CHAPTER 14
Pediatric Allergy
Allergy is directly or indirectly involved in up to half the problems encountered in the office practice of otolaryngology. This is true whether the patient population under consideration is composed primarily of adults or children. It has been (very conservatively) estimated that allergic rhinitis occurs in 10% of children and 20% of adults.1 Allergy is probably more commonly present in children than current figures indicate, however, as in this age group it more frequently takes the form of food hypersensitivity, a disorder that is easily overlooked or misdiagnosed. Thus, it is necessary that the otolaryngologist whose practice includes pediatric patients recognize the many manifestations of allergy affecting children. Although much of the material in this chapter has been presented elsewhere in this text, it is repeated here to provide, a single reference source regarding allergy as it affects the ear, nose, and throat in children.
SIGNS AND SYMPTOMS OF ALLERGY IN CHILDREN
Allergy may affect every organ system and region within the province of the otolaryngologist. However, in children the physician must more carefully look for signs, as verbalization of corresponding symptoms may be lacking because of patient age or (unfortunately) lack of parental attention to these problems.
Head
It is now well accepted that the typical “adenoid fades,” characterized by mouth breathing, a retrognathic jaw, and a high palatal arch, maybe the result of nasal airway obstruction as well as a hypertrophic adenoid mass. In addition to these features, the child with allergy often demonstrates facial grimacing and wrinkling of the nose, and a gesture referred to as the “allergic salute”: lifting the tip of the nose with an upward sweep of the palm. These gestures result from intense itching of the mucous membranes of the nose, and in many instances the child soon discovers that a beneficial effect of the actions is to lift the nasal tip and briefly improve the airway. Repetition of the allergic salute for a period of years usually results in a permanent creasing of the skin above the nasal tip, and this “supratip crease” is another aid to the diagnosis of allergy in a child.
Other facial stigmata of allergy appear in the region of the eyes. The most characteristic finding is infraorbital puffiness and discoloration, often referred to as an “allergic shiner.” This condition occurs because chronic nasal congestion results in stasis of the venous drainage from the periorbital region. Venous stasis is also postulated to be the cause of “Dennie’s sign”: lines that radiate downward from the inner corner of the eye in the area of the lower lid, attributed to spasm of the unstriated muscle of Muller resulting from poor oxygenation. Allergic children also frequently have long, silky eyelashes, although the cause of this phenomenon remains obscure.
Finally, some children manifest a characteristic “sad-eyed” look, often combined with tearing and profuse rhinorrhea. In severe instances, this results in chronic excoriation of the soft tissue between the anterior nares and upper lip (Fig. 14-1).
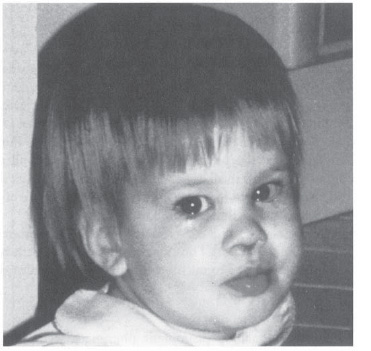
Figure 14-1 Child with severe allergy to corn. Note the rhinorrhea, nasal crusting, and teary-eyed appearance.
Eyes
Although the eyes are not truly the province of the otolaryngologist, the astute clinician observes the patient’s eyes, not only for the signs described previously but also for conjunctival or scleral injection, often indicative of the chronic rubbing that results from pruritus in these areas. Although not scientifically explained or documented, observations over many years by at least one of the authors validates Dr. Helen Krause’s observation (personal communication) that allergic children often have long, silky lashes.
Ears
The skin of the allergic child is often dry, scaly, or excoriated, and this condition can involve the skin of the concha and external canal. Although controversy continues regarding the role of allergy in recurrent otitis media or chronic middle ear effusion, studies indicate that this factor cannot be ignored. McMahan et al.2 found that of 119 children undergoing tube insertion for otitis media with effusion, 93% had positive results on radioallergo-sorbent testing (RAST) for inhalants, foods, or both. Renfro3 found that skin test results were positive in all of a study group of children receiving a set of tubes for the second time or more.
Nose
The nasal membranes (like all mucosa of the upper aerodigestive tract) are afflicted with intense pruritus during an allergic flare, giving rise to the allergic salute, supratip crease, and other signs already described. Other characteristic nasal manifestations of allergy are sneezing, discharge of clear mucus, and congestion. At one time, the presence of nasal polyps was thought to be a definite indication of the presence of allergy. Polyps and allergy are no longer thought to be linked in all cases. However, allergic patients with polyps have clinically been observed to have a higher rate of recurrence of their nasal polyps when their allergy is untreated following surgery.
The presence of nasal mucosal edema, combined with hypersecretion, often results in stasis within the sinuses. Thus, allergic children frequendy have sinusitis; this is slower to resolve and recurs more rapidly than in nonallergic children.
Pharynx
Signs of allergy may include prominent pharyngeal lymphoid follicles, producing a “cobblestone” appearance, often with prominent lateral bands. Hypertrophic adenoids and tonsils have also been attributed to uncontrolled allergy, with resultant chronic postnasal drainage.4 Similar hypertrophy of lingual tonsillar tissue may result in a sensation of having a “lump in the throat,” chronic throat clearing, or even dysphagia.
Although recurrent episodes of pharyngitis cannot be directly attributed to the presence of allergy, there is little doubt that chronic mouth breathing (with resultant drying of the mucous membranes and loss of the cleansing function of the nasal mucosa) and postnasal drainage provide a fertile field for the microorganisms to which children are frequently exposed.
Larynx
Recurrent or chronic hoarseness may suggest the presence of allergy and may be related to chronic throat clearing or episodes of allergic edema of the vocal folds.
FAMILY HISTORY AND ENVIRONMENTAL EXPOSURE
There is little doubt that a predisposition to the development of allergy is an inherited characteristic. The presence of atopy in parents and siblings should alert the physician to possible allergy in the patient. Although exact figures vary, it is generally accepted that a child with one allergic parent has roughly one chance in three of being allergic, whereas if both parents are allergic, the chance increases to more than two in three.
For clinical allergy to develop, repeated exposures to the allergens must occur, so that the formation of antigen-specific immunoglobulin E (IgE) is eventually triggered. Most allergy in children below the age of 2 years is caused by food hypersensitivity. Inhalant allergy becomes a significant factor after this age, and the earliest incriminated antigens are those to which the child is exposed: dust mite, mold, and animal danders. By about the age of 6 years, pollens are also significant offenders. Although in adults it is often necessary to employ several antigens when testing for inhalant allergy, the number may be less in children through a judicious history that focuses on exposure and circumstances under which symptoms are noted.
ADJUNCTIVE TESTS
An increase in the eosinophil fraction of leukocytes in a differential count should suggest the presence of allergy (although other disease states, such as infection with intestinal parasites, may also cause eosinophilia). More specific is the finding of eosinophils in an eosin-methylene blue-stained smear of nasal secretions. The exact details of specimen collection, staining, and interpretation are beyond the scope of this work and are described elsewhere.5 Although the finding of eosinophils (indicating allergy) or neutrophils (indicating an infectious component) in nasal secretions constitutes a respected means of confirming a clinical diagnosis, this test is not entirely accurate. For example, long-term topical application of corticosteroids to the nasal mucosa has been shown to diminish the number of nasal eosinophils.6 In addition, sampling techniques are highly variable (from having the patient blow the nose into waxed paper to the use of a plastic blunt curette to obtain nasal scrapings), and the experience of the person preparing and examining the slides significantly impacts the accuracy of the test results.
Another adjunctive test that has traditionally been employed in the diagnosis of allergic rhinosinusitis is examination of sinus radiographs. It is now accepted that conventional sinus x-ray films are of little benefit in confirming disease in the ethmoid sinuses, and that computed tomography (CT) scan of the sinuses is required for accurate diagnosis. To investigate antral disease, either an open-mouth, upright Waters view of the sinuses or the use of A-mode ultrasound scans may be helpful, as may be transillumination.7
TREATMENT BASED ON A PRESUMPTIVE DIAGNOSIS OF ALLERGY
The diagnosis of upper respiratory inhalant allergy is made by history. Physical examination confirms the manifestations. After these steps, specific testing may be performed to determine the offending antigens with certainty. However, a positive allergy test result without historical verification of symptoms likely produced by that antigen does not establish a diagnosis of “allergy” or justify treatment.
It is important for the clinician to realize that effective clinical management may be instituted based solely on a presumptive diagnosis of allergy made through history and physical examination alone. Thus, it is unnecessary to await the results of testing to afford some degree of relief to the child (and parents). In some instances, these measures are sufficiently successful to warrant deferring specific allergy testing.
Environmental Control
Although a great deal of upper respiratory allergy in very young children (especially below the age of 2 years) arises from food hypersensitivity, inhalant allergy in infants and young children in most cases is sensitization that develops to allergens found in the home environment, to which they are most frequently exposed: dust mite, molds, and animal danders.
Dust mite is an acarid that thrives in a warm, moist environment and feeds on human skin scales. Its antigen is found in the dung balls deposited by the organisms. The most common sites for dust mite exposure in children are stuffed animals and toys, bedding, upholstered furniture, and rugs. Several measures are available for diminishing dust mite exposure (Table 14-1), and parents should be urged to employ them as much as possible.8 Because this antigen is so commonly involved, dust mite avoidance measures are merited on an empiric basis in the management of children suspected of upper respiratory inhalant allergy, even before specific testing has been performed.
Molds are a frequent indoor antigen. Their growth requirements are similar to those for dust mite, and control of relative humidity in the home is helpful. It is often problematic to keep the indoor relative humidity above 40% (to combat the harmful effects of dry air on respiratory mucosa), yet below 50% (to minimize dust mite and mold growth). The purchase of a hygrometer or the use of a central humidifier with a humidistat is recommended. In addition to humidity control and avoidance of reservoirs such as houseplants, mold elimination should focus on treating visibly moldy surfaces. Commercially prepared “mildew sprays” are available, but a solution of household bleach (one part of bleach in ten parts of water) sprayed or wiped onto affected surfaces is also an effective treatment for mold and mildew.
1. Eliminate mite reservoirs. A. Encase mattress and pillows with barrier material. B. Wash all bedding weekly in hot water (140°F). C. Tumble stuffed animals in dryer weekly on hot cycle. D. Store stuffed animals in “hammock” over bed. E. Eliminate or minimize carpets and draperies in bedroom. 2. Utilize filtration devices and minimize visible dust. A. Use electrostatic or high-efficiency particulate air (HEPA) filters. B. Clean filters regularly or (if using conventional filters) change monthly. C. Dust regularly (patient should not do the dusting), using treated cloth to avoid spreading dust. 3. Reduce indoor humidity (<50%). A. Install air conditioner, dehumidifier. B. Eliminate or minimize houseplants. C. Ventilate home. 4. Use acaricides (e.g., benzyl benzoate) and antigen-denaturing agents (e.g., tannic acid). |
Animal danders are common sources of allergy in children, and cats are by far the most frequent and serious offenders. It appears that the allergen associated with cats is produced by the sebaceous glands in the cat skin (not just the salivary glands, as once thought). The allergen becomes airborne when skin scales are shed, and because the particles are quite small (2 to 4 μm), they remain airborne for prolonged periods. Even removing the cat (a suggestion that is usually met with significant resistance) does not solve the problem, as dander may continue to be present in the environment for 3 to 4 months afterward. Nevertheless, several measures may be instituted that will alleviate some of the symptoms suffered by children allergic to their beloved cat (Table 14-2).7
Pharmacotherapy
In addition to avoidance of known provoking factors, the treatment of suspected allergic rhinitis in children involves the administration of appropriate pharmacotherapeutic agents. Although these should be administered in an appropriate stepwise fashion, in the same manner as in the treatment of adults,9 certain factors unique to the treatment of children must be considered.
1. Limit exposure to the cat. A. Remove (when possible), or B. Eliminate from indoor access, or C. Eliminate from bedrooms. 2. Limit reservoirs (carpets, draperies, upholstered furniture). A. Eliminate carpets and draperies, or B. Frequently clean reservoirs, using HEPA vacuum, and C. Use efficient air filtration system (HEPA, electrostatic). 3. Minimize shed antigen and its effect. A. Wash the cat weekly.* B. Administer acepromazine to cat.* C. Apply Allerpet to cat.* D. Apply tannic acid to carpet (to neutralize antigen). *The efficacy of these measures has been questioned.24 |



