to as mycetomas, are large fungal collections that typically accumulate in one sinus, generally the maxillary or sphenoid, in immunocompetent patients. In these situations, surgical extirpation and marsupialization are curative. It is frequently the case that fungi grow saprophytically in the debris and purulent exudate found in the sinuses of patients with chronic purulent sinusitis. This represents merely a fungal presence, not an infection, and is generally of no clinical significance.
One entity that may present a greater diagnostic challenge has been described by Ferguson,9 who terms it allergic mucin sinusitis. In this situation, the histopathologic picture mimics that of AFS, with the exception of demonstrable fungal forms.
Physical Presentation of Disease
The typical clinical presentation of AFS is chronic pansinusitis with polyposis, often with a history of recurrent problems despite one or more previous sinus operations. If sinus disease is long-standing or severe, bone remodeling may result in proptosis or diplopia. However, other patients may present with simple nasal congestion and purulent sinusitis. These patients are generally young but may range in age from preadolescence to middle age; AFS shows no predilection for either sex. The patients do not show an increased incidence of salicylate sensitivity, and only about one third are asthmatic. Atopy is virtually a universal finding in these patients, who often have allergic rhinitis. Interestingly, many patients with AFS have received immunotherapy previously and have discontinued it because of adverse local or constitutional reactions.
Radiographic Characteristics
The radiographic findings in AFS are typical.10 Multiple sinuses are opacified. Longstanding or severe disease may have caused bone remodeling or erosion involving the lamina papyracea, orbital apex, or cribriform plate. Heterogeneous densities on computed tomography (CT) scans of patients with AFS (Fig. 16-1) have been described and are theorized to result from high levels of magnesium, manganese, and iron in allergic mucin within the sinuses.11 Magnetic resonance imaging (MRI) may be useful, especially if erosion is suspected. OnTl-weighted images, allergic mucin is seen as isoin-tense or slightly hypointense masses, which frequently become completely black on T2-weighted images (Fig. 16-2).
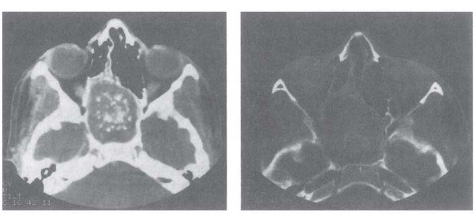
Figure 16-1 Computed tomography (CT) scan of patient with expansile mass of allergic fungal sinusitis involving the sphenoid. Both soft tissue (left) and bone (right) windows demonstrate a typical speckled pattern of high attenuation. (With permission from Manning SC, Merkel M, Kriesel K, Vuitch F, Marple B. Computed tomography and magnetic resonance diagnosis of allergic fungal sinusitis. Laryngoscope 1997;107:170-176.)
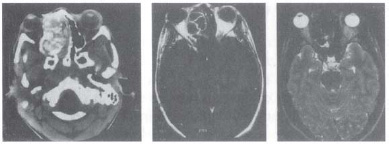
Figure 16-2 Patient with allergic fungal sinusitis involving the right ethmoid and expanding into orbit. The CT scan (left) demonstrates the extent of disease and orbital involvement. The Tl-weighted magnetic resonance imaging (MRI) (center) shows lowsignal in the center of the mass, with a high signal on the periphery. On the T2-weighted MRI (right), the central area demonstrates a void signal. (With permission from Manning SC, Merkel M, Kriesel K, Vuitch F, Marple B. Computed tomography and magnetic resonance diagnosis of allergic fungal sinusitis. Laryngoscope 1997;107:170-176.)
Gross and Histologic Characteristics
Although the disorder may be suspected based on history, physical examination, and radiographic characteristics, surgical and histopathologic findings are able to provide more definitive diagnostic information. At surgery, in addition to polyps and mucosal hyperplasia, sinuses involved with AFS contain a unique material, allergic mucin (Fig. 16-3). This is a thick, viscous, tenacious material that may vary in color from light tan to brown to green to black. Its consistency is sometimes compared with that of axle grease or peanut butter. It is typically very difficult to remove from the involved sinuses, usually requiring irrigation, suction, and painstaking dissection. The accumulation of this material is responsible for the bone remodeling or pressure erosion that characterizes AFS.
Histopathologic examination of allergic mucin reveals characteristic findings of an eosinophilic substrate that, when stained appropriately (using a combined hematoxylin/eosin and silver based stain), demonstrates the presence of noninvasive fungal elements (Fig. 16-4). The substrate is composed of sheets of eosinophils (both intact and in varying degrees of degradation) and contains Charcot-Leyden crystals. These elongated eosinophilic bodies represent the product of eosinophil degradation. They are not specific for AFS and may be found in any secretions rich in eosinophils, such as the sputum of asthmatic patients.

Figure 16-3 Allergic mucin removed from a patient with extensive allergic fungal sinusitis. This thick material, often compared in consistency with peanut butter or axle grease, is a hallmark of allergic fungal sinusitis (AFS).
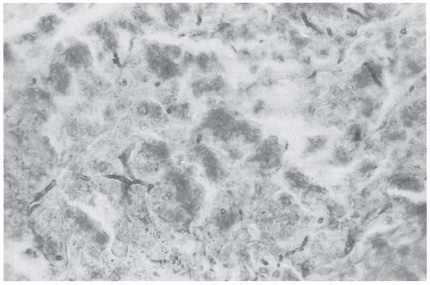
Figure 16-4 Histopathology of allergic fungal sinusitis. On a background of sheets of eosinophils, a fungal stain demonstrates noninvasive fungal hyphae. Clumps of degenerating eosinophils form Charcot-Leyden crystals.
DIAGNOSIS
Epidemiology
Although during the last decade AFS has been recognized as being less rare than initially thought, its exact incidence remains unclear. This is primarily because no single set of criteria for the establishment of this diagnosis have been universally accepted. Even with the varied standards of diagnosis that currently exist, it is estimated that -7% of the cases of chronic sinusitis that require surgery involve AFS.12
The initial descriptions of allergic Aspergillus sinusitis included the common factors of immunocompetence (as opposed to the immune deficiency seen in patients with invasive fungal sinusitis), positive skin test reactions to Aspergillus antigen, other positive serologic findings (high levels of fungal-specific antigen and elevated total IgE), and typical histopathologic findings of allergic mucin containing noninvasive fungal forms.
Corey13 and others have described immunologic characteristics that might suggest preoperatively the presence of AFS. These are derived from those for ABPA, which include peripheral eosinophilia, immediate cutaneous reactivity and the presence of precipitating antigens to Aspergillus, elevated total serum IgE, and elevated levels of Aspergillus-specific IgE and IgG. Such immunologic information may be highly suggestive of AFS. However, clinical characteristics must also be considered in making this diagnosis.
Diagnostic Criteria
Numerous authors have set forth their own diagnostic criteria,14-16 all of which generally include immunocompetence, typical radiographic findings, presence of typical allergic mucin with noninvasive hyphae, and presence of atopy. Among the best known and most used are the criteria set forth by Bent and Kuhn.17 After an analysis of 15 cases of AFS, they found five characteristics common to all (Table 16-1): Gell and Coombs type I hypersensitivity, nasal polyposis, characteristic CT appearance, eosinophilic mucus without fungal invasion, and positive fungal stain of sinus contents removed at surgery They found that a unilateral predominance, a history of asthma, the presence of Charcot-Leyden crystals, and peripheral eosinophilia were often (but not universally) present in their series. Our experience has been similar to theirs, and we base the diagnosis of AFS on the presence in atopic patients of pansinusitis with polyposis, with typical gross and histologic findings of allergic mucin, including noninvasive hyphae.
Gell and Coombs type I hypersensitivity |
Positive skin test results |
Positive in vitro test results |
Strongly positive history |
Nasal polyposis |
Characteristic findings on CT scan |
Clouding of multiple sinuses |
Areas of increased attenuation, especially on bone windows |
Bone destruction and remodeling variably present Allergic mucin |
Typical gross appearance |
Eosinophilic material on histopathology |
Identifiable fungal forms with appropriate fungal stains |
Noninvasive |
Fungal cultures variably positive |
Adapted with permission from Bent JP III, Kuhn FA. Diagnosis of allergic fungal sinusitis. Otolaryngol Head Neck Surg 1994;111:580-588.



