Purpose
Ultraviolet-B (UV-B) radiation can cause phototoxic macular injuries in young people who have been sunbathing but not sungazing and in welders. Welders have a reportedly increased risk of uveal melanoma. We analyze phakic and pseudophakic risks for solar and welding arc UV-B exposure.
Design
Optical radiation measurement, analysis, and perspective.
Methods
Spectral transmittances were measured for UV-transmitting, UV-blocking, and blue-blocking intraocular lenses (IOLs). The photoprotective performances of crystalline and intraocular lenses were analyzed using relevant epidemiologic and laboratory data and action spectra for acute retinal phototoxicity and melanoma photocarcinogenesis.
Results
Crystalline lens UV-B retinal protection is deficient in children and young adults, increasing their potential susceptibility to acute retinal phototoxicity and hypothetical photomelanomagenesis. UV-B radiation has sufficient energy/photon to induce primary melanomagenic DNA lesions, unlike blue light or UV-A radiation. UV-blocking and blue-blocking IOLs have negligible UV-B transmittance. UV-transmitting IOL transmittance of UV-B radiation is equivalent to that of a 15-year-old crystalline lens.
Conclusions
If optical radiation exposure is responsible for welders’ increased risk of uveal melanoma, then UV-B radiation is the most probable causative agent and spectacle wear is a potential confounding factor in epidemiologic studies of ocular melanoma. Welders under 30 years of age are at greater risk for welding maculopathy than older welders. Children, adults under 30 years of age, and pseudophakic individuals with UV-transmitting IOLs should wear sunglasses in bright environments because of the UV-B window in their crystalline lenses or IOLs.
Ultraviolet (UV) radiation and visible light can cause photochemical retinal damage, also known as retinal phototoxicity or photic retinopathy. International safety standards for photic retinopathy are based on photosensitizer-type retinal phototoxicity mediated primarily by lipofuscin in the retinal pigment epithelium (RPE). Phototoxicity decreases with increasing wavelength, so UV-B radiation is more hazardous than UV-A radiation. Similarly, UV radiation is more hazardous than violet light, which is more hazardous than longer-wavelength blue light.
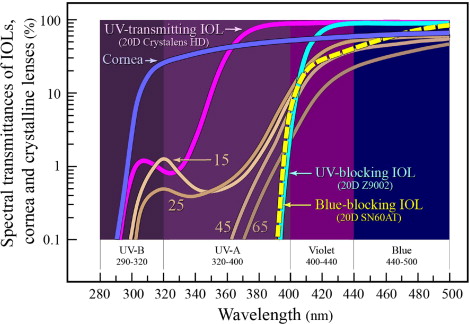
The Table summarizes the optical radiation bands potentially involved in retinal phototoxicity or photocarcinogenicity. Figure 1 presents the spectral dependence of photosensitizer-type retinal phototoxicity in comparison to 1) photokeratitis and mammalian cell mutagenicity and 2) photopic, scotopic, and circadian photoreception. Figure 2 shows the protection afforded by the cornea and by crystalline lenses of different ages. In general, the cornea completely blocks UV radiation below 300 nm. The crystalline lens protects the retina from most UV-B (280–320 nm) and UV-A (320–400 nm) radiation, but crystalline lenses under 30 years of age transmit potentially harmful UV-B radiation to the retina.
| Optical Radiation Band | Wavelengths | Clinical Relevance |
|---|---|---|
| UV-C | 100–280 nm | The cornea completely blocks UV-C radiation. |
| UV-B | 280–320 nm | The cornea transmits UV radiation wavelengths longer than 300 nm. UV-B has the greatest potential retinal phototoxicity and choroidal photocarcinogenicity. UV-B radiation is fully absorbed by crystalline lenses over 30 years of age, as well as by UV-blocking and blue-blocking IOLs. Crystalens IOLs and young crystalline lenses do transmit a small but potentially significant amount of this hazardous radiation to the retina. |
| UV-A | 320–400 nm | UV-A radiation is responsible for two-thirds of the potential acute UV-blue phototoxicity in a pseudophakic eye. UV-A radiation passes through the cornea but crystalline lens absorption prevents most of it from reaching deeper ocular structures. UV-blocking and blue-blocking IOLs also screen the retina from UV-A radiation that passes through UV-transmitting IOLs. |
| Violet light | 400–440 nm | Violet light is responsible for 18% of potential acute UV-blue phototoxicity in a pseudophakic eye. It provides 10% of scotopic, 28% of circadian, and 62% of S-cone photoreception for an isoilluminance source. |
| Blue light | 440–500 nm | Blue light is responsible for only 14% of potential acute UV-blue phototoxicity in a pseudophakic eye. It provides 35% of scotopic, 55% of circadian, and 32% of S-cone photoreception for an isoilluminance source. |
| Violet & blue light (short-wavelength visible light) | 400–500 nm | Neither violet nor blue light has adequate energy per photon to cause the direct DNA damage responsible for photomelanomagenesis. Violet and blue light combined provide 45% of scotopic, 83% of circadian, and 94% of S-cone photoreception for an isoilluminance source. Blue-blocking IOLs eliminate 43% to 57% of this violet and blue light, depending on their dioptric power, accounting for their inferior photopic, scotopic, and circadian photoreceptive performance in comparison to UV-blocking IOLs. |
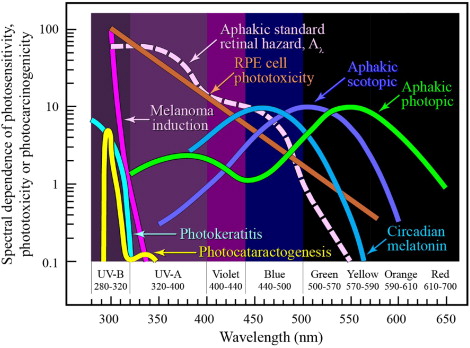
Solar and welding arc maculopathy and operating microscope and endoilluminator injuries are the only common retinal syndromes of proven phototoxic origin. Photocarcinogenesis differs from retinal phototoxicity because it involves primarily UV-B radiation damage to DNA molecules, a mechanism quite different from the retinal cell apoptosis involved in photopigment-mediated or photosensitizer-mediated photic retinopathies.
Intraocular and Crystalline Lens Transmittance
UV-transmitting, UV-blocking, and blue-blocking intraocular lenses (IOLs) are all widely used today, 30 years after the recognition that early polymethylmethacrylate IOLs transmitted UV radiation to the retina. Polymers in IOL optics are opaque to UV radiation below 250 nm, but chromophores are needed to block UV-B radiation completely or significantly attenuate longer-wavelength optical radiation. UV-transmitting IOLs have no additional chromophores, but colorless benzophenone or benzotriazole chromophores are added to UV-blocking IOL polymers to eliminate most UV radiation and possibly some violet light. Additional yellow dyes are bound to optic polymers in blue-blocking IOLs to eliminate substantial amounts of violet and blue light.
Spectral transmittances between 200 and 1100 nm were measured for UV-transmitting (Crystalens HD 20 diopter [D]; Bausch and Lomb Inc., Rochester, New York, USA), UV-blocking (Z9002 Tecnis 20D; Abbott Medical Optics, Santa Ana, California, USA), and blue-blocking (AcrySof SN60AT 20D; Alcon Inc., Fort Worth, Texas, USA) IOLs with a Beckman-Coulter DU 800 UV/Visible microcomputer-controlled spectrophotometer (Beckman-Coulter, Fullerton, California, USA). Spectra are shown in Figure 2 .
Maximal crystalline lens UV-B transmittance is only around 1.33% for a 15-year-old, but UV-B radiation is probably responsible for solar maculopathy without sungazing in young people and in young military personnel in tropical environments. Henle-layer fiberoptic transmission increases with decreasing wavelength, potentially increasing foveolar UV-B irradiance. It is also the likely cause of any increased risk of uveal melanoma in welders, if that increased risk is associated with optical radiation exposure.
The UV-B window in the crystalline lens closes by roughly 30 years of age as age-related increased short-wavelength crystalline lens absorption blocks transmission of essentially all UV-C and UV-B radiation. As shown in Figure 2 , UV-blocking and blue-blocking IOLs attenuate all UV-B and even more UV-A radiation than crystalline lenses. Conversely, UV-transmitting IOLs transmit roughly the same amount of UV-B radiation as teenage crystalline lenses: 1.19% at 310 nm and 0.85% at 320 nm for UV-transmitting IOLs versus 0.75% at 310 nm and 1.33% at 320 nm for 15-year-old crystalline lenses.
Optical Radiation and Melanoma
Epidemiologic, genetic, and biological studies implicate solar UV radiation as a cause of cutaneous melanomas, but this association is much weaker than that of basal and squamous skin cancers. Cutaneous melanomas can occur at locations receiving only minimal, intermittent solar exposure (eg, the backs, lower legs, and soles of indoor workers), whereas basal and squamous cell carcinomas occur at sites with the highest total cumulative solar UV irradiation (eg, the faces of farmers or sailors).
UV-B is overwhelmingly responsible for the primary DNA lesions in non-ionizing radiation–induced melanoma oncogenesis (cyclobutane pyrimidine dimers and pyrimidine [6-4] pyrimidone photoproducts) whose aberrant repair causes mutations, but UV-A radiation can also produce potentially mutagenic oxidative DNA damage. The incidence of cutaneous melanoma depends on skin color and geographic region. It is uncommon in darker-skinned people and most common in Australia.
Mutations from DNA damage initiate melanoma oncogenesis. Skin cancer incidence rises exponentially with age because of 1) progressively increasing time available for tumor initiation, promotion, and progression, and 2) progressively decreasing DNA repair capability. Some evidence suggests that sunlight may not be a significant risk factor in cutaneous melanoma, including the absence of demonstrable dose-response curves in epidemiologic studies, variability in correlations of incidence with geographic latitude, and tumor development at sites not exposed to solar radiation.
Optical Radiation and Melanoma
Epidemiologic, genetic, and biological studies implicate solar UV radiation as a cause of cutaneous melanomas, but this association is much weaker than that of basal and squamous skin cancers. Cutaneous melanomas can occur at locations receiving only minimal, intermittent solar exposure (eg, the backs, lower legs, and soles of indoor workers), whereas basal and squamous cell carcinomas occur at sites with the highest total cumulative solar UV irradiation (eg, the faces of farmers or sailors).
UV-B is overwhelmingly responsible for the primary DNA lesions in non-ionizing radiation–induced melanoma oncogenesis (cyclobutane pyrimidine dimers and pyrimidine [6-4] pyrimidone photoproducts) whose aberrant repair causes mutations, but UV-A radiation can also produce potentially mutagenic oxidative DNA damage. The incidence of cutaneous melanoma depends on skin color and geographic region. It is uncommon in darker-skinned people and most common in Australia.
Mutations from DNA damage initiate melanoma oncogenesis. Skin cancer incidence rises exponentially with age because of 1) progressively increasing time available for tumor initiation, promotion, and progression, and 2) progressively decreasing DNA repair capability. Some evidence suggests that sunlight may not be a significant risk factor in cutaneous melanoma, including the absence of demonstrable dose-response curves in epidemiologic studies, variability in correlations of incidence with geographic latitude, and tumor development at sites not exposed to solar radiation.
Uveal Melanoma Epidemiology and Etiopathogenesis
Epidemiologic and biological evidence linking UV radiation from sunlight exposure to the etiopathogenesis of uveal melanoma is at best weak and contradictory. Uveal melanoma has a mean, age-adjusted incidence of 4.3 per 1 million people in the United States. Mean age at diagnosis is 58 years, but 1% of melanomas occur in individuals under 20 years of age. Incidence begins to rise in the third decade of life, peaking around at 70 years of age (∼20 per 1 million people or 0.002%), and then declines. Age-related increase in tumor incidence is found in most cancers, attributable in part to the age-associated loss of DNA repair capability. Decline in cancer incidence in the very elderly is found in most routinely screened cancers, possibly attributable to decreased disease ascertainment in older people.
One epidemiologic study showed that solar exposure predicts the risk of uveal melanoma in Australia. A multinational study, however, found no association between occupational sunlight exposure and the risk of uveal melanoma. Studies on anatomic patterns of choroidal melanomas have also produced conflicting results concerning solar exposure’s hypothetical role in the etiopathogenesis of uveal melanoma. N-ras mutations correlated with sunlight exposure are absent in uveal melanomas. Light iris and skin color have been found to be risk factors for uveal melanoma.
The incidence of uveal melanoma decreases with decreasing latitude (the equator’s latitude is 0) and increasing solar exposure. This inverse relationship between sunlight and the incidence of ocular melanoma exists in European populations where pigmentation increases at lower latitudes, but it is also present in non-Hispanic, more uniformly pigmented, white North American populations.
The inverse relationship between sunlight exposure and the incidence of uveal melanoma cannot support a causal relationship between optical radiation and the oncogenesis or proliferation of uveal melanomas unless other factors are taken into consideration, such as 1) the anti-oncogenic benefits of sunlight-induced vitamin D production found to reduce non–skin cancer mortality, 2) the protective effects of increased uveal pigmentation, and 3) the immune benefits of higher environmental retinal illuminances that produce robust circadian rhythms. Darker eyes may have increased antioxidant, free-radical-scavenging, and light-absorptive effects attributable to denser melanin. Additionally, structural differences between melanin in darkly and lightly pigmented eyes may produce predominantly antioxidant and pro-oxidant properties, respectively. In summary, the present medical literature “does not support a significant role for sunlight—which includes blue light—in the oncogenesis of uveal melanoma.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


