CHAPTER 11
Allergic Emergencies
The practice of office allergy has been compared with flying: hours of calm interspersed with occasional moments of stark terror. Those engaging in this practice must be constantly mindful that they are injecting patients with an antigen that may at any time potentially precipitate a life-threatening anaphylactic reaction. Obviously, the preferred approach is the prevention of such an emergency situation, and this chapter outlines steps aimed at just such a purpose.
Because bad things sometimes happen to good people, however, despite our best efforts, the appropriate management of an allergic emergency is also discussed. In the same fashion as a flight attendant calling your attention to the emergency procedure card located in the airplane seat pocket, we suggest you read this information carefully and hope you never need to use it.
PREVENTION OF ALLERGIC EMERGENCIES
Although it is mandatory that every health care provider who deals with allergy immunotherapy be well versed in the management of allergic emergencies, it is much better to avoid the occurrence of such crises altogether. Thus, it is worthwhile to devote some attention to measures that minimize the risk for anaphylaxis associated with allergy immunotherapy. Happily, the authors can attest to the effectiveness of these safeguards in their own practice of otolaryngic allergy.
Initial Testing Methods
The first important measure is the use of quantitative testing methods as a basis for immunotherapy. With intradermal dilutional testing (IDT), skin testing is begun at an anticipated nonreactive antigen dilution, and concentrations are advanced in fivefold steps until reactivity is observed and confirmed. This methodology immediately identifies the threshold of reactivity for each antigen to which the patient is sensitive, and allows the practitioner to avoid the introduction through testing or treatment of excessive amounts of that antigen.
Testing by in vitro methods, such as radioallergosorbent testing (RAST) or enzyme-linked immunosorbent assay (ELISA), not only provides quantitative information in a fashion similar to testing with IDT, but also avoids altogether the introduction of antigen into the patient’s system for testing purposes. With the diagnostic information provided by a quantitative in vitro assay, it is possible to know the degree of sensitivity of patients to any antigen long before a therapeutic injection is administered. In vitro tests are always safer than skin tests.
In either case, the immunotherapy treatment mixture formulated from IDT or in vitro tests can be adjusted so that every antigen is initially administered at the threshold concentration of reactivity. Antigens to which the patient is highly sensitive are placed into the mix in very dilute concentrations, whereas those to which the patient has only a limited degree of sensitivity can be introduced at stronger concentrations, providing treatment that is both efficient and safe.
Vial Testing
The final test to ensure safety is the initial in vivo test of the treatment vial. If no errors in compounding have occurred, this may be unnecessary in the case of IDT-based therapy, as testing and treatment vials have come from identical antigen sources in the stock vials. However, vial testing remains an excellent “fail-safe” measure to avoid any possible reactions resulting from errors in compounding the treatment vial. In vitro-based therapy must always include a vial test, as it is not certain that the antigens in the treatment vial are anti-genically the same as those used in the testing laboratory. Details of the vial test concept are presented in Chapter 10.
When a new stock vial of an antigen is obtained, even though it comes from the same manufacturer that provided the previous vial, it may not have the same antigenic potency as the one it is replacing. In this situation, vial tests of new treatment mixes made after such a change are a useful safety measure. As a practical matter, however, it is not always necessary to perform such vial testing if the antigen manufacturer is the same, and their quality control is good. On the other hand, if antigen is obtained from a new manufacturer, vial tests or even parallel IDT determinations using the old and new material may be necessary to avoid unnecessary reactions. Parallel IDT test comparison is always the best practice when switching from a weight/volume (w/v) antigen to a standardized antigen extract.
Recognition of Potential Hazards
Some antigens are known to present a significant potential for severe systemic reactions and should be used in skin tests with caution. The generally recognized examples of cottonseed, flaxseed, castor bean, and peanut will probably never concern the novice allergist, and if it is necessary to test for these, in vitro is a safe choice. Among the common inhalant antigens, grasses are recognized as being the most antigenically potent material, milligram for milligram, of any in the allergist’s armamentarium. In some patients, dust mite, cat, or cockroach extracts may also be very potent. Skin testing for any antigen while it is in season and/or in an individual whose history suggests a high degree of sensitivity should never be begun at a level more concentrated than the #6 (1:312,500 w/v) dilution.
Some patients are recognized as “brittle,” or highly sensitive, with a high potential for reactions to skin testing or injections. The prime examples of such high-risk patients are those with asthma.1 Others in this category include patients with urticaria, those with a history of prior severe reactions to allergy skin testing or injections, and patients suspected of having sensitivities to a great many allergens. These patients should be tested by in vitro means when possible, and if skin testing is required, they should have tests administered beginning at a very low concentration (usually #6 IDT dilution). Furthermore, it may be wise to limit the number of antigens tested for at any one sitting, to avoid a cumulative effect of numerous positive reactions in possibly producing a systemic reaction. A common error is testing for numerous antigens in the same or cross-reacting families, which effectively administers a higher dose of that antigen. This is most important when skin testing grasses. In most areas, it is sufficient to test with only Bermuda and Bahia grasses and with one Pooid grass, such as Timothy or Fescue. Placing additional wheals at higher concentrations after the confirming wheal has occurred is another way in which an unacceptable antigen load may be administered during testing. As a practical matter, if IDT is correctly performed (including proper antigen selection and not progressing past a confirming wheal), a reaction is unlikely to occur. Unless individual circumstances dictate otherwise, however, testing should probably be limited to 12 to 15 antigens per sitting. Finally, testing personnel should be trained to stop testing when they observe an unusual number of large wheals developing during a test session.
Reactions are more likely to occur during advancement immunotherapy than during skin testing, and this risk is heightened when the antigens in question are “in season.”2,3
Dose Advancement
The first injection from any new treatment vial should ideally be administered in the physician’s office, because there is potential for an abrupt effective dose increase with a freshly made vial.3 Thereafter, dose advancement should be modified as circumstances change. One can never completely place a patient on a routine schedule for dose advancement without consideration of changes in allergic load, complicating infections, and similar modifying factors. The dose should be advanced to the maximum tolerated dose, with the realization that local (and systemic) reactions indicate the need for modification of dose schedules. If continued reactions occur despite appropriate dose adjustments, it is often best to discard the treatment vial in use and begin again. The effort involved in remaking a vial is small, whereas the costs of dealing with anaphylaxis are large and not simply measured in units of time and money.
Human Errors
The possibility for error in the allergy office exists at every step, from testing to vial formulation to administration of immunotherapy. Measures to avoid allergic reactions begin with adequate training of the person responsible for testing, so that proper technique and procedure are followed. It is a good idea to have the physician or another member of the allergy team double-check the determination of end points and the mathematics of vial preparation from the data obtained. It must be emphasized that the person preparing vials should do so in an environment totally free from interruptions and distractions, to minimize lapses in concentration and possible compounding errors. During mixing, labels should be preattached to mixing vials, and mixing technique should be checked and double-checked. If ever the mixing process is interrupted, or the person preparing a vial becomes uncertain of a vial’s contents, that vial should be discarded, and a new one made.
If properly performed, IDT is a safe means of skin testing for inhalant allergy. However, if additional wheals are placed beyond the “confirming wheal,” overdosing is possible. Correct interpretation of the test results is also necessary to assess accurately the antigen concentration that will be included in the initial treatment vial. After end points have been determined (either from IDT or in vitro), accurate calculations and mixing are necessary to prepare the treatment vial, and errors in this process can have disastrous results. One of the most common (and potentially catastrophic) errors is a misplaced decimal point, either in calculations of dose or in drawing up the appropriate volume for injection. This is particularly a problem if injections are given in an office that is relatively unfamiliar with allergy treatment, and is used to giving 0.5 or 1.0 mL shots. Reactions have ensued after a dose of 0.05 mL has been confused with one of 0.5 mL, providing a 10-fold overdose of antigen.
The administration of injections from the treatment vial requires that the vial of the correct patient be chosen from all the available vials (Fig. 11-1) and that the proper dose be given. The opportunities for disastrous consequences of a mistake are obvious. When an injection is administered, the patient’s identity should be checked against the vial label, and the dose administered should be carefully scrutinized. To avoid any such misidentification, the authors advise that the treatment vial be shown to the patient, who is asked to confirm its identity (Fig. 11-2). Birth dates should also be used whenever two patients with similar or identical names are on treatment. Color-coded vials may be used when more than one patient in a family is on home treatment.

Figure 11-1 The correct patients vial must be carefully selected from all those available.
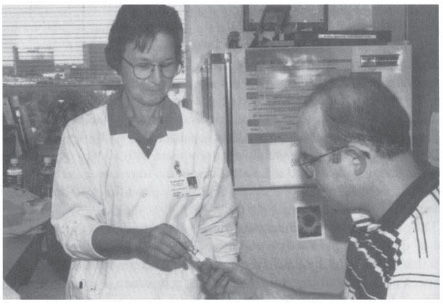
Figure 11-2 Both the person giving the injection and the patient should make sure that the proper treatment vial has been chosen.
In short, allergy testing and treatment present numerous opportunities for errors that can possibly result in anaphylaxis. The prevention of these errors requires constant and meticulous attention on the part of the allergy nurse or assistant.
NURSE’S NOTE
A number of points should be emphasized for safety:
1. When making an initial treatment vial, have a second person check the calculations, including the strengths of each antigen to be placed in the vial.
2. Carefully check the decimal point when drawing up a dose.
3. Have patients identify treatment vials as their own.
TYPES OF ALLERGIC REACTIONS 303
True allergic reactions may be immediate or delayed. These should be differentiated from nonallergic, vasovagal reactions, which are (fortunately) much more common than true allergic reactions. Both immediate and delayed reactions may be local or systemic. Local reactions are characterized by induration (wheal) surrounded by erythema (flare) (Fig. 11-3). The size of the wheal (not the flare) is the determining factor in altering subsequent immunotherapy doses.
Delayed allergic reactions may be either local or systemic, and the former are much more common than the latter. A significant delayed local reaction is characterized by an area of induration and redness greater than 30 mm in diameter (i.e., larger than a half-dollar coin) at the site of a previous injection. Delayed systemic reactions are generally manifested as an increase in the patient s usual allergic symptoms, but symptoms may also include urticaria, arthralgias, or constitutional symptoms involving almost any organ system.
Delayed allergic reactions are generally of the Gell and Coombs type III. They are most often seen in association with allergy to molds. These reactions typically occur from 6 to 36 hours after an injection (or skin test), and thus do not occur while the patient is in the office or has just had the injection or test. It is therefore important not only to educate patients about the possible occurrence of such reactions, but also to advise them regarding proper treatment measures. The treatment of a delayed local reaction generally requires only the administration of one or more doses of an antihistamine, sometimes augmented by application of ice to the reaction site followed by a topical steroid cream or ointment. However, it is important that these reactions be reported so that appropriate adjustment of the immunotherapy dose can be made if they occur regularly.
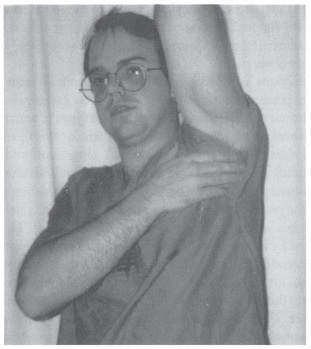
Figure 11-3 Large delayed local reaction, with central induration (wheal) and surrounding erythema (flare), indicating a need for dose adjustment.
Delayed general reactions are extremely uncommon. Treatment consists of the administration of antihistamines, augmented by systemic corticosteroids for a few days (such as a tapered-dose pack) if the severity of symptoms warrants. As with delayed local reactions, a decrease in dose to prevent a recurrence is prudent.
Acute arm reactions resulting in wheals that are less than 30 mm in diameter, and that produce no systemic symptoms, are frequently observed normal events, and indicate that an immunologically potent allergen dose has been administered. As desensitization progresses, these reactions typically become smaller, and may eventually vanish.
Acute local reactions with wheals larger than 30 mm display the same characteristics as delayed local reactions, except that they occur within an hour or less of the test or injection. They are treated in the same fashion: a systemic antihistamine (by mouth), local application of ice to the affected area followed by a steroid ointment or cream if necessary, and subsequent adjustment of the immunotherapy dose.
Vasovagal reactions, in which symptoms range from sweating and pallor to syncope, do not present the same potential for severe consequences as anaphylaxis. It is important to differentiate between these types of reaction rapidly and accurately, however, to avoid either undertreatment or overtreatment. Patients with vasovagal reactions typically complain of “feeling faint” and manifest both pallor and sweating (the classic “cold sweat”). Their pulse is slow. In vasovagal episodes, the blood pressure may be slightly low in the sitting position but is normal when the patient is placed in a recumbent position. These patients may lose consciousness, although generally for a minute or less. This event is frequently initiated by a brief episode of twitching or even tonic movements and must be differentiated from a true seizure. Patients undergoing vasovagal syncope do not lose bowel or bladder control, do not chew their tongues, and do not demonstrate the persistent or prolonged tonic or clonic motions that characterize a seizure. They usually awaken rapidly, with no sequelae.
The treatment of vasovagal reactions is recumbency, reassurance, and time. This is generally augmented by placing a cold cloth to the forehead and administering a whiff of an ammonia ampule. Although not a required therapeutic maneuver, oxygen administered by a mask is sometimes reassuring. The most important part of managing a vasovagal reaction is differentiating it from anaphylaxis.
Anaphylactic reactions are of the immediate type and represent a Gell and Coombs type I event. Their importance lies in their potential for rapid progression to an ultimately fatal outcome. Therefore, it is important to recognize their characteristic signs and symptoms (Table 11-1). In anaphylaxis, the organs richest in mast cells (respiratory tract, blood vessels, skin) are primarily affected. The onset of anaphylaxis is generally seen within 15 to 20 minutes of the allergic event and almost never begins after 45 to 60 minutes have passed.3,4
Signs and symptoms | Vasovagal reaction | Anaphylaxis |
|---|---|---|
Cardiovascular system | ||
Pulse | Slow | Rapid |
Blood pressure (recumbent) | Normal | Low |
Skin | ||
Color | Pale | Red (cyanosis late) |
No rash | Angioedema-urticaria | |
Temperature | Cool | Warm |
Perspiration | Profuse | Little |
Respiratory system | ||
Itching | None | Itching mucous membranes |
Secretions | No change | Increased |
Nasal congestion | No change | Increased |
Hoarseness | None | Progressive |
Cough, wheezing | No change | Present |
Dyspnea | None | Progressive (retractions late) |
Central nervous system | ||
Loss of consciousness | Transient | Late |
Apprehension | Anxious | Angor animi |
Gastrointestinal system | ||
Nausea, diarrhea | Generally absent | Present late |
Genitourinary system | ||
Urinary urgency | Generally absent | Present late |
Uterine cramps | Generally absent | Present late |



