FIGURE 11.1 A: SD-OCT image of the foveal center of a 46-week-old (corrected age) male infant born with a birth weight of 1,250 g and 31 weeks of gestation. The layers marked in blue denote the IRLs and comprise the nerve fiber layer, GCL, IPL, and INL. As a general rule, the nuclear layers appear hyporeflective compared to the plexiform layers. The layers marked in red denote the outer retinal layers and include the outer plexiform, the outer nuclear, the external limiting membrane, and the PRLs (inner segment and outer segment) and the retinal pigment layers. B: SD-OCT image of the foveal center of a healthy adult shows IRLs appear more centrifugally located than in (A), with condensation into a single hyperreflective band at the foveal center. The outer retinal layers are thicker at the foveal center, with further differentiation and increased thickness in the PRLs.
The foveal center of a healthy adult is shown alongside (Fig. 11.1B) and shows that with increasing age, the IRLs show a centrifugal location and condensation into a single hyperreflective band at the foveal center. The outer retinal layers on the other hand are much thicker at the foveal center in an adult with further differentiation and increased thickness in the PRLs.
Retinopathy of Prematurity Imaging on SD-OCT
The current gold standard for retinopathy of prematurity (ROP) diagnosis is clinical examination performed using the indirect ophthalmoscope by a trained ROP specialist. Wide-field digital retinal imaging of infants for ROP screening with the Retcam (Clarity MSI, CA, USA) is gaining popularity. OCT imaging in ROP in the current scenario is an adjunctive imaging technique that allows better understanding of the clinicopathologic aspects of the disease and has not yet become mainstream for its management. However, some recent reports suggest that SD-OCT is likely to play a major role in the near future.
In stage 4A, in which the macula appears attached, anatomic macular abnormalities not immediately apparent ophthalmoscopically, are detected on OCT and may explain the variability in visual outcome after lenssparing vitrectomy (8). A subclinical detachment of the macula detected on OCT would potentially convert the diagnosis from stage 4A to stage 4B, which would affect the visual prognosis and outcome of surgery. As a corollary, SD-OCT imaging may be used to obtain the macular status following stage 4B surgery to predict the outcome and visual improvement. With incomplete posterior hyaloid removal being the norm in ROP vitrectomy, OCT may be used as a quantifiable and measurable parameter to record the foveomacular attachment following surgery.
Recently, the advantage of SD-OCT in the management of cases of advanced ROP has been highlighted by the detection of features such as preretinal structures, retinoschisis, and retinal detachment that were not identified on standard examination (9).
We reported foveal disruptive changes in the macula, resembling adult cystoid macular edema in a subgroup of ROP infants (5). These changes were observed in clinically normal-looking foveas and were seen between the ages of 35 and 43 weeks postmenstrual age in cases of type 2 ROP, not requiring treatment. Interestingly, these foveal changes resolved spontaneously by 3 months postmenstrual age.
The foveal changes were divided into two categories based on their appearance. Pattern A: The central foveal change had a dome-shaped elevation resembling cystoid macular edema of the adult. The intraretinal cystoid spaces had highly reflective intervening vertical septa between the roof and the floor of the dome with complete disruption of the foveal depression in all cases and were accompanied by a marked increase in central foveal thickness (Fig. 11.2A). Pattern B: This type of central foveal change had features of multiple, confluent, or near confluent vacuolated optically empty hyporeflective spaces within the layers of the retina with a smaller number of septa or none at all. There was a preservation of the foveal depression and a moderate increase in the central foveal thickness (Fig. 11.2B).
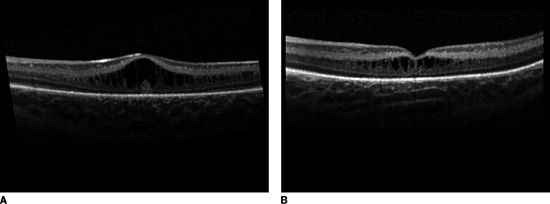
FIGURE 11.2 A: SD-OCT image of the foveal center of an infant with type 2 ROP and pattern A changes. Note the dome-shaped elevation resembling cystoid macular edema of the adult. Note the highly reflective intervening vertical septa of the intraretinal cystoid spaces between the roof and the floor of the dome with complete disruption of the foveal depression. There is significant increase in central foveal thickness. B: SD-OCT image of the foveal center of an infant with type 2 ROP with pattern B changes. Note the multiple, confluent, or near confluent vacuolated optically empty hyporeflective spaces within the layers of the retina with a smaller number of septa, preservation of the foveal depression, and a moderate increase in the central foveal thickness.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


