Purpose
To quantify and describe practically a novel technique for donor tissue preparation in Descemet stripping endothelial keratoplasty to approach the superior visual outcomes of Descemet membrane endothelial keratoplasty.
Design
Experimental laboratory investigation.
Methods
setting: Institutional. study population: Eleven human donor corneas. intervention: Double-pass of microkeratome over donor corneas—first with a thicker cutting depth and subsequently with a thinner cutting depth.
Main Outcome Measures
Donor tissue profiles and residual bed thicknesses.
Results
After the first pass of the microkeratome, the average cut thickness using the 250-μm cutting head was 342.5 ± 14.8 μm (range, 332 to 353 μm), that using the 300-μm head was 343.8 ± 39.2 μm (range, 315 to 411 μm), and that with the 350-μm head was 467.7 ± 50.1 μm (range, 419 to 519 μm). We used the 200-μm cutting head only once with a cut depth of 210 μm. For the second pass, when using the 110-μm head, the cutting depth averaged to 167.8 ± 28.8 μm (range, 133 to 203 μm). The 130-μm cutting head yielded a cut depth of 199.7 ± 24.4 μm (range, 180 to 227μm). Two corneas were perforated during the second pass. The average final thickness of the residual bed was 121 ± 32.2 μm (range, 52 to 160 μm).
Conclusions
Double-pass harvest for ultra-thin Descemet stripping automated endothelial keratoplasty could improve optical outcomes by obtaining donor Descemet stripping automated endothelial keratoplasty tissue with thinner residual beds. Further studies are needed with larger sample sizes to establish algorithms for appropriate cutting head thickness in each pass. Potential additional endothelial cell loss with the second pass of the microkeratome also should be evaluated.
Descemet stripping endothelial keratoplasty and Descemet stripping automated endothelial keratoplasty (DSAEK) have become the new standards for endothelial transplantation. Although good visual outcomes are obtained, the issues of optical aberration from stromal interface haze and postoperative hyperopia remain. Descemet membrane endothelial keratoplasty (DMEK) presents as an upgrade to DSAEK with improved visual outcomes related to the absence of transplanted stroma. Currently, the harvest and manipulation of the donor Descemet membrane and endothelium in DMEK is technically difficult because of the thin nature of the tissue and its tendency to scroll.
This pilot study investigated a new method to obtain thin, uniform stromal tissue overlying Descemet membrane and endothelium for endothelial keratoplasty using 2 passes of the microkeratome. At present, the standard approach for DSAEK tissue harvest uses a single microkeratome pass, typically with a 300- to 350-μm cutting depth. Alternatives to the current DSAEK harvest technique include minimizing the thickness of stroma overlying the central Descemet membrane and endothelium with a peripheral rim of stromal tissue, permitting facile manipulation of the donor tissue. Our new proposed technique permits reproducible and facile harvest of donor tissue to allow future clinical implementation to assess potential improved visual outcomes with less induced hyperopia.
Methods
Eleven human corneoscleral rims donated for research (Utah Lions Eye Bank, Salt Lake City, Utah, USA) were mounted in an artificial anterior chamber (ALTK System; Moria/Microtech, Doylestown, Pennsylvania, USA). All corneas were harvested uniformly by in situ excision and were place immediately into the Optisol (Bausch & Lomb, St Louis, Missouri, USA) medium when harvested; therefore, the death-preservation time was the same as death-retrieval time. The anterior chamber was filled with Optisol GS to maintain an applanation pressure of approximately 80 mm Hg measured using a Reichert Tono-Pen applanation tonometer (Depew, New York, USA). Central corneal thickness (CCT) was measured using an ultrasound pachymeter (Pachette 2; DGH Technology, Exton, Pennsylvania, USA) and averaging 3 readings. Anterior segment optical coherence tomography (AS OCT; Zeiss, Jena, Germany) imaging of the donor tissue was obtained by holding the artificial anterior chamber at the AS OCT imaging aperture ( Figure 1 ). Scans were performed across the 180-degree meridian, and thicknesses of the residual stromal bed (RSB) were measured at the center of the cornea and at 1-mm intervals away from the center across the 6-mm optical zone.

A Carriazo Barraquer microkeratome (Moria, Antony, France) with cutting head depths of 200 μm, 250 μm, 300 μm, or 350 μm were used to create the superficial free cap, and depths of 110 and 130 μm were used to obtain the intralamellar stromal lenticula. In general, the microkeratome head that represented 50% of the precut cornea was used for each cut to ensure adequate RSB. After each passage of the microkeratome, the residual bed thickness was imaged using AS OCT and CCT again was measured (see supplemental video at AJO.com ). Typically, ultrasound pachymetry could not be performed on very thin residual beds because of inadequate signal registration.
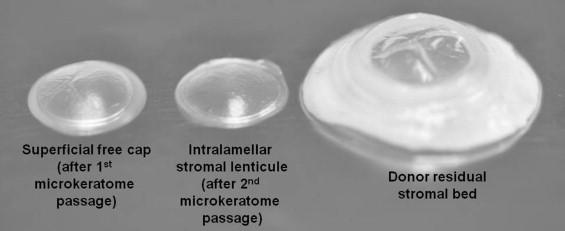
For illustrative purposes, photography of the superficial free cap, intralamellar stromal lenticula, and residual bed at ×4 magnification ( Figure 2 ) and histologic analysis with hematoxylin and eosin staining at ×20 magnification ( Figure 3 ) were obtained.

Results
The average age ± standard deviation of the 11 donors was 48.3 ± 17 years (range, 24 to 73 years). The average death to preservation time ± standard deviation was 7.4 ± 5 hours (range, 2.4 to 15.9 hours). The average storage time ± standard deviation was 23 ± 6.7 days (range, 10 to 31 days; Table ).
| Cornea No. | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| Age (y) | 41 | 24 | 44 | 61 | 44 | 24 | 42 | 73 | 73 | 63 | 42 |
| Time to preservation (h) | 4.3 | 7.7 | 15.9 | 2.4 | 15.9 | 7.7 | 10.8 | 3 | 3 | 3.1 | 10.8 |
| Storage time (d) | 10 | 28 | 18 | 16 | 18 | 28 | 23 | 29 | 29 | 31 | 23 |
| Initial CCT (μm) | 520 | 570 | 587 | 590 | 630 | 630 | 690 | 690 | 710 | 760 | 840 |
| Cutting depth head of first pass (μm) | 200 | 300 | 300 | 250 | 250 | 300 | 300 | 300 | 350 | 350 | 350 |
| Superficial free cap (μm) | 210 | 340 | 315 | 353 | 332 | 317 | 336 | 411 | 419 | 465 | 519 |
| Intermediate RSB (μm) | 310 | 230 | 272 | 237 | 298 | 313 | 354 | 279 | 291 | 295 | 321 |
| Cutting depth head of second pass (μm) | 130 | 110 | 130 | 110 | 110 | 110 | 110 | 130 | 110 | 110 | 130 |
| Intralamellar stromal cap (μm) | 180 | xx | xx | 133 | 138 | 203 | 196 | 227 | 171 | 166 | 192 |
| Final RSB (μm) | 130 | xx | xx | 104 | 160 | 110 | 158 | 52 | 120 | 129 | 129 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


