Purpose
To evaluate wound architectures of a clear corneal incision and the duration of stromal edema caused by intentional hydration in cataract surgery using 3-dimensional (3-D) cornea and anterior segment optical coherence tomography (OCT).
Design
Prospective, randomized study.
Methods
On 30 eyes of 23 patients, cataract surgery was performed through a clear corneal incision created with a 2.4-mm blade. After confirming the water tightness of the clear corneal incision at the end of surgery, 15 randomly selected eyes received stromal hydration, and the remaining 15 eyes did not. Using the 3-D cornea and anterior segment optical coherence tomography, wound architecture was assessed 1 day, 1 week, and 2 weeks after surgery.
Results
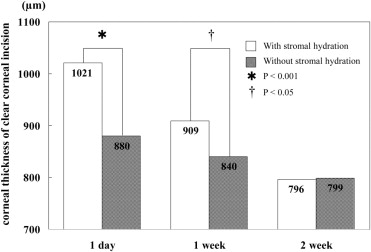
There was a statistically significant difference in corneal thickness at the clear corneal incision between eyes with and without stromal hydration 1 day and 1 week after surgery ( P < .001 and P < .05, Mann–Whitney U test), but not at 2 weeks after surgery. On day 1, gaping at the epithelial side was seen in 6.7% (2 eyes), gaping at the endothelial side in 30% (9 eyes), misalignment of the roof and floor of incision in 40% (12 eyes), and local detachment of Descemet membrane in 36.7% (11 eyes). These imperfections improved with time.
Conclusions
Using the 3-D cornea and anterior segment optical coherence tomography, detailed architectures of the clear corneal incision were investigated. It was found that the effect of stromal hydration lasted for at least 1 week after surgery.
A self-sealing clear corneal incision has been used widely in cataract surgery because of ease of construction and lack of bleeding. Surgeons typically check the wound integrity by inflating the anterior chamber with balanced salt solution and applying pressure with a Weck cell sponge (Eagle Laboratories, Rancho Cucamonga, California, USA) against the posterior lip of the incision. If apparent leakage exists, the surgeon often applies corneal stromal hydration to enhance wound sealing and to prevent the inflow of ocular surface fluid. Proper construction and secure closure of the incision, including application of stromal hydration, are of critical importance to obtain optimal outcomes after cataract surgery. However, there have been only a few reports that investigated the detailed structure of the clear corneal incision using optical coherence tomography (OCT), and it is not clear how long the effects of stromal hydration last.
We developed a 3-dimensional (3-D) corneal and anterior segment OCT based on swept-source OCT technology, which is a variation of Fourier-domain OCT. Because the measurement speed of swept-source 3-D corneal and anterior segment OCT is more than 10 times faster than that of time-domain OCT, it has high robustness against a sample motion and is capable of obtaining full 3-D images of ocular tissues. The 3-D corneal and anterior segment OCT can create any cross-sectional images of the anterior segment of the eye, and thus it provides more precise perpendicular scans of the incision than the conventional imaging methods. In this study, 3-D corneal and anterior segment OCT was used to evaluate the detailed structural characteristics of clear corneal incision, including the duration of stromal hydration.
Methods
A total of 30 eyes from 23 patients undergoing standard cataract surgery were evaluated. The procedure was performed under topical anesthesia by a same surgeon (T.O.) at Tsukuba University Hospital. The research followed the tenets of the Declaration of Helsinki, and written informed consent was obtained from each eligible participant. The mean age of the participants was 71.1 ± 13.5 years of age (mean ± standard deviation). Inclusion criteria included no history of ocular surgery, maximum pupil dilation of more than 7.0 mm at the preoperative examination, absence of biomicroscopic signs of pseudoexfoliation, normal fundus examination, and endothelial cell count of at least 2000 cells/mm 2 . Exclusion criteria were the presence of preexisting corneal disease and of glaucoma.
Phacoemulsification and intraocular lens implantation were performed as follows. A side-port incision was created with a 30-degree steel blade. An ophthalmic viscosurgical device was injected into the anterior chamber, and then the main clear corneal incision with a square wound configuration was made using a 2.4-mm steel blade. Phacoemulsification was performed using OZil (Alcon, Fort Worth, Texas, USA) torsional technology with an ultra-sleeve on an Infiniti phacoemulsification platform (Alcon). An intraocular lens (SN60WF; Alcon) was implanted using the D cartridge and Monarch injector. After the ophthalmic viscosurgical device was thoroughly washed out with an irrigation and aspiration unit, the anterior chamber was reformed with balanced salt solution through the paracentesis aiming for a slightly higher intraocular pressure. Intraocular pressure was checked digitally. At this stage, the wounds were checked for water tightness in all 30 eyes using a Weck cell sponge, and it was confirmed that all incisions had no leakage. Thereafter, corneal stromal hydration was applied in 15 randomly selected eyes by placing the tip of a 25-gauge cannula in the side walls of the incision and gently irrigating balanced salt solution into the stroma. This was performed at both edges of the incision. In the remaining 15 eyes, the wounds were not hydrated. The clear corneal incision was evaluated using the 3-D corneal and anterior segment OCT at 1 day, 1 week, and 2 week after surgery.
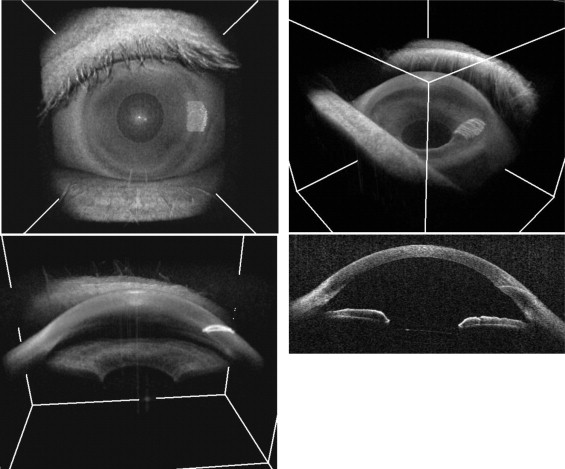
The 3-D corneal and anterior segment OCT was a custom prototype model built by the Computational Optics Group, University of Tsukuba, and the Tomey Corporation (Nagoya, Japan), which was based on optical frequency-domain imaging technology. The light source had a center wavelength of 1.3 μm, which enables greater penetration into the ocular tissue compared with the conventional 830 nm OCT. This system 3-dimensionally depicts the anatomic features of the anterior segment, such as cornea, scleral spur, angle recess, iris root, and filtering bleb. The measurement speed is 20 000 A-lines/second. The maximum measurement ranges were 16 × 16 mm in width and 6 mm in depth in tissue. The mean axial resolution within a 4-mm depth range was 11 μm in tissue. The 3-D corneal and anterior segment OCT provided 3-D tomography with the acquisition time of 3.3 seconds per volume for 256 × 256 × 1024 voxels. A typical 3-D scan comprises 256 horizontal cross-sections, each of which comprises 256 A-scans. This OCT system can produce 2-dimensional images by sectioning the 3-D image in any arbitrary direction ( Figure 1 ).
The measurement parameters of the clear corneal incision included the length and width of the clear corneal incision, the length between angle recess to the endothelial side of the clear corneal incision, and the length between the point that drops a perpendicular line from the angle recess to the corneal surface and the epithelial side of the clear corneal incision ( Figure 2 ).
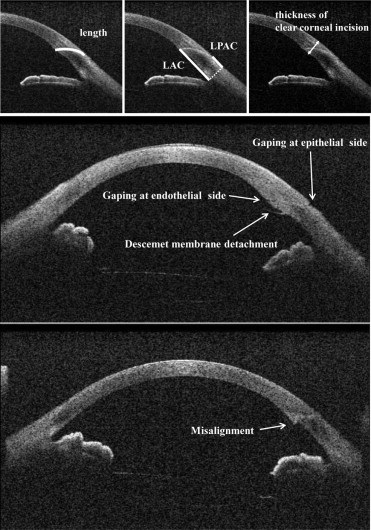
Five architectural features of the clear corneal incision were assessed according to the report by Calladine and Packard: gaping of the wound at the epithelial and endothelial side, misalignment on the roof and the floor of the incision at the endothelial side, local detachment of the Descemet membrane, and loss of adaptation along the stromal tunnel ( Figure 2 ).
Table 1 summarizes preoperative characteristics of patients and surgery time. There were no significant differences in the baseline parameters between the stromal hydration group and the nonstromal hydration group. The measurement values of 2 groups were compared using the Mann–Whitney U test. The 5 architectural features of the clear corneal incision were compared between 2 groups using the Fisher exact probability test. The intraocular pressure was compared in eyes with and without architectural features using the Mann–Whitney U test. Analyses were carried out using StatView software (SAS Institute, Cary, North Carolina, USA).
| With Stromal Hydration | Without Stromal Hydration | All | P Value | |
|---|---|---|---|---|
| Age (yrs) | 70.8 ± 12.3 | 71.4 ± 15.0 | 71.1 ± 13.5 | .740 |
| logMAR BCVA | 0.46 ± 0.23 | 0.42 ± 0.18 | 0.41 ± 0.23 | .659 |
| Surgery time (min) | 5.87 ± 1.30 | 5.93 ± 1.23 | 5.90 ± 1.24 | .848 |
| Preoperative IOP (mm Hg) | 12.6 ± 2.4 | 13.0 ± 2.3 | 12.8 ± 2.3 | .516 |
| Postoperative IOP (mm Hg) | ||||
| 1 day after surgery | 17.9 ± 3.2 | 18.7 ± 2.1 | 18.3 ± 2.7 | .390 |
| 1 wk after surgery | 13.3 ± 2.5 | 13.1 ± 2.0 | 13.2 ± 2.2 | .866 |
| 2 wks after surgery | 12.4 ± 1.9 | 13.2 ± 1.6 | 12.8 ± 1.8 | .075 |
| Nuclear color | 2.43 ± 0.46 | 2.47 ± 0.69 | 2.45 ± 0.58 | .983 |
| Preoperative cell count (/mm 2 ) | 2701 ± 210 | 2815 ± 243 | 2758 ± 231 | .191 |
Results
Corneal Thickness at Clear Corneal Incision
In eyes with stromal hydration, corneal thickness at the clear corneal incision was 1020.5 ± 98.0 μm, 908.9 ± 54.4 μm, and 795.7 ± 57.6 μm at 1 day, 1 week, and 2 weeks after surgery, respectively. In eyes without stromal hydration, corneal thickness at the clear corneal incision was 880.3 ± 79.6 μm, 840.3 ± 92.0 μm, and 799.3 ± 93.6 μm at 1 day, 1 week, and 2 week after surgery, respectively. A statistically significant difference was noted between the 2 groups at 1 day and 1 week after surgery ( P < .001 and P < .05, Mann–Whitney U test; Figure 3 ). There was no significant difference between the 2 groups at 2 weeks after surgery ( P = 0.852).
Wound Architecture
Gaping at the epithelial and endothelial side was seen in 6.7% (2 eyes) and 30% (9 eyes) at 1 day after surgery ( Figure 4 ). Misalignment of incision roof and floor at the endothelial side was seen in 40% (12 eyes), and local detachment of Descemet membrane was found in 36.7% (11 eyes). At 1 week after surgery, gaping at the epithelial side disappeared, and the percentage of eyes with gaping at the endothelial side and misalignment decreased to 13.3%. One patient showed local Descemet membrane detachment at 1 week and 2 week after surgery.




