History of present illness
A 44-year-old mildly symptomatic woman is referred for a “swollen retina” and vision that cannot be corrected better than 20/30 in her left eye. She has a past ocular history significant for high myopia. She is a frequent contact lens wearer, although dry eyes made her intolerant to contact lenses, and she underwent phakic intraocular lens (IOL) surgery in each eye 2 years earlier.
Ocular examination findings
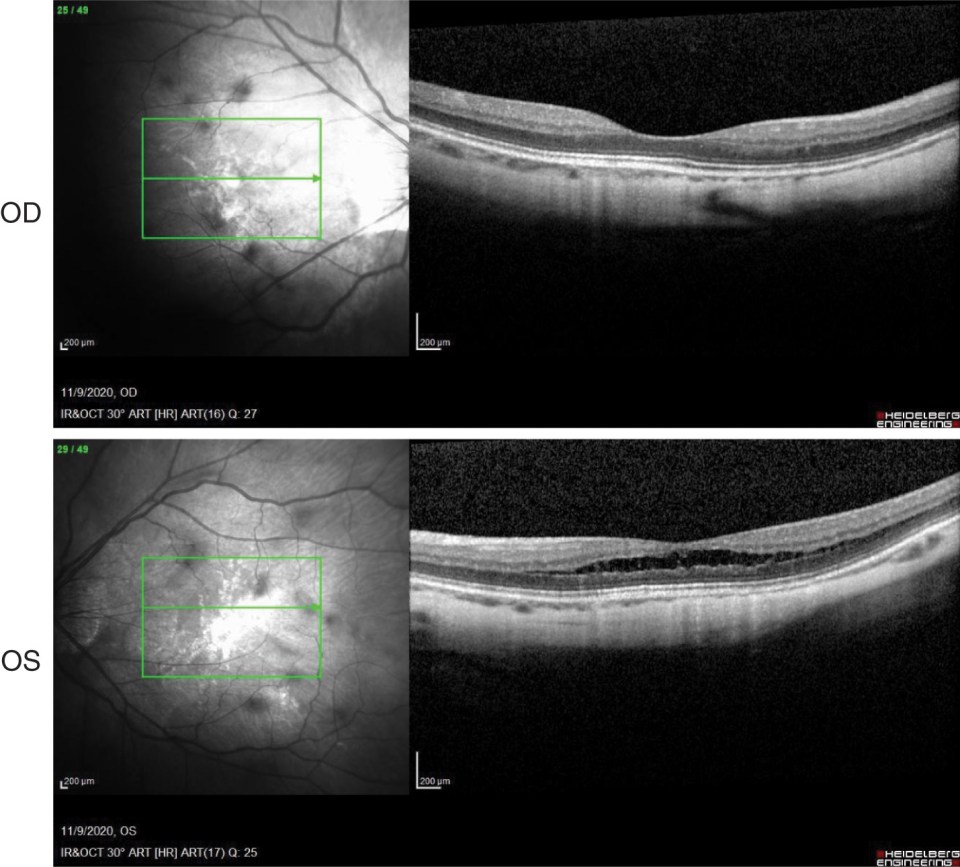
Visual acuities with correction were 20/20 in the right eye and 20/30 in the left eye. Intraocular pressures were normal. Anterior segment examination showed bilateral phakic IOL and symmetrical mild nuclear sclerotic cataracts but otherwise was unremarkable. Dilated fundus examination of the right eye showed a myopic, tilted optic nerve with peripapillary atrophy. The right macula showed some mild hypopigmentation. Dilated fundus examination of the left eye showed a slightly myopic, tilted optic nerve. The left macula showed pigment mottling consistent with myopic macular degeneration ( Fig. 14.1 ).

Imaging
Optical coherence tomography (OCT) of the right eye was normal for a myopic eye. OCT of the left eye showed intraretinal cyst-like changes in the outer retina (outer plexiform and outer nuclear layers) in the foveal and parafoveal regions. The foveal contour was irregular, but there was no epiretinal membrane ( Fig. 14.2 ).
Questions to ask
- ■
What is the patient’s refractive error? Myopic foveoschisis should be considered in the differential diagnosis for retinoschisis.
- ■
Refraction before phakic IOL surgery was −28.50 − 0.75 × 153 in the right eye and −29.50 − 0.25 × 009 in the left eye
- ■
- ■
Does the patient have a family history of ocular conditions or consanguinity? A family history would be important to ascertain etiologies for retinoschisis such as congenital juvenile X-linked retinoschisis (CXLR), retinitis pigmentosa, or familial internal limiting membrane dystrophy.
- ■
No
- ■
- ■
Does the patient have a history of trauma? Trauma has been associated with macular retinoschisis.
- ■
No
- ■
- ■
What medications does the patient take? Medications such as niacin and taxanes can cause cystic macular edema that appears similar to retinoschisis.
- ■
None
- ■
Assessment
- ■
This is a case of a 44-year-old woman with a past ocular history of high myopia and bilateral phakic IOL surgery demonstrating unilateral myopic macular schisis of mainly the foveal and parafoveal areas on OCT.
Differential diagnosis
- ■
CXLR
- ■
Stellate nonhereditary idiopathic foveomacular retinoschisis
- ■
Myopic choroidal neovascularization
- ■
Pseudophakic cystoid macular edema
- ■
Epiretinal membrane
- ■
Lamellar macular hole
- ■
Degenerative retinoschisis
- ■
Medication-associated retinoschisis (niacin, taxanes)
- ■
Traction retinal detachment
Working diagnosis
- ■
Myopic macular schisis (also called myopic foveoschisis) in a highly myopic patient
Multimodal testing and results
- ■
Fundus photos
- ■
On fundus examination, characteristic findings of high myopia can be seen, but the intraretinal cystic spaces typically cannot be appreciated.
- ■
Features typical of degenerative myopia, including chorioretinal atrophy, peripapillary atrophy, posterior staphyloma, and lacquer cracks, may or may not be seen.
- ■
- ■
OCT
- ■
As mentioned, OCT of the left eye showed cyst-like changes in the outer retina in the foveal and parafoveal regions along with an irregular foveal contour, even in the absence of any epiretinal membrane.
- ■
The diagnosis of myopic macular schisis is almost impossible without OCT.
- ■
- ■
Fluorescein angiography (FA)
- ■
FA does not show any late leakage or petaloid hyperfluorescence in the macula.
- ■
Management
- ■
Given that this patient was mildly symptomatic with visual acuity of 20/30 in the affected eye, the patient was observed.
- ■
This condition has also been called myopic traction maculopathy, which is a misnomer. There are no tractional membranes present on the retinal surface. The condition does not respond well to vitrectomy with internal limiting membrane peel, and this intervention is associated with complications because of the severity of the myopia in most cases and should be avoided in eyes with good vision.
- ■
Patients generally maintain a stable OCT appearance and relatively good and stable visual acuity for many years.
Follow-up care
- ■
There are no previously established guidelines for follow-up.
- ■
Our patient is followed on an annual basis. Vision and OCT in the left eye have been unchanged ( Fig. 14.3 ).





