Purpose
To describe a technique that uses a transcorneal suture for safe delivery and fixation of donor tissue during Descemet stripping automated endothelial keratoplasty in patients that are at risk of graft dislocation into the vitreous cavity as a result of minimal or absent iris–lens diaphragm.
Design
Interventional case series.
Methods
Thirteen eyes with endothelial decompensation and inadequate iris–lens diaphragm underwent modified Descemet stripping automated endothelial keratoplasty surgery. A 10-0 Prolene suture (Ethicon Inc) was passed through the endothelial graft and used to pull the graft into the eye and anchor it onto the recipient cornea. Best-corrected visual acuity, refraction, and complications were recorded.
Results
Preoperative best-corrected visual acuity was less than 20/200 in all cases. Eleven patients had a pre-existing comorbidity (glaucoma, n = 8; previous retinal detachment, n = 2; epiretinal membrane n = 1). Average follow-up was 11.3 months (range, 3 to 36 months). No graft dislocation occurred during surgery. After surgery, graft detachment was noted in 2 cases and rebubbling succeeded in achieving reattachment. All patients had successful attachment of the endothelial graft. Postoperative best-corrected visual acuity improved in 11 of 13 patients and remained unchanged in 2 patients.
Conclusions
In patients with insufficient iris–lens diaphragm, this technique allowed safe graft delivery, prevented intraoperative and postoperative graft dislocation, and facilitated successful rebubbling in case of postoperative graft detachment.
Standard Descemet stripping endothelial keratoplasty (DSAEK) surgery involves stripping of Descemet membrane from the recipient cornea followed by the introduction of a posterior lamellar graft into the anterior chamber. The graft is usually delivered by means of an injector or via a pull-through technique using forceps or sutures. Once inside the eye, the donor tissue floats freely in the anterior chamber above the iris–lens diaphragm. Air is injected under the graft to fixate it against the recipient cornea. The air bubble is trapped in the anterior chamber by the iris–lens barrier. However, if such a barrier is partly or totally breached, the graft cannot be safely delivered because it may dislocate into the vitreous cavity during insertion or intraoperative manipulation. In addition, even if the surgeon succeeded in primarily attaching the donor tissue, the air can escape into the vitreous cavity after surgery, resulting in loss of the tamponading effect and risk of graft detachment and dislocation.
Suture and viscoelastic-assisted techniques have been described previously to aid DSAEK surgery in case of partial or total absence of the iris–lens barrier. We describe herein a modified technique that uses a transcorneal Prolene suture to allow safe graft delivery and anchoring onto the recipient cornea. This technique aims to eliminate the intraoperative and postoperative risk of posterior graft dislocation, while facilitating the management of postoperative graft detachment. The outcomes of this technique in 13 patients with endothelial decompensation and minimal or absent iris–lens diaphragm are reported.
Methods
This prospective study was undertaken in an institutional setting at the Department of Ophthalmology, Villa Serena Hospital, Forlì, Italy. Thirteen patients with corneal decompensation and minimal or absent iris–lens diaphragm were recruited into the study, which was aimed at evaluating the results of an anchoring transcorneal suture in DSAEK surgery. The diaphragm was deemed absent in the event of aphakia or when the plan was to leave the patients aphakic after surgery (ie, removal of anterior chamber intraocular lens [IOL]). Eyes with zonular dehiscence in the presence of a fixed mydriasis or an iris defect of 120 degrees or more (i.e., deemed unsuitable for pupilloplasty) were classified as having a minimal diaphragm.
Iridoplasty before DSAEK surgery was not feasible (iris defect ≥ 120 degrees, n = 5; iris atrophy with fixed pupil larger than 8 mm, n = 2), and IOL implantation was not believed to be beneficial (functionally monocular, n = 2; contralateral aphakia, n = 2; high-degree myopia, n = 2) for any of these patients. Patients were scheduled to be seen 1, 3, 6, and 12 months after surgery and annually thereafter. Data collected included patient demographics, preoperative and postoperative Snellen best-corrected visual acuity, preoperative and postoperative refraction, endothelial cell count, as well as note of any complications.
Surgical Technique
Intravenous droperidol 3 mL (7.5 mg) was administered immediately before peribulbar local anesthetic injection (50% mixture of 2% lidocaine and 0.5% bupivacaine) to achieve sedation. All procedures were performed by a single surgeon (M.B.)
Descemetorhexis and wound construction in the recipient eye was carried out as previously described. The endothelium of the donor corneoscleral tissue was coated with viscoelastic (IAL F; Bausch & Lomb, Inc, Rochester, New York, USA) and was placed on an artificial anterior chamber (ALTK System; Moria, Antony, France). Approximately two thirds of the anterior corneal stroma was removed using a 300-μm microkeratome head. The residual stromal bed was dried with a sponge, and a 9.0-mm circular marker dipped in trypan blue was used to outline the area of dissected stroma. An orientation mark was also made within the ring to confirm graft orientation and the donor button was punched to the desired size (range, 8.5 to 9.0 mm).
The ensuing steps are illustrated in Figure 1 and in the Supplemental Video . The graft then was placed on the conjunctiva with the stromal side up. Both arms of a 10-0 prolene suture (Ethicon Inc., Somerville, New Jersey, USA) with straight 16mm needles were passed through the peripheral edge of the donor button from the endothelial side and spaced approximately 1 mm apart.
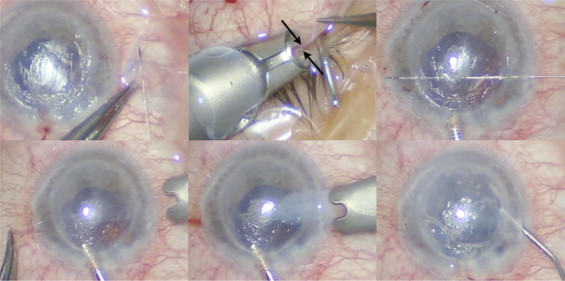
An anterior chamber maintainer was placed at the 12-o’clock position and the graft was mounted onto the Busin glide (Moria SA, Antony, France), with the endothelial side up. The 2 long needles of the Prolene suture were inserted through the nasal corneal tunnel and were passed across the anterior chamber exiting through the temporal recipient cornea. The exit points of the needles were located just anterior to the temporal paracentesis to aid rebubbling in case of graft detachment. The Busin glide was positioned adjacent to the nasal wound and the sutures were used to pull the graft into the anterior chamber. The graft was allowed to unfold spontaneously, and the anterior chamber maintainer was removed thereafter. When necessary, centration of the graft was achieved by gentle tapping on the corneal surface. The 9.0-mm ring and orientation mark allowed visualization of the graft, and on correct positioning, air was injected into the anterior chamber to attach the graft against the recipient stroma. The 2 ends of the suture were tied on the recipient corneal surface and the knot was buried. All clear corneal wounds were sutured airtight with 10-0 nylon sutures. A 30-gauge needle was used to inject air and to achieve a complete air fill. Four peripheral stab incisions were made in the recipient cornea down to the graft interface to release trapped fluid and to facilitate graft adherence.
Triamcinolone acetonide and gentamicin sulfate 0.3% was injected subconjunctivally at the end of the procedure. Patients were instructed to posture face up for 6 to 8 hours. After surgery, all patients received dexamethasone phosphate 0.1% and tobramycin sulphate 0.3% combination drops every 2 hours. The treatment was tapered gradually over 3 to 4 months to a single daily administration of dexamethasone phosphate 0.1% that was continued indefinitely. All sutures, including the prolene suture, were removed 4 toAll sutures, including the 6 weeks after surgery.
Results
Thirteen eyes of 13 patients (7 female, 6 male) were recruited. The mean patient age was 63.6 years (range, 34 to 82 years). Preoperative best-corrected visual acuity was 20/200 or worse in all cases. All eyes had some degree of iris–lens defect (aphakia, n = 8; pseudophakia [anterior chamber IOL], n = 2; pseudophakia [IOL in the capsular bag] with 120 degrees of zonular and iris defect, n = 1; pseudophakia [IOL in the capsular bag] with zonular defect and extreme mydriasis, n = 1; pseudophakia [IOL in the capsular bag] with zonular defect and 170-degree iris defect, n = 1), posing the risk of air and graft migration into the vitreous cavity. Anterior chamber IOLs were explanted from 2 eyes with a view to secondary implantation after endothelial transplantation. Eleven patients had a pre-existing comorbidity (glaucoma, n = 8; previous retinal detachment, n = 2; epiretinal membrane, n = 1). All patients had undergone a previous vitrectomy, either at the time of trauma, lens surgery, or retinal detachment repair.
Suture-assisted DSAEK was performed in all cases as described above, and no intraoperative complications were noted. Patients 6 and 9 (see the Table ) were noted to have endothelial graft detachment on the first postoperative day. Air had escaped into the vitreous cavity in both eyes. Rebubbling was performed through the paracentesis located immediately beneath the transcorneal suture, and successful attachment of the graft was achieved thereafter.
| Patient No. | Age (yrs) | Sex | Diagnosis | Iris Defect | Postoperative Lens Status | Preoperative BCVA | Postoperative BCVA | Donor ECC | Postoperative ECC | Follow-up (mos) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 45 | M | ABK, trauma | None | Aphakia | HM | HM | 2500 | 1897 | 6 |
| 2 | 34 | M | Decompensated PK, previous RD, trauma | 360° | Aphakia | HM | 1/200 | 2600 | 2232 | 3 |
| 3 | 75 | M | PBK, glaucoma | Peripheral 30° | Aphakia | < 20/200 | < 20/200 | 2400 | 1668 | 6 |
| 4 | 48 | F | ABK, congenital cataracts, glaucoma | None | Aphakia | 1/200 | 20/50 | 2700 | 1882 | 24 |
| 5 | 82 | M | AC IOL, ERM | None | Aphakia | 1/200 | 20/60 | 2800 | 1518 | 12 |
| 6 | 76 | F | ABK, glaucoma | None | Aphakia | 20/200 | 20/30 | 2600 | 2189 | 3 |
| 7 | 78 | F | Trauma | Sectoral 120° | Aphakia | 20/200 | 20/30 | 2400 | 2112 | 24 |
| 8 | 80 | F | AC IOL, glaucoma | None | Aphakia | HM | 20/100 | 2500 | 2232 | 3 |
| 9 | 65 | M | PBK, previous RD, trauma | Fixed mydriasis | Pseudophakic zonular dehiscence | HM | 20/200 | 2700 | 1309 | 18 |
| 10 | 72 | F | Decompensated PK, glaucoma | Sectoral 150° | Aphakia | 20/400 | 20/100 | 2600 | 2157 | 3 |
| 11 | 53 | M | PBK, glaucoma, microphthalmos | Sectoral 100°, fixed mydriasis | Aphakia | < 20/200 | 20/100 | 2500 | 1697 | 36 |
| 12 | 64 | F | PBK, glaucoma | Sectoral 120° | Pseudophakic zonular dehiscence | 1/200 | 20/40 | 2500 | 1650 | 6 |
| 13 | 55 | F | Decompensated PK, glaucoma, trauma | Sectoral 170° | Pseudophakic zonular dehiscence | 20/200 | 20/100 | 2300 | 1876 | 3 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


