Vascular Malformations
Any orbital vascular problem, especially the arteriovenous (AV) communication engenders a good deal of anxiety not only on the part of the patient and the referring physician but also the orbital specialist. The thought of uncontrolled bleeding, be it vigorous or even just a persistent ooze, is not appealing to anyone at any level of training. The tumefactions discussed in this chapter are a heterogeneous group of “abnormalities,” “anomalies,” “aberrations,” “dilatations,” “enlargements,” and “intercommunications” of established vascular channels that we elect to lump together simply as malformations. They are composed, either entirely or in part, of arteries and veins of variable size and in various combinations. We will restrict our discussion to those malformations of nontraumatic origin that may be primarily intraorbital or located in an adjoining space, where their size may alter the dynamics of the orbital vascular circulation. Whether primary or secondary in anatomic type, they produce proptosis or an orbital symptomatology that must be considered in the differential diagnosis of orbital tumors. We once again reference the work of Harris (1999) and Rootman (2003) in the consideration of orbital vascular disease. Rather than discuss morphology, we will classify these tumefactions on the basis of their hemodynamic properties because this is germane to patient management. The classification has three primary categories: No flow, venous flow or arterial flow. The no flow lesion is typified by the lymphangioma; the venous flow lesion is typified by the orbital varix (both distensible and nondistensible variety); and the lesion with arterial flow is typified by the AV malformations or arteriolized veins distal to them.
The nontraumatic malformations comprise 4% (72 out of 1,795) of our total tumor series (Chapter 3). Most are secondary in type and make up 7.6% (56 out of 732) of the group of secondary tumors. They are the fourth most common secondary orbital tumor. There is a strong preponderance among women, outnumbering men in a ratio of 4:1. They occur in all age-groups, but the majority, 68% (49 out of 72), are clustered in individuals over 50 years of age. A future survey of this type, predictably, will show an increase in the number of vascular malformations relative to the total tumors because of the diagnostic capabilities of the newer imaging methods, particularly magnetic resonance imaging (MRI).
Orbital Aneurysm
In this subchapter, we reserve the term aneurysm for a vascular dilatation, the makeup of which is entirely arterial. In the orbit, such an aneurysm would involve the intraorbital portion of the ophthalmic artery or one of its branches. Over 40 years ago, the literature was rife with reports of orbital aneurysm, in which diagnosis was chiefly based on clinical findings. In retrospect, many such cases were a mixture of arteries and veins. The advent of angiography differentiated the several types of vascular dilatations. Later, improvements in surgical techniques encouraged exploration and excision of these lesions, further narrowing the diagnosis of aneurysm to only a very few histopathologically proved cases.
In the 1980 edition of our text, this situation was reviewed in some detail. We summarized the cases in the literature in English language, which were confirmed by angiography or surgical exploration, and added three of our own. We estimated that the total of well-studied cases of orbital aneurysm did not exceed 16, including some in the literature in foreign languages, which were not annotated by us. This underscores the rarity of this lesion in the orbit.
We have not seen a new case but there have been three case reports of aneurysms of the ophthalmic artery in the orbital apex in the literature in English language since 1971 (Ogawa et al., 1992; Kikuchi and Kowada, 1994; Ernemann et al., 2002). One of these was in association with a dural AV malformation of the anterior fossa skull base and the authors speculated whether the hemodynamic stress of the fistula had played a role in the genesis of the aneurysm (Kikuchi and Kowada, 1994). Those well-studied cases from the literature that we annotated in the 1980 edition are referenced at the end of this chapter for the interest of new readers who would not have access to the 1980 text, because it has long been out of print.
The three cases from the Mayo survey were all women aged 26, 31, and 63 years, all with the involvement of the right orbit. Diagnosis was made by angiography. The feeding vessel of one aneurysm was surgically ligated with only partial relief of orbital symptomatology; one case was surgically deferred because of left-sided seizures following angiography and was subsequently lost to follow-up; and the third case underwent management of the aneurysm elsewhere.
In the clinical assessment of a case of presumed aneurysm, it is important to keep in mind that the location (orbital or nonorbital) of the aneurysm along the ophthalmic artery may determine the presenting symptomatology. The intraorbital aneurysm is basically a mass lesion chiefly characterized by proptosis. Beyond this symptom, the clinical picture is not well standardized. Ancillary findings are bloodshot eye, impairment of ocular motility, pain or headache on the affected side, pulsation of eye, and subjective or objective bruit. These ancillary signs and symptoms vary in number, severity, and combinations.
The nonorbital aneurysms are located either in the extreme proximal intracranial portion of the artery or in its intracanalicular course. In both, the presenting picture includes visual loss, visual field defects, pallor or atrophy of the optic disk, deep orbital pain, and neurogenic type motility paresis, but no proptosis. In the rare instances in which the entire artery is involved, there may be combinations of both of the above clinical presentations but, more often, the picture is that of the nonorbital aneurysm.
The past management of these lesions included temporary surgical compression, clipping, embolization, ligatures, excision, and conservative observation. The choice depended on the severity of symptoms and the size of the aneurysm.
Arteriovenous Communications
Most of the vascular malformations affecting the orbit are due to some abnormal communication between arteries and veins. The most common of these AV communications result from an abnormal flow of blood directly into the cavernous sinus from a defect in the intracavernous segment of the internal carotid artery or indirectly through intervening branches of the internal carotid or external carotid arteries. We will discuss this group first. A discussion of the less common AV communications not based on an arterial communication with the cavernous sinus will follow. In both subgroups, the mechanism of the orbital tumefaction is secondary to a rise in the orbital venous pressure. As noted earlier, we will exclude those cases in which the malformation is due to trauma and will dwell only on those cases of spontaneous type of unknown origin.
Carotid-Cavernous Fistula
Terminology and Classification
Fistula is a term that has long been associated with the high-pressure flow of arterial blood into the cavernous sinus resulting from trauma. Fistula connotes a cleft or break in the feeding artery and is also a suitable term for the direct, spontaneous carotid-cavernous communication. Dural shunt, currently, is a popular designation that emphasizes the participation of a plexus of small meningeal vessels in the carotid-cavernous intercommunication, with the understanding that the carotid artery, as it passes through the cavernous sinus, is intact.
Barrow et al. (1985), in an effort to standardize a system for judging symptomatology, management, and prognosis, proposed a classification based on angiographic findings rather than the hemodynamic properties of the carotid-cavernous fistulas. They divided them into four types: Type A, a direct high-flow “shunt” between internal carotid artery and cavernous sinus (there is a defect within the intracavernous carotid artery); type B, an indirect communication involving meningeal branches of internal carotid; type C, an indirect communication involving meningeal branches of external carotid; and type D, an indirect communication involving branches of both internal and external carotid artery systems. The “direct” or the type A defect is associated with an intracavernous sinus carotid artery defect and is synonymous with the carotid-cavernous fistula or the “high-flow” fistula. The indirect fistulas are the types B, C, and D. The intracavernous carotid artery, by definition, is intact. These are the so-called dural fistulas or the “low-flow” shunts. We shall refer to this classification later. This can be further classified as whether the onset was traumatic or spontaneous. The traumatic fistula is primarily the concern of the neurosurgeon, but the spontaneous type is usually seen initially by the ophthalmologist.
Incidence
Fifty-one of our patients are classified in the spontaneous category. Forty-three are women; eight are men, a ratio of approximately 5.4 to 1. The age range is 31 to 84 years with a mean of 62.5 years. Seventy-six percent (39 out of 51) of the cases were clustered in a 24-year age span of 48 through 72 years. The right orbit was involved in 27 cases, the left orbit in 19 cases, and bilateral orbital involvement was present in five patients. Incidence data based on other publications are scant because these reports include a mix of traumatic and spontaneous cases. Two other surveys, each reporting ten cases of spontaneous dural shunts, are those of Newton and Hoyt (1970) and Grove (1984). Both publications cite the prevalence of the fistula in women and the concentration of cases in the sixth and seventh decades of their life span.
Clinical Features
No other tumefactions of the orbit are associated with such a variety of symptoms and signs as the carotid-cavernous fistulas
with secondary orbital manifestations. There is no single feature that will always appear in all cases. Neither will all the clinical features be present in any given case. For the purpose of analysis, we have divided the presenting manifestations of our patients into ten principal subgroups. These are summarized in Table 11.1.
with secondary orbital manifestations. There is no single feature that will always appear in all cases. Neither will all the clinical features be present in any given case. For the purpose of analysis, we have divided the presenting manifestations of our patients into ten principal subgroups. These are summarized in Table 11.1.
Table 11.1 Principal Presenting Features of 51 Patients with Spontaneous Carotid-Cavernous Fistulas in Order of Decreasing Frequency: Mayo Clinic 1948–1995 | |||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Redness and congestion of the eye owing to dilation and tortuosity of the epibulbar venous plexus are the most common and striking features of these fistulas with secondary orbital manifestations. The plexus of corkscrew vessels extends directly to the limbus of the eye and has a brighter red hue than an average vein. The plexus of vessels is often more prominent on one sector of the globe than another (see Fig. 11.1). The tissue spaces between the dilated vessels tend to retain their normal color unless chemosis supervenes. Patients usually refer to their eye as bloodshot. Occasionally, this increase in epibulbar venous pressure is manifest only as a chronic subconjunctival hemorrhage.
Second in frequency is proptosis of the eye. Usually the proptosis is straightforward, but, with time, downward displacement occurs owing to persistent engorgement of the superior ophthalmic vein. The proptosis averaged 4.9 mm with a range of 3 to 9 mm in our group of patients. One patient had a sudden and dramatic increase in proptosis noted in association with a probable thrombosis of the superior ophthalmic vein (vida infra).
Some degree of impairment of ocular motility with diplopia was the third most frequent presenting manifestation. It was mild in degree in approximately half of the 32 patients with an ocular motility disorder and consisted of a limitation of gaze in all directions. This milder disability probably was due to the bulk effect of the suffused orbital tissues on ocular rotations. Such patients likely would show some enlargement of the extraocular muscles and an enlarged superior ophthalmic vein on computed tomography (CT) scan. In another 30% of these patients, the impairment was more severe owing to a sixth cranial nerve palsy. Bilateral sixth cranial nerve paresis also was a common accompaniment of bilateral orbital tumefactions. The remaining 20% of patients had severe ophthalmoplegia, secondary to pressure on both the third and sixth cranial nerves in their intracavernous course.
Headache, deep orbital pain, bruit, and head noise occurred in only 48% of the total series but were distressing
and noteworthy features of the anamnesis when present. The head noise was described as buzzing, pounding, blowing, swishing, or simply “strange,” and often was lateralized to the ipsilateral ear. The bruit, when present, had no localizing significance. Interestingly, the patient, described in the subsequent text, had a sudden cessation of her bruit in association with thrombosis of the superior ophthalmic vein (SOV) and cavernous sinus. Two patients had orbital pain prior to diagnosis of indirect shunts that responded to prednisone. Facial pain is well described in association with direct and indirect fistulas (Brazis et al., 1994; Sugano et al., 2003; Jensen et al., 2004)
and noteworthy features of the anamnesis when present. The head noise was described as buzzing, pounding, blowing, swishing, or simply “strange,” and often was lateralized to the ipsilateral ear. The bruit, when present, had no localizing significance. Interestingly, the patient, described in the subsequent text, had a sudden cessation of her bruit in association with thrombosis of the superior ophthalmic vein (SOV) and cavernous sinus. Two patients had orbital pain prior to diagnosis of indirect shunts that responded to prednisone. Facial pain is well described in association with direct and indirect fistulas (Brazis et al., 1994; Sugano et al., 2003; Jensen et al., 2004)
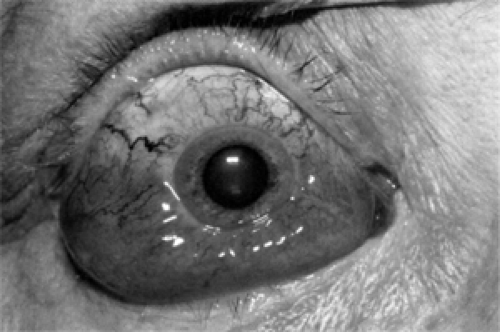 Figure 11.1 Spontaneous indirect carotid-cavernous fistula: Dilated, corkscrew veins on the superior surface of right eye with marked chemosis inferiorly of 1 week duration in a 64-year-old woman who had noted a swishing head noise. Angiography showed a low-flow fistula supplied by terminal branches of the internal maxillary artery, and inferior hypophyseal and dorsal meningeal branches of internal carotid artery. Orbital process underwent resolution following angiography with full recovery over subsequent 16 months. (Courtesy Bartley GB, M.D., Rochester, MN.) (See Color image.) |
Eyelid manifestations such as fullness, puffiness, drooping, and swelling did not contribute significantly to diagnosis although present in 45% of total cases. Inability to elevate a nonswollen lid was indicative of a partial third nerve palsy.
Curiously, the 37% incidence of secondary glaucoma is much lower than we anticipated. Studies on smaller but similar series of carotid-cavernous fistulas that have been published by ophthalmologists tend to emphasize secondary glaucoma as one of the three main manifestations (Keltner, 1987). The latter may reflect the ocular rather than orbital orientation of such studies. In roughly 50% of our series of 19 patients with secondary glaucoma, the elevation of intraocular pressure was mild to moderate in degree and was controlled with medical therapy. In the other 50%, the intraocular pressure was high, recalcitrant to medical measures, and was a motivating factor to pursue surgical management of the fistula. Glaucoma surgery alone was not an effective control in our limited experience with one patient. The secondary glaucoma was unilateral except in one patient with bilateral orbital findings.
Pulsation of the eye, which in an earlier era was considered the most obvious and frequent sign of a fistula, was present in only 16% of the total series. It tended to be present in those patients with the higher blood volume communications, which resulted in a greater degree of proptosis, although this relationship was not absolute. Often, its presence was one of the major determinants on which therapeutic surgical intervention was based.
Considering the complex symptomatology and the prevalent proptosis of significant degree, we were surprised that only 11 patients (22%) presented with a visual acuity <20/30. A central scotoma was present in three of the eight patients, reflecting the altered vascular dynamics of the optic nerve associated with the increased intraorbital pressure. These three patients were the only ones with a visual acuity of 20/200 or less. Prior to availability of the now routine endovascular techniques, a 59-year-old woman had a left indirect type B fistula with drainage through the contralateral SOV. Externally, both eyes were quite red and chemotic. Visual acuity was 20/50 right eye and 20/40 left eye. Each fundus displayed superficial retinal hemorrhages and deep round retinal hemorrhages consistent with marked venous obstruction. Bilateral disk edema and cystoid macular edema were also present. The cavernous sinus was explored and the fistula was repaired. Postoperative follow-up was limited but the left eye remained the same whereas the right eye vision dropped to 20/400 secondary to a central retinal vein occlusion. Another patient, a 49-year-old woman, was seen for further evaluation of a one-week history of visual loss, which was a presumed exacerbation of her well established Graves ophthalmopathy. Visual acuity was 20/60 in the right eye with a mild afferent papillary defect (the left eye was amblyopic); 6 mm proptosis was recorded; and corkscrew vessels going to the limbus were present. The right optic disk was mildly swollen (see Fig. 11.2A and B). CT scanning showed enlarged extraocular muscles in the right eye, greater than in the left eye, (Fig. 11.2C) consistent with a diagnosis of Graves ophthalmopathy, but the right SOV was enlarged (Fig. 11.2D). There was not felt to be enough extraocular muscle enlargement to support a diagnosis of Graves optic neuropathy so the plan was to proceed with an angiogram that revealed an indirect right carotid-cavernous sinus fistula that was being fed by both meningohypophyseal arteries and branches from the right internal maxillary artery. The lesion could not be completely treated with endovascular techniques. When she returned 3 weeks later, the visual acuity had dropped to 5/200, and she reported numerous episodes of no-light-perception vision lasting up to 30 minutes. The right cavernous sinus was explored and packed. Postoperatively, she was asymptomatic and the visual acuity improved although she has a hypesthetic cornea. Final visual acuity was 20/25 with 13 months of follow-up. In general, ophthalmoscopic findings did not play a major role in the patients’ disabilities, other than those with central scotomas. It is intriguing that eyes of these 50- to 80-year-old individuals can withstand the rise of intraorbital pressure attendant to this entity with so little impairment of vision, unlike the higher incidence of visual impairment associated with a similar event in infants with capillary hemangioma.
Another interesting finding was the absence of a palpable mass in all 38 patients. Neither was the orbital swelling exacerbated by the Valsalva maneuver, although some patients noted a difference in symptoms with changes in posture or head position.
A further study of our data revealed that patients presented with an average of five of the diagnostic groups listed in Table 11.1. This underscores the heterogeneous mix of orbital symptoms and signs associated with spontaneous fistulas. We also analyzed our patients in terms of the angiographic classification of Barrow, which was described earlier. A type A communication was present in 9 patients, type B in 12 patients, type C in 2 patients, and type D in 24 patients. In four patients who underwent angiography in the 1960s, the feeder arteries were not detailed. No correlation was found between the angiographic classification and the number or character
of the diagnostic groups in Table 11.1. This suggests that factors other than the arterial components of the vascular communication may play a part in the degree of orbital engorgement and clinical presentation.
of the diagnostic groups in Table 11.1. This suggests that factors other than the arterial components of the vascular communication may play a part in the degree of orbital engorgement and clinical presentation.
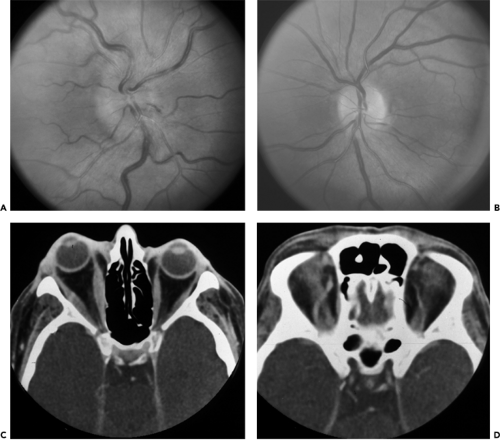 Figure 11.2 Indirect carotid-cavernous fistula in a 49-year-old woman. Disk edema right eye (A) is obvious compared to normal left optic disk (B). Axial computed tomography scan (C) shows fusiform enlargement of medial and lateral rectus muscles, right eye greater than left eye. Morphology of enlargement is consistent with patient’s known Graves ophthalmopathy. There is not enough apical compression to produce optic neuropathy/disk edema. Axial computed tomography scan (D), higher view demonstrates asymmetry with right superior ophthalmic vein enlarged. (See Color image.) |
The duration of symptoms prior to presentation usually extended over a period of months in 45 of our 51 patients. The average duration was 6.4 months with a range of 0.5 to 36 months. The median of the duration curve was 5.1 months. There was a noticeable trend toward earlier diagnosis in the last 10 years, most likely reflective of wider availability of neuroimaging and endovascular therapy. The onset of the orbital problem was commonly associated with some noticeable or startling event, such as headache or pain in the affected orbit associated with vomiting, sudden appearance of diplopia, red eye, or head noise. In this respect, these fistulas differ from other orbital tumors—except some metastatic carcinomas—in the more prominent delineation of their onset. In one patient, symptoms of right-sided face pain, blepharoptosis, and bruit commenced 3 days before physician evaluation.
Another event peculiar to this disorder is the tendency of some patients to have a severe exacerbation of symptoms
before undergoing clinical improvement. This paradox of “getting worse before getting better” was ascribed to a thrombosis of the SOV by Sergott et al. (1987). They reported three cases of this “dural-cavernous malformation.” Their cases were angiographically proved in women in the 70 plus age range. The first case initially was thought to have either a low-flow or early thrombosis through the SOV. When symptoms worsened, a repeat imaging by MRI demonstrated evolution of the thrombosis. Within 19 days of this event, her signs and symptoms improved. In their second case, the orbital manifestations increased in severity 1 month after onset. A second arteriogram disclosed a thrombosis of the SOV. This was quickly followed by fever and a clinical picture suggestive of orbital cellulitis, but blood cultures were negative. The patient was treated with antibiotics. Thirty-five days later the problem had resolved. Their third case involved a sudden increase in a preexisting proptosis. Angiography and MRI demonstrated thrombosis of SOV and the patient improved spontaneously within 16 days.
before undergoing clinical improvement. This paradox of “getting worse before getting better” was ascribed to a thrombosis of the SOV by Sergott et al. (1987). They reported three cases of this “dural-cavernous malformation.” Their cases were angiographically proved in women in the 70 plus age range. The first case initially was thought to have either a low-flow or early thrombosis through the SOV. When symptoms worsened, a repeat imaging by MRI demonstrated evolution of the thrombosis. Within 19 days of this event, her signs and symptoms improved. In their second case, the orbital manifestations increased in severity 1 month after onset. A second arteriogram disclosed a thrombosis of the SOV. This was quickly followed by fever and a clinical picture suggestive of orbital cellulitis, but blood cultures were negative. The patient was treated with antibiotics. Thirty-five days later the problem had resolved. Their third case involved a sudden increase in a preexisting proptosis. Angiography and MRI demonstrated thrombosis of SOV and the patient improved spontaneously within 16 days.
We have seen this paradoxical symptomatology in three patients of our series. In one, a 77-year-old woman, the sudden thrombosis of the SOV was angiographically demonstrated 4 months after embolization of the external carotid supply to a dural fistula. In the other patient, a 64-year-old woman, the thrombosis and exacerbation of the orbital disorder immediately followed diagnostic angiography. The last case was quite dramatic. An 84-year-old woman had spontaneous onset of a “carotid-cavernous sinus fistula” 1 month prior to evaluation. There was 4 mm proptosis and the eye was injected with minimal chemosis. A dull ache was present. Visual acuity was 20/60, the intraocular pressure was 21 (the fellow eye was 20/25 with intraocular pressure of 11), 4 mm proptosis was present and there was mild sixth nerve paresis. No specific therapy was given, and then one day prior to evaluation she noted an abrupt worsening of the proptosis, chemosis, reduced visual acuity and marked orbital pain (see Figs. 11.3A and B). The bruit that had been present was now gone. Visual acuity was 20/400 with a mild afferent papillary defect. The lids were minimally swollen and ecchymotic whereas the globe was quite injected with minimal chemosis. The globe was “fixed” and 9 mm proptosis was present. The anterior chamber was very shallow although the intraocular pressure was 23. Massive choroidal effusions were present with evidence of a central retinal vein occlusion with disk edema. An angiogram suggested that an intracavernous carotid artery aneurysm had ruptured and spontaneously thrombosed as there was no flow within the right SOV, cavernous sinus or inferior petrosal sinus. An incidental 5 mm internal carotid artery aneurysm was noted within the left cavernous sinus. No specific therapy was given and within 1 week there was marked clinical improvement. One month later, visual acuity was 20/40, the intraocular pressure was 11, and the choroidal effusions had resolved although there was still evidence of a mild central retinal vein occlusion.
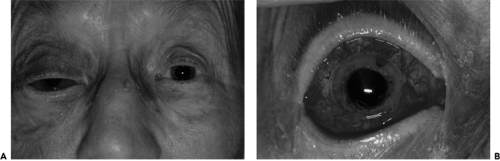 Figure 11.3 Spontaneous direct carotid-cavernous fistula with subsequent spontaneous thrombosis. An 84-year-old woman with rupture of intracavernous carotid artery aneurysm. The lesion underwent spontaneous thrombosis of cavernous sinus, superior ophthalmic vein and inferior petrosal sinus commensurate with pain and clinical deterioration. Proptosis of 9 mm was present and globe was immobile (A). Arterialized episcleral vessels coming to limbus. Note shadow of choroidal effusions temporally and nasally (B). (See Color image.) |
One last feature of importance is the rare presentation of younger women with the symptomatology of carotid-cavernous fistula. In these 20- and 30-year-old women, a pregnancy is likely the triggering mechanism. Upon completion of the pregnancy, the orbital manifestations subside only to recur if a second pregnancy occurs. Such recurrences may be so severe that an early termination of pregnancy may be necessary.
Imaging Aspects
Most attention, in the past, has been given to the display of the carotid-cavernous sinus fistula because of its traumatic
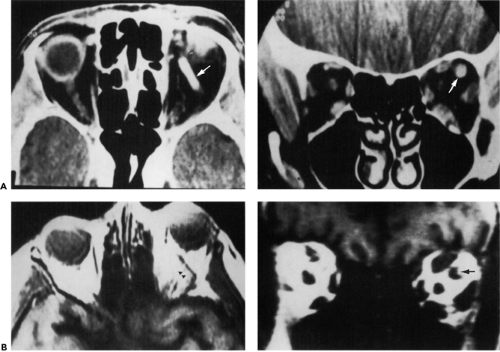
origin, high morbidity, guarded prognosis, and tricky management. The “Johnny-come-lately” spontaneous type has received less attention. In the latter, ultrasonography will show the dilated SOV and the enlarged extraocular muscles that usually occur, but echographic findings and clinical assessment are not always in agreement (Phelps et al., 1982). CT scan also shows the enlarged veins and the swollen muscles in the orbit (see Fig. 11.4A). The coronal scan is particularly useful in demonstrating the symmetrical thickening of the extraocular muscles unlike the asymmetric enlargement of extraocular muscles of Graves orbitopathy although this is not a constant finding. Some observers comment that CT scan will show a bulging of the cavernous sinus, which, if present, is a helpful ancillary finding. Although echography, CT scan, and MR angiography are supportive of a carotid-cavernous intercommunication, neither technique demonstrates the actual location of the fistulous tract.
origin, high morbidity, guarded prognosis, and tricky management. The “Johnny-come-lately” spontaneous type has received less attention. In the latter, ultrasonography will show the dilated SOV and the enlarged extraocular muscles that usually occur, but echographic findings and clinical assessment are not always in agreement (Phelps et al., 1982). CT scan also shows the enlarged veins and the swollen muscles in the orbit (see Fig. 11.4A). The coronal scan is particularly useful in demonstrating the symmetrical thickening of the extraocular muscles unlike the asymmetric enlargement of extraocular muscles of Graves orbitopathy although this is not a constant finding. Some observers comment that CT scan will show a bulging of the cavernous sinus, which, if present, is a helpful ancillary finding. Although echography, CT scan, and MR angiography are supportive of a carotid-cavernous intercommunication, neither technique demonstrates the actual location of the fistulous tract.
Although MRI is proving useful in the evaluation of carotid-cavernous vascular disorders, angiography is still the premier choice for the accurate study of carotid-cavernous fistulas. The relationship and location of the small meningeal vessels communicating with the cavernous sinus are best delineated by selective (separate) injection of the internal and external carotid arterial systems with supplementary subtraction display. Otherwise, some of the smaller caliber communications may not be visualized. Even in the latter event, selective angiography will visualize the dilated venous channels that drain the communication. The importance of injecting the internal and external carotid arteries separately was driven home by the finding of an indirect left carotid-cavernous fistula with drainage through the right SOV. The patient had the clinical findings of a right-sided fistula but only an outside angiogram performed on the right carotid artery was normal. The answer was
revealed when the left internal carotid artery was injected.
revealed when the left internal carotid artery was injected.
The present role of MRI is ancillary to arteriography. MRI can serially assess the evolution of thrombosis of the draining venous channel, which may occur either during the clinical course or following therapeutic embolization. In either case, MRI replaces the need for a second angiogram that once was necessary in the follow-up evaluation of the patient. Normally, with MRI there is an absence of signal “flow void” from patent venous channels. When thrombosis occurs, the flow void of the affected venous channel will be replaced by a signal of some intensity, the latter being proportional to the degree of thrombosis (Fig. 11.4B). In the stage of recanalization of a thrombus, the reverse of this signal sequence will occur (Macchi et al., 1986).
The recent development of color Doppler imaging of the orbit may also play an increasing role in both diagnosis and tracking of low-flow fistulas. Flaherty et al. (1991) describe their experience with this modality in two patients with this type of vascular malformation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree