Purpose
To compare clinical outcomes after vitrectomy and internal limiting membrane (ILM) peeling, with and without gas tamponade, for the treatment of myopic foveoschisis.
Design
Retrospective, comparative, interventional case series.
Methods
In this retrospective clinical study, 17 eyes of 17 consecutive patients underwent vitrectomy and ILM peeling for treatment of myopic foveoschisis. Eyes were divided into 2 groups, those with gas tamponade (n = 9) and those without (n = 8). Gas tamponade was chosen according to the period and surgeon’s discretion. The changes of foveal anatomy on preoperative optical coherence tomography (OCT) were not considered in the decision. Main outcome measures were the rate of resolution of myopic foveoschisis measured by OCT, the time interval until resolution of myopic foveoschisis, central foveal thickness, and best-corrected visual acuity (BCVA).
Results
After surgery, OCT showed a resolution of myopic foveoschisis in 8 eyes (88.9%) in the gas-treated group and in 6 eyes (75.0%) in the no-gas group. This difference between the groups was statistically insignificant ( P = .576). The mean period until the resolution of myopic foveoschisis was 2.25 months in the gas-treated group and 4.50 months in the no-gas group ( P = .011). The mean BCVA improved significantly in both the gas-treated and no-gas groups ( P = .011 and P = .017, respectively).
Conclusions
Vitrectomy and ILM peeling without gas tamponade appears to be as effective in the treatment of myopic foveoschisis as vitrectomy with gas tamponade. However, eyes treated with gas tamponade showed more rapid resolution of myopic foveoschisis.
Myopic foveoschisis is one of the major causes of poor vision in highly myopic eyes. Its prevalence has been reported to range from 8% to 34%. Its pathogenesis remains uncertain. Several factors, including vitreous traction of residual premacular vitreous cortex, rigidity of the internal limiting membrane (ILM), stiffness of retinal vessels, and posterior staphyloma, have been suggested to have a role in the development of myopic foveoschisis. Retinal schisis, defined as complete separation between retinal layers, assumes a condition that cannot be improved functionally. A good visual improvement after repositioning of the retinal layers indicates that this condition may be a form of retinal edema resulting from traction rather than true retinoschisis. The term “myopic traction maculopathy” was proposed for this disease entity.
Many studies have revealed that vitrectomy, with or without ILM peeling and gas tamponade, is an effective treatment for myopic foveoschisis. Gas tamponade has been used in the treatment of myopic foveoschisis, inducing retinal repositioning by pushing the retina back. However, it remains unclear whether gas tamponade is essential for the treatment of myopic foveoschisis, and its efficacy has not been established. The purpose of our study was to compare clinical outcomes after vitrectomy and ILM peeling, with and without gas tamponade, in the treatment of myopic foveoschisis.
Methods
We conducted a retrospective review of the medical records of 17 eyes in 17 consecutive patients with myopic foveoschisis who underwent vitrectomy with ILM peeling between November 1, 2007 and February 28, 2010 at the Seoul St. Mary’s Hospital of the Catholic University of Korea.
Surgical indications were macular retinoschisis with or without foveal detachment, as confirmed by optical coherence tomography (OCT) and symptomatic visual loss, or metamorphopsia attributable to foveoschisis associated with high myopia. Patients with macular hole detected by OCT were excluded. Eyes were divided into 2 groups: the gas-treated group, which underwent vitrectomy with gas tamponade, and the no-gas group, which underwent vitrectomy without gas tamponade. All patients were followed for at least 12 months.
All patients underwent a complete ocular examination at baseline and at each follow-up visit, including Snellen best-corrected visual acuity (BCVA) test and dilated fundus examination with slit-lamp biomicroscopy. A-scan ultrasonography was obtained at baseline for measurement of axial length. OCT was performed monthly at each visit, until complete resolution of foveoschisis was observed. Stratus OCT (Carl Zeiss Meditec, Dublin, California, USA) was used primarily. Spectral-domain OCT (Cirrhus OCT; Carl Zeiss Meditec) was also used once it became available, to obtain more detailed images of macular structure. The morphology of myopic foveoschisis was classified into 2 types based on the foveal anatomy by OCT: macular retinoschisis with foveal detachment (foveal detachment type) and without foveal detachment (retinoschisis type).
All operations were performed by one experienced surgeon (W.K.L.). All patients underwent pars plana vitrectomy and ILM peeling, with and without gas tamponade. Cataract surgery was performed in all 13 phakic eyes to avoid cataract progression. Triamcinolone acetonide (0.1 mL at 40 mg/mL; Dongkwang Pharmaceutical, Seoul, Korea) was injected into the vitreous cavity for visualization of the posterior vitreous cortex during vitrectomy. Indocyanine green dye (ICG, 5 mg/mL; Dongindang Pharmaceutical, Shihung, Kyunggi-do, Korea) was then used for staining of the ILM. The ILM was peeled using intraocular forceps over 2 to 3 disc diameters in all eyes. In 9 eyes, fluid-air exchange was performed, followed by gas tamponade with 14% perfluoropropane (C 3 F 8 ). The decision to use gas tamponade was made based on the study period and the surgeon’s discretion. The changes of foveal anatomy on OCT at baseline, such as height of retinoschisis and presence of retinal detachment, were not considered in the decision. In the early period of the study, we used gas tamponade in most cases. Later, gas tamponade was performed only when a suspicious macular hole developed (1 eye) or paravascular breaks were noted during surgery (1 eye). Patients with gas tamponade were instructed to maintain a prone position for at least 1 week.
Main outcome measures included the rate of resolution of myopic foveoschisis by OCT. We also followed the time interval until the resolution of myopic foveoschisis, central foveal thickness (CFT), postoperative BCVA, and changes in visual acuity. In this study, resolution of myopic foveoschisis was defined as resolution of central macular retinoschisis in retinoschisis-type eyes, and as resolution of central macular retinoschisis as well as reattachment of detached foveal retina in foveal detachment–type eyes.
For statistical analysis, Snellen visual acuity was converted to the logarithm of the minimal angle of resolution (logMAR units). Improvement or deterioration of visual acuity was defined as a change of 0.3 or more logMAR units. Preoperative and postoperative clinical parameters were compared using Mann-Whitney U tests for continuous variables, and using Fisher exact tests for categorical variables. Wilcoxon signed rank tests were used for comparisons of visual change within a group. The SPSS software (version 12.0 software for Windows; SPSS, Inc, Chicago, Illinois, USA) was used for statistical analyses. P values < .05 were considered to indicate statistical significance.
Results
Baseline Characteristics
In total, 17 eyes of 17 consecutive patients undergoing surgery for treatment of myopic foveoschisis were included in the study. Nine eyes (52.9%) were in the gas-treated group and 8 eyes (47.1%) were in the no-gas group. Table 1 summarizes the baseline characteristics of the patients. All patients were female. The mean age was 61.9 years (range, 44–78 years). Mean axial length was 29.75 mm (range, 27.80–32.95 mm) and mean refractive error in 13 phakic eyes was −15.41 diopters (D) (range, −11.25 to −22.88 D). The lens status ranged from C1N0P0 to C2N2P0, following Lens Opacities Classification System III. Baseline OCT classified 7 eyes as foveal detachment type and 10 eyes as retinoschisis type. The mean duration of symptoms was 7.88 ± 3.98 months (range, 3–12 months) in the gas-treated group and 7.13 ± 5.51 months (range, 1–18 months) in the no-gas group. The mean CFT was 573 ± 149 μm (range, 390–777 μm) in the gas-treated group and 538 ± 207 μm (range, 248–822 μm) in the no-gas group. The mean logMAR BCVA at baseline was 0.81 ± 0.18 (Snellen equivalent of 20/129, range, 20/200–20/63) in the gas-treated group and 0.83 ± 0.18 (Snellen equivalent of 20/134, range, 20/200–20/63) in the no-gas group. The mean follow-up period after surgery was 15.3 (range, 12–22) months in the gas-treated group and 13.0 (range, 12–15) months in the no-gas group. No statistically significant differences in age, refractive error, axial length, lens status, foveal anatomy on OCT, duration of symptoms, baseline CFT, baseline visual acuity, or follow-up period were observed between the 2 groups ( Table 1 ).
| Variable | Gas-Treated Group (n = 9) | No-Gas Group (n = 8) | P Value |
|---|---|---|---|
| Age (years), mean ± SD | 61.78 ± 8.98 | 62.13 ± 10.10 | >.999 a |
| Sex (male/female) | 0/9 | 0/8 | |
| Axial length (mm), mean ± SD | 29.31 ± 1.10 | 30.24 ± 1.55 | .211 a |
| Refractive error in phakic eyes (D), mean ± SD | −18.21 ± 4.36 | −14.21 ± 3.10 | .138 a |
| Duration of symptoms (months), mean ± SD | 7.88 ± 3.98 | 7.13 ± 5.51 | .590 a |
| Lens status | .576 b | ||
| Phakia/pseudophakia | 6/3 | 7/1 | |
| OCT finding | .637 b | ||
| Foveal detachment type, no. (%) | 3 (33.3) | 4 (50.0) | |
| Retinoschisis type, no. (%) | 6 (66.7) | 4 (50.0) | |
| Central foveal thickness (μm), mean ± SD | 573 ± 149 | 538 ± 207 | .847 a |
| Baseline BCVA in logMAR, mean ± SD | 0.81 ± 0.18 | 0.83 ± 0.18 | .921 a |
| Follow-up (months), mean ± SD | 15.33 ± 4.33 | 13.00 ± 1.41 | .375 a |
Anatomic Results
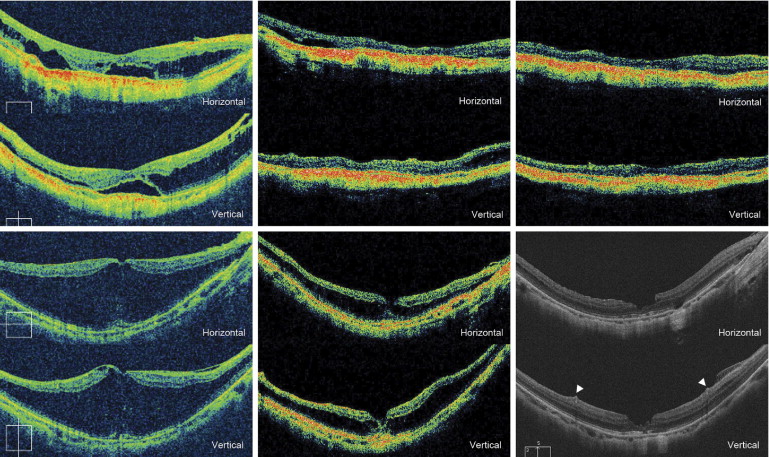
At 12 months after initial vitrectomy, resolution of myopic foveoschisis was achieved in 8 of 9 eyes (88.9%) in the gas-treated group and in 6 of 8 eyes (75.0%) in the no-gas group ( Table 2 ). This difference between the groups was statistically insignificant ( P = .576). The mean CFT improved significantly, from 573 ± 149 μm and 538 ± 207 μm at baseline to 208 ± 95 μm (range, 126–435 μm) and 324 ± 153 μm (range, 119–611 μm) at 1 month ( P = .012) and 137 ± 45 μm (range, 85–238 μm) and 132 ± 23 μm (range, 94–171 μm) at 12 months ( P = .012) in the gas-treated and no-gas groups, respectively. At 1 month, the mean CFT was lower in the gas-treated group than in the no-gas group, but the CFT did not differ significantly between the groups at 1 month ( P = .059) or 12 months ( P = .834). The mean period until the resolution of myopic foveoschisis was 2.25 months (range, 1–3 months) in the gas-treated group and 4.50 months (range, 2–8 months) in the no-gas group; this difference was statistically significant ( P = .011). Among 14 eyes showing anatomic resolution, 12 eyes achieved complete resolution of myopic foveoschisis on the entire macular area ( Figure 1 ) . However, the remaining 2 eyes, 1 from the gas-treated group and the other from the no-gas group, had persistent focal retinoschisis outside of the central macula at the final visit ( Figure 2 ) .
| Variable | Gas-Treated Group (n = 9) | No-Gas Group (n = 8) | P Value |
|---|---|---|---|
| Resolution of MF | |||
| No. (%) | 8 (88.9%) | 6 (75.0%) | .576 a |
| Time interval (months), mean ± SD | 2.25 ± 0.71 | 4.50 ± 1.97 | .011 b |
| Preoperative OCT finding (FD type/RS type) | 2/6 | 3/3 | |
| Central foveal thickness (μm), mean ± SD | |||
| Baseline | 573 ± 149 | 538 ± 207 | .847 b |
| 1 month ( P value c ) | 208 ± 95 (.012 d ) | 324 ± 153 (.012 d ) | .059 b |
| 12 months ( P value c ) | 137 ± 45 (.012 d ) | 132 ± 23 (.012 d ) | .834 b |
| Complications | |||
| MH with or without RD, no. (%) | 2 (22.2%) | 0 (0.0%) | .471 a |
| Peripheral retinal break, no. (%) | 0 (0.0%) | 0 (0.0%) | >.999 a |
| BCVA (logMAR), mean ± SD | |||
| Baseline | 0.81 ± 0.18 | 0.83 ± 0.18 | .921 b |
| 12 months ( P value c ) | 0.56 ± 0.19 (.011 d ) | 0.56 ± 0.23 (.017 d ) | .922 b |
| Visual improvement in logMAR, mean ± SD | 0.26 ± 0.17 | 0.26 ± 0.18 | .922 b |
| Change in visual acuity, no. (%) | |||
| Improved, ≥0.3 logMAR | 5 (55.6%) | 5 (62.5%) | |
| Stable | 4 (44.4%) | 3 (37.5%) | |
| Worsened, ≥0.3 logMAR | 0 (0.0%) | 0 (0.0%) |
c P value between preoperative and postoperative data.