Nose and Paranasal Sinuses
Anatomy and physiology
The nose
Anatomy
It is useful to consider the anatomy of the nose by dividing it into:
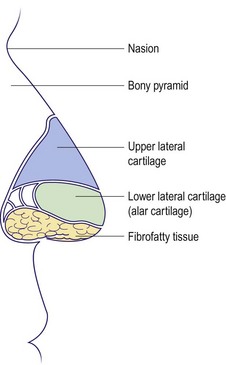
External nose
The upper third of the external nose (Fig. 2.1) is bony, consisting of nasal bones which connect with the nasion at the forehead. The inferior two-thirds are cartilaginous, consisting of the upper lateral and lower lateral (alar) cartilages. The tip laterally contains resilient but pliable fibrocartilage. This allows maintenance of nasal shape after minor trauma. The skin over the cartilaginous portion is closely adherent and contains multiple sebaceous glands; these latter structures may hypertrophy to form a rhinophyma.
Nasal cavity
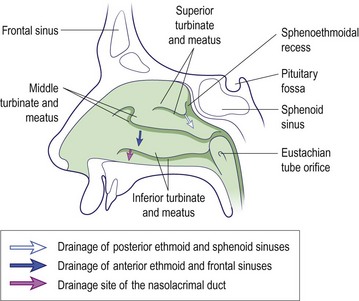
The nasal cavity stretches from the vestibule anteriorly to the nasopharynx posteriorly and is divided by a midline osteocartilaginous septum. The lateral wall of the cavity supports a series of ridges called turbinates (Fig. 2.2). These structures are lined by ciliated columnar epithelium and contain erectile tissue. The paranasal sinuses – maxillary, frontal, ethmoid and sphenoid – drain into the nasal cavity around the middle turbinate.
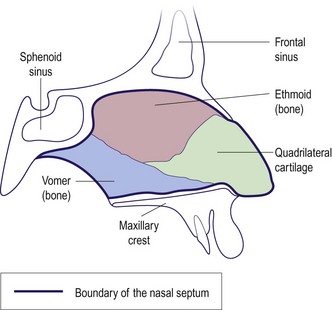
The nasal septum comprises bony and cartilaginous elements. Inferiorly, it is inserted into a groove in the maxillary crest (Fig. 2.3). It is lined with mucoperichondrium and mucoperiosteum over the cartilage and bone, respectively. The nasal septum is rarely straight; marked displacement causes nasal airway blockage and an external cosmetic deformity.
The paranasal sinuses
Anatomy
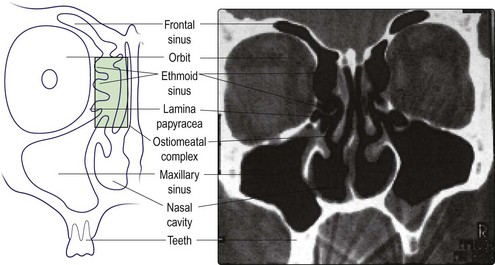
The paranasal sinuses (Fig. 2.4) are really extensions of the nasal cavity as air-filled spaces into the skull bones. Although paired anatomically, from a pathophysiological view they should be grouped as anterior and posterior. The frontal, anterior ethmoidal and maxillary sinuses (anterior group) drain into the middle meatus, and the posterior ethmoidal and sphenoid (posterior group) drain into the superior meatus and sphenoethmoidal recess. The crucial drainage area of the anterior group of paranasal sinuses is called the ostiomeatal complex (Fig. 2.4). The nasolacrimal duct opens into the anterior part of the inferior meatus.
Physiology
Anatomy and physiology
 The nose is structurally composed of bone and cartilage.
The nose is structurally composed of bone and cartilage.
 Both the external and internal carotid arteries provide the rich vascular supply of the nasal mucosa.
Both the external and internal carotid arteries provide the rich vascular supply of the nasal mucosa.
 The nose has an important protective role in filtering, humidifying and warming inspired air.
The nose has an important protective role in filtering, humidifying and warming inspired air.
 The nose, as part of the respiratory tract, is prone to acute infection and allergic phenomena.
The nose, as part of the respiratory tract, is prone to acute infection and allergic phenomena.
 Since the paranasal sinuses drain via the nose, sinus disease is frequently due to primary problems in the nose.
Since the paranasal sinuses drain via the nose, sinus disease is frequently due to primary problems in the nose.
Symptoms, signs and investigations
Symptoms
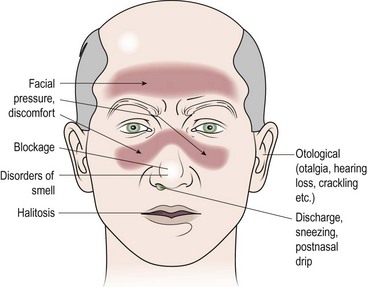
It is vital to establish the precise complaint of the patient; therefore, a full history is mandatory (Fig. 2.5).
Nasal obstruction
Nasal obstruction is the most common symptom, and may be due to anatomical abnormalities, disorders of the mucous membrane lining or stimulation of the autonomic nervous system (Table 2.1). An allergic aetiology is likely where the symptoms manifest after contact with allergens such as grass pollen, feathers or animal dander. Viral infections, e.g. acute coryza and influenza, cause severe nasal obstruction but generally resolve rapidly over days. An overactivity of the parasympathetic as compared to the sympathetic nerve supply will cause dilatation of the vascular tree and hence engorgement. This is particularly noted by some patients in stress situations and with alterations in ambient temperature and humidity. Neoplasia produces a progressive unilateral obstruction.
Table 2.1 Causes of nasal obstruction
| Variety | Associated conditions |
|---|---|
| Anatomical | Septal deflection |
| Adenoidal hypertrophy | |
| Neoplasia | |
| Choanal atresia | |
| Disorders of nasal lining | Allergic and infective rhinitis |
| Nasal polyps | |
| Autonomic nervous system | Vasomotor rhinitis |
Nasal discharge
The specific character of the discharge is helpful in deciding aetiology (Table 2.2). Many patients describe this as ‘catarrh’. However, if it produces a runny nose, the discharge should be described as rhinorrhoea and the term ‘catarrh’ (or postnasal drip) reserved for nasal discharge passing backwards into the nasopharynx. Epistaxis is nasal haemorrhage and is most commonly due to spontaneous rupture of a blood vessel in the nasal mucous membrane. However, it is vital to exclude any bleeding disorders and neoplasms. If the discharge is offensive, it may indicate a bacterial infection, the presence of a foreign body or neoplasia.
Table 2.2 Nasal discharge: its characteristics and significance
| Character of discharge | Associated conditions |
|---|---|
| Watery/mucoid | Allergic, infective (viral) and vasomotor rhinitis |
| Cerebrospinal fluid leak | |
| Mucopurulent | Infective (bacterial) rhinitis and sinusitis |
| Foreign body | |
| Serosanguineous | Neoplasia |
| Bloody | Trauma, neoplasia, bleeding diathesis |
Signs
External
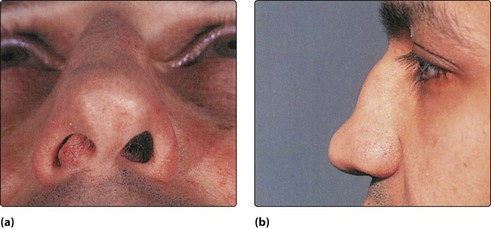
Certain cosmetic deformities such as angulation of the bony nasal pyramid or a nasal hump may be obvious. A saddle deformity due to previous injury or infection is readily identified. It is not unusual to find the septal cartilage dislocated into the nasal vestibule (Fig. 2.6).
Investigations
Allergy testing
The simplest allergy test is a skin-prick performed on the volar aspect of the forearm. A wide variety of allergens may be tested, but the common ones include pollens, animal dander, and house and dust mite. Controls such as a negative control (saline) and positive control (histamine) should be employed. A positive response produces a wheal and flare (in about 20 minutes) which can be graded. A negative response does not exclude allergy, and a positive response is not absolute proof that the specific allergen is causing symptoms (Fig. 2.8). The radioallergosorbent test (RAST) measures allergen-specific serum immunoglobulin E, but is expensive.
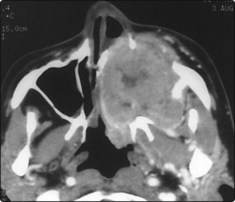
Radiology
Plain X-rays of the sinuses have limited value. Computed tomography (CT) is the imaging of choice for the majority of nasal and sinus disease (Fig. 2.9). Soft tissue abnormalities and tumours require magnetic resonance imaging (MRI) (Fig. 2.10).
Miscellaneous
Symptoms, signs and investigations
 Nasal obstruction is the most common symptom.
Nasal obstruction is the most common symptom.
 The characteristics of nasal discharge may be suggestive of particular disease.
The characteristics of nasal discharge may be suggestive of particular disease.
 Nasal pathology may, via the trigeminal nerve, give rise to referred head and neck pain.
Nasal pathology may, via the trigeminal nerve, give rise to referred head and neck pain.
 The internal nose is best examined using a rigid endoscope.
The internal nose is best examined using a rigid endoscope.
 Skin-prick tests for nasal allergy are recommended for investigating rhinitis.
Skin-prick tests for nasal allergy are recommended for investigating rhinitis.
 CT and MRI have replaced plain radiology in the detailed examination of the nose and paranasal sinuses.
CT and MRI have replaced plain radiology in the detailed examination of the nose and paranasal sinuses.
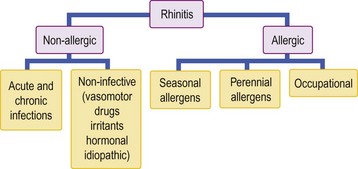
Allergic and vasomotor rhinitis
The term ‘rhinitis’ implies an inflammatory response of the lining membrane of the nose and may be intermittent or persistent. It is important to understand that such an event can occur as a consequence of both primary allergic and non-allergic mechanisms (Fig. 2.11). In allergic rhinitis, specific allergens are responsible for a type 1 hypersensitivity reaction, and the symptom complex may be subclassified as being predominantly seasonal or perennial. Non-allergic pathologies include viral and bacterial infections (pp. 38, 50), as well as autonomic nervous system abnormalities which can result in vasomotor rhinitis.
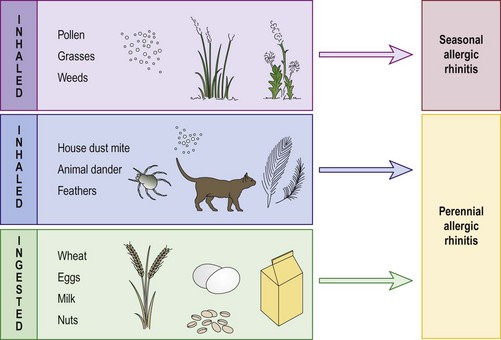
Allergic rhinitis
More than 20% of the population in Western Europe suffers to some degree from nasal manifestations of an antigen–antibody type 1 hypersensitivity reaction (Fig. 2.12). In seasonal allergic rhinitis (hay fever), the allergens are inhaled, e.g. grass, pollens, weeds and flowers. Animal dander, house dust mite and feathers are the principal allergens in perennial allergic rhinitis and have no seasonal variation. Rarely, ingested allergens are implicated in the perennial group, e.g. dairy products and wheat. This would normally occur in conjunction with gastrointestinal symptoms.
Clinical features
The clinical features of allergic rhinitis include the classic triad of:
 nasal obstruction due to mucosal vasodilatation and oedema
nasal obstruction due to mucosal vasodilatation and oedema
 rhinorrhoea (runny nose) due to enhanced activity of glandular elements
rhinorrhoea (runny nose) due to enhanced activity of glandular elements
Typically, the nasal mucosa has a boggy, oedematous appearance (Fig. 2.13); it is covered by a thin layer of watery secretion. Application of a vasoconstrictor produces marked mucosal shrinking with improvement in the nasal airway. Skin-prick tests should be interpreted only in relation to the history. Negative skin tests in the face of obvious allergens are not infrequent.
Management
 changing a feather pillow to foam
changing a feather pillow to foam
 washing the bedclothes twice weekly, as the antigen is heat sensitive
washing the bedclothes twice weekly, as the antigen is heat sensitive
 using a dust-proof cover over the mattress, duvet and pillows
using a dust-proof cover over the mattress, duvet and pillows
Rhinitis medicamentosa
Management
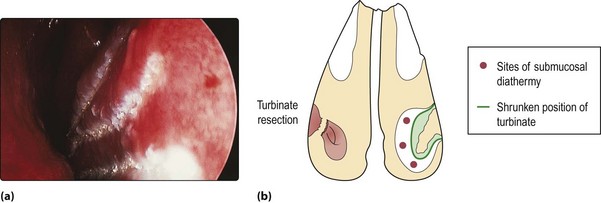
Treatment should be prophylactic, i.e. certain preparations should only be employed as ‘short, sharp’ therapies. Established rhinitis medicamentosa requires substitution of the offending drug by one containing a steroid, or use of a systemic decongestant. In severe cases, the mucosal swelling becomes irreversible. Such cases require surgical treatment, usually partial turbinate resection (Fig. 2.14).
Allergic and vasomotor rhinitis
 The most common perennial allergen is house dust mite.
The most common perennial allergen is house dust mite.
 Pollen is the most common seasonal allergen.
Pollen is the most common seasonal allergen.
 False-negative results on skin tests are not infrequent.
False-negative results on skin tests are not infrequent.
 Sinofacial congestion is common in allergic rhinitis.
Sinofacial congestion is common in allergic rhinitis.
 Rhinitis and asthma frequently coexist as part of the same disease process.
Rhinitis and asthma frequently coexist as part of the same disease process.
 The mainstay of treatment of allergic and vasomotor rhinitis is medical.
The mainstay of treatment of allergic and vasomotor rhinitis is medical.
 Topical nasal steroid preparations are valuable in reducing or abolishing the allergic reactions in many patients and can be prescribed long term.
Topical nasal steroid preparations are valuable in reducing or abolishing the allergic reactions in many patients and can be prescribed long term.
 Prolonged application of potent topical vasoconstrictors leads to rhinitis medicamentosa.
Prolonged application of potent topical vasoconstrictors leads to rhinitis medicamentosa.
Nasal polyps and foreign bodies
Nasal polyps
The cause of nasal polyps is not well understood, although they are common in patients with conditions such as asthma and cystic fibrosis (Table 2.3).
Table 2.3 Percentage prevalence of nasal polyps
| Normal population | 4% |
| Nasal allergy | 1.5% |
| Asthma | 7–15% |
| Aspirin sensitivity | 36–60% |
| Allergic fungal sinusitis | 80% |
| Cystic fibrosis | 27% |
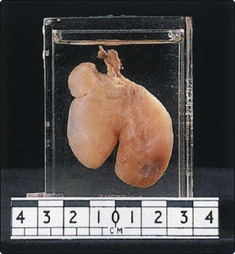
Nasal polyps are ‘bags’ of oedematous mucosa and most frequently arise from the ethmoid cells and prolapse into the nose via the middle meatus. They are nearly always bilateral. If allowed to grow they may present in the nasal vestibule (Fig. 2.15). The cardinal symptom is progressive nasal obstruction. Rhinorrhoea is frequent and occasionally a history of recurrent sinusitis due to ostial blockage is a feature. Hyposmia and anosmia are not uncommon and otological symptoms may occur.
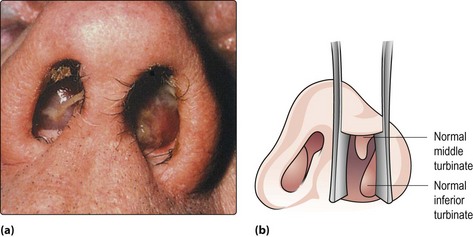
Fig. 2.15 (a) Bilateral nasal polyps presenting in the nasal vestibules. A polyp can easily be confused with a normal inferior turbinate (b), especially if the turbinate is hypertrophic. (See also Fig. 2.8, p. 33.)
Management
Small polyps respond well to topical nasal steroids. Large polyps are treated by a short course of systemic steroids followed by long-term use of topical steroids. Endoscopic ethmoidectomy is indicated for non-responsive and recurrent polyps. Recurrence rates may be reduced by long-term topical steroids, postsurgery. Any chronic sinus infection should be treated in conjunction with nasal polypectomy. Routine management strategies for the associated allergy or asthma should also be instituted (pp. 34–35).
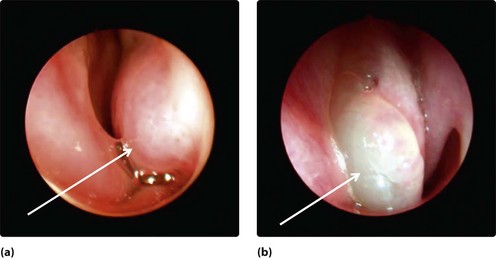
Antrochoanal polyp
The antrochoanal polyp is uncommon. It is usually unilateral and commences as oedematous lining in the maxillary sinus. This prolapses, usually via a posterior accessory ostium, into the nasal cavity and enlarges towards the posterior choana and nasopharynx. The patient, commonly a young adult, complains of unilateral nasal obstruction, which is worse on expiration due to the ball valve effect of the polyp in the posterior choana. If significantly large it may block both choanae and cause otological symptoms due to obstruction of the Eustachian tube (Fig. 2.16). Patients occasionally present so late that the polyp has enlarged behind the soft palate and hangs visibly in the oropharynx.
Neoplastic polyps
Neoplastic polyps (p. 110) are invariably unilateral and cause progressive symptoms: nasal obstruction, epiphora (blocking of the vasolacrimal duct), epistaxis and foul-smelling nasal discharge. They are frequently fleshy in appearance and bleed on palpation. Biopsy is mandatory.
Nasal foreign bodies
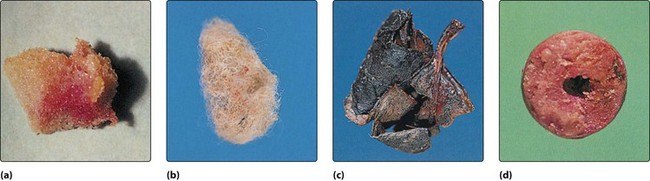
Young children (and on occasion, psychiatric cases) are the main patients who insert foreign bodies into the nose. The variety of foreign bodies is protean (Fig. 2.17), but readily available items such as foam rubber, peas and small stones are frequent. Inorganic objects may be in situ for long periods before producing symptoms. However, organic objects, such as paper, wool and vegetable material, produce a brisk mucosal reaction and hence rapid onset of symptoms (Fig. 2.18).
Clinical features
The child is usually calm, although prior clumsy attempts at removal may have caused distress. Usually, the parents provide a sound history which an older child frequently denies. The cardinal sign is a unilateral nasal discharge which is foul smelling if the foreign body has been present for any length of time (Fig. 2.18). Excoriation of the nasal vestibular skin and upper lip may be present. The foreign body frequently impacts in the lower part of the nose and on occasions simply rests in the nasal vestibule. Unless there is a marked infection, visualization is usually possible in good light by elevating the nasal tip gently with the thumb.