FIGURE 13.1 Simulated view of the vitreous during pars plana vitrectomy. The anterior vitreous is represented by lightly frosted cellophane tape. The retinal surface is represented by alphabets printed on a sheet of reddish-pink paper. A: With conventional wide-angle viewing systems (e.g., BIOM), illumination is separated from the surgeon’s view through the operating microscope. In the image below, the cellophane tape is barely visible overlying the alphabets. B: With endoscopy, illumination and the surgeon’s view are coaxial. In the image below, the same frosted tape is now almost opaque and highly visible, completely obscuring the underlying alphabets.
The anatomical perspective of the endoscope is unique. Conventional contact and noncontact viewing systems enable visualization of posterior segment structures through a bird’s-eye or face-on view through the pupil, with the most anteriorly visible structure being the vitreous base and occasionally the pars plana. Even with deep scleral indentation, anatomical structures anterior to that, that is, the pars plicata, ciliary body, lens equator, and posterior iris surface, are almost impossible to directly visualize and manipulate surgically. As ophthalmologists, the bird’s-eye view is the anatomical perspective we are most familiar and comfortable with based upon our experience of examining with the direct and indirect ophthalmoscopes. In contrast, the endoscope provides an unfamiliar side-on perspective relative to the patient’s visual axis. Through a pars plana sclerotomy, the vitreous base, pars plana, pars plicata, ciliary body, posterior lens surface, and retroiridial surface can be directly visualized without distortion from spherical aberration at the edge of a lens or deep scleral indentation (Fig. 13.2). This is advantageous in pediatric vitreoretinopathies in which adequate dissection of fibrovascular membranes involving the aforementioned structures can be the difference between surgical success and failure.
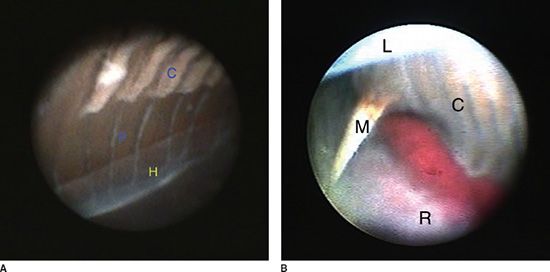
FIGURE 13.2 Intraoperative view through a 20-gauge endoscope. A: This is a child with aphakic glaucoma and rhegmatogenous RD. Normal anterior anatomical structures are clearly visualized. C, ciliary processes; P, pars plana; H, hyaloid (anterior hyaloid face). Note that the anterior hyaloid face is seen very clearly, due to the use of reflected rather than transmitted light. B: This is a neonate with stage 4B ROP. Anterior TRD is present. There is a much smaller space than normal for safe sclerotomy placement without lacerating the lens or retina due to an immature pars plana and anterior TRD. L, lens; M, MVR blade (20-gauge); C, ciliary processes; R, retina.
The unique anatomical perspective of the endoscope comes into its own, when an unhindered direct view under an immobile opaque tissue plane is required. For instance, in TRD in ROP or FEVR, the surgeon can alternate the position of the endoscope between visualizing above and below opaque fibrovascular membranes. Instead of relying on indirect clues, direct visualization of otherwise inaccessible safe preretinal dissection planes is possible, reducing the risk of iatrogenic retinal break formation. Minimizing the risk of complications is critical for surgical success in these zero error tolerance eyes. In stage 5 ROP, unlike rhegmatogenous RD or diabetic TRD in adults, an iatrogenic retinal break has been shown to lead to 100% failure in a series of six eyes (14).
There are several key aspects to the learning curve of endoscopic vitrectomy. Firstly, the surgeon’s view is derived from a video feed projected onto a monitor, rather than through the eyepieces of the microscope. This is a two-dimensional image, necessitating the greater use of nonstereoscopic clues such as shadows and inferring object distance by recognizing the size of anatomical landmarks relative to the known instrument gauge. It is noteworthy that intraocular shadows formed with an endoscope provides a different perspective from conventional viewing systems, due to the differing angle of reflected light captured, that is, coaxial versus noncoaxial illumination, respectively. Secondly, the intraoperative view is derived from a live video feed to a monitor, dissociated from the surgeon’s manipulation of surgical instruments. This requires some relearning of hand-to-eye coordination and feedback. Thirdly, the advantage of being able to resolve detail down to at least 20 μm equates to a highly magnified surgical perspective. It is essential that greater care is taken to maintain awareness of relative instrument positions within the narrow FOV to avoid inadvertent retina or lens touch. Fourthly, the endoscope adds rotation to the x-, y-, and z-axes of movement of conventional viewing systems. Fifthly, there is a need for regular adjustment of illumination levels. The optimum luminosity required to illuminate anatomical structures can vary significantly depending on the distance from the endoscope. The closer the endoscope is to the object of interest, the less light is required to avoid whiteout. This is the result of the narrower dynamic range of a digital image capture system such as the endoscope, relative to the human eye, predisposing to loss of some detail in the high or low extremes of illumination. Taking these factors into account, the initial experience with the endoscope is unfamiliar and can be disorientating. In the author’s experience, the use of a wet lab can be very useful for accelerating the familiarization process. The additional surgical time that is initially required is time well invested, as the ability to directly visualize surgical planes in complex surgical scenarios pays dividends in terms of reduced complications and improved clinical outcomes.
Clinical Application
In 1981, the first endoscopy-assisted vitreous surgery was described (15). In adults, there is good evidence for its use in rhegmatogenous (16) and TRD (17), PVR (18), endophthalmitis (19,20), penetrating eye injury (21
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


