Purpose
To discuss the implications of the current nomenclature and use of current diagnostic modalities on the classification and treatment of pellucid marginal degeneration and keratoconus.
Design
Perspective analysis of the literature.
Methods
Analysis of published reports on the various treatment methods for pellucid marginal degeneration and keratoconus, and the technologies used in these studies to support the diagnosis and classification of these ectatic disorders.
Results
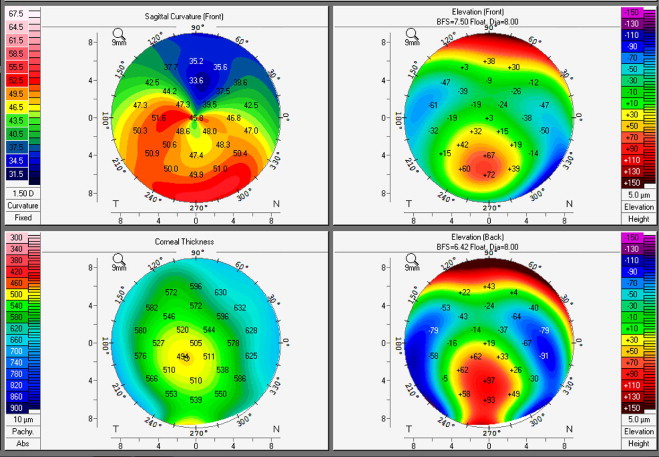
Many studies exploring the different treatment modalities for pellucid marginal degeneration and keratoconus rely mainly on anterior curvature maps to establish the diagnosis of these ectatic disorders, and either do not utilize or disregard information provided by pachymetric maps and posterior elevation maps. In addition, the interchangeability of the nomenclature used to describe these disorders in the literature makes it even more difficult for the clinician to determine the applicability of the results to their patient population.
Conclusions
We propose that future studies minimally include anterior and posterior elevation maps, anterior curvature topography, and full pachymetric maps. This will allow practitioners a better understanding of the study population, and allow them to ascertain when and in whom the treatment modality being explored may be applicable.
‘Tis but thy name that is my enemy;
Thou art thyself, though not a Montague.
What’s Montague?
It is nor hand, nor foot, nor arm, nor face, nor any other part belonging to a man.
O, be some other name! What’s in a name?
That which we call a rose by any other name would smell as sweet;
So Romeo would, were he not Romeo call’d ,
Retain that dear perfection which he owes without that title.
Romeo, doff thy name, and for that name which is no part of thee take all myself.
Juliet; Shakespeare’s Romeo and Juliet , 1600
In the celebrated quote above, William Shakespeare suggests that names do not matter. Shakespeare may have been a prolific bard, but we should all be glad he chose to pick up a quill as opposed to a scalpel, because in medicine names matter.
In 1984 Jay H. Krachmer, Robert S. Feder, and I [Dr Belin] wrote a comprehensive review article for Survey of Ophthalmology titled “Keratoconus and Related Noninflammatory Corneal Thinning Disorders.” We began by posing 2 questions: how do you diagnose early disease, and what is the appropriate treatment? In 1998 Yaron S. Rabinowitz updated the review, stating that in the past 14 years technology has had a major impact on our understanding of keratoconus and asserting that computer-assisted videokeratoscopes represented the most sensitive and sophisticated devices for diagnosing early disease. In the intervening 12 years, newer technologies (eg, Scheimpflug cross-sectional imaging, optical coherence tomography [OCT]) have evolved to further assist the clinician in diagnosing ectatic disorders. More importantly, newer surgical modalities have evolved, necessitating an accurate preoperative diagnosis to insure that the procedures being advocated are appropriately applied and properly utilized.
In this Perspective we will discuss the diagnosis of pellucid marginal degeneration (PMD) and the classification of early, subclinical, or form-fruste keratoconus. Whether PMD and keratoconus (KCN) represent different clinical presentations of the same underlying disease process will not be addressed. That question has yet to be answered and will be left to the biochemists and geneticists. We will discuss the clinical importance and implications of the current, somewhat ambiguous nomenclature. The discussion of what is true PMD and/or what is true KCN is more than just an academic argument, as the correct classification will suggest the appropriate treatment modality, while the incorrect classification can lead to misguided treatments.
Pellucid Marginal Degeneration
In our original review article PMD was described as a typically bilateral, clear, inferior, peripheral corneal-thinning disorder, characterized by a narrow band of corneal thinning (often approaching 20% normal thickness) separated from the inferior limbus by a relatively uninvolved area 1 to 2 mm in width ( Figure 1 ). The cornea protrudes above the area of thinning, resulting in high and irregular astigmatism. The cornea above the band of thinning is of normal thickness and has the most marked anterior displacement just above the band. The resultant astigmatism depends on the location in which it is measured. Above the band of thinning there is a flattening of the vertical meridian and “against-the-rule” astigmatism, while below the band the cornea steepens with increased curvature.
The hallmark of the disease was an inferior band of thinning 1 to 2 mm from the inferior limbus. The disease was typically diagnosed by this classic slit-lamp finding. The advent of Placido-based videokeratoscopes in 1984 3 altered the way we described many corneal disorders. There is no doubt that Placido-based videokeratoscopes greatly improved our ability to identify subtle anterior corneal changes. What is not appreciated is that this increased sensitivity often comes at the expense of specificity. A disease (PMD) that was relatively rare and classically defined by its perilimbal thinning was now being frequently diagnosed solely based on anterior curvature patterns from the central and paracentral cornea. Corneas exhibiting “lobster” or “crab claw” patterns or severe inferior steepening were diagnosed as having PMD without any regard to the corneal thinning.
The confusion is, at least in part, attributable to the limitations of Placido-based anterior curvature topography. Placido systems rely on the analysis of a reflected image and as such are limited to analyzing the anterior corneal surface. Without the additional information from the posterior surface and full pachymetry for depicting patterns of corneal thinning, clinical differentiation is not possible. Additionally, because of the optics of the system and the limitations imposed by the orbital anatomy, in many instances it may only be possible to capture the central 9.0 mm of the cornea with a reflective ring topography system, while the area of maximal pathology may be located outside of this range.
Numerous articles have been published purporting the use of intracorneal ring segments for the surgical management of PMD. The majority of these articles do not show a pachymetric map, fail to describe the classic inferior band of thinning, and rely on the “lobster claw” curvature pattern depicted on anterior curvature maps to confirm the diagnosis. Lee and associates in 2007 reviewed 40 eyes of 26 patients exhibiting the classic “claw pattern” on anterior curvature. Of these, only 9 eyes of 6 patients (23%) met their criteria for true PMD. The authors conclude that “ the topographic patterns (crab claw) are artifacts of the method of data representation and do not accurately portray the cornea’s shape .”
Kymionis and associates reported in 2004 on the use of intracorneal ring segments for the treatment of early PMD. While their description of PMD stated that the disease is characterized by an inferior band of thinning, the case report only showed a “claw pattern” on anterior curvature and central and inferior ultrasound pachymetry measurements of 550/530 microns OD and 560/550 microns OS. They further go on to state that slit-lamp examination showed no evidence of corneal thinning. It is our view that this case may represent typical early keratoconus with inferior displacement of the cone.
Mularoni and associates in 2005 described the use of dissimilar intracorneal rings for the treatment of PMD. They describe the successful treatment of 8 contact lens–intolerant patients. The corneal thickness map depicted in the article did not show a band of thinning and the elevation maps revealed a paracentral island of positive elevation against the best fit sphere, which is typical for an inferior cone.
Ertan and Bahadir in 2006 described the use of the femtosecond laser and intrastromal rings to correct PMD. While no corneal thickness maps were presented, the posterior elevation maps were typical of KCN and not classic PMD.
Kubaloglu and associates in 2010 described the use of a single 210-degree intrastromal corneal ring for the management of PMD. They report on 16 eyes of 10 patients. The topographic figures presented in the article reveal paracentral thinning, no evidence of an inferior band of thinning, and anterior and posterior elevation maps typical of KCN.
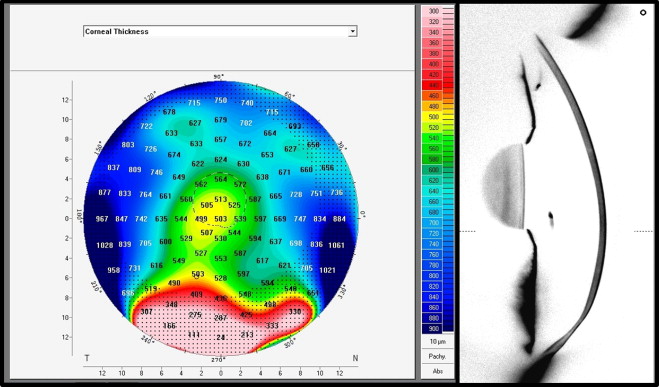
Luck in 2010 reported on the use of a high-power, toric intraocular lens in the management of PMD. While the article describes Scheimpflug imaging, neither pachymetric maps, elevation maps, nor Scheimpflug cross-sectional images were shown. The author, however, was kind enough to supply us with the actual data files and subsequently agreed that this was a case of KCN and not PMD, as the cornea had the typical thickness map seen with keratoconus ( Figure 2 ).
Many other reports purporting treatment modalities for PMD fail to show clear evidence supporting the diagnosis of PMD. The clinical importance of this may not be initially evident. While the use of a toric intraocular lens is more dictated by the overall refractive state of the eye and there would be little, if any, consequence of misdiagnosing PMD, the same cannot be said for intracorneal rings (ICR). ICR work, in part, by encompassing the ectatic region and causing a flattening of the surrounded tissue. In true PMD the area of maximal ectasia would fall outside of any currently available ICR. The results of ICR in keratoconus may not be applicable to true PMD. Additionally, the risk of intrastromal dissection in true PMD, where there is a dramatic change in corneal thickness, is likely very different.
More recently, reports have appeared reporting the combined use of customized photorefractive keratectomy (PRK) and collagen cross-linking or PRK and collagen cross-linking after the insertion of ICR segments. Both of these papers only demonstrate anterior curvature maps depicting a “claw type” pattern. Pachymetry maps were not presented and the ultrasound thickness measurements described are not compatible with true PMD.
In the authors’ opinion, future articles asserting specific treatment modalities for PMD should minimally include, in addition to corneal topography, a full corneal pachymetric map to differentiate inferior keratoconus from true PMD and allow the clinician to know what patients may be appropriate for the treatment being described.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


