This article presents a current view of training in neurorhinology and focuses on the level of evidence for the clinical question of “how many cases are needed to achieve proficiency in endoscopic endonasal skull base surgery?” The authors discuss what defines surgical proficiency, what makes up the learning curve and how it shifts with increasing experience, comparisons of learning curves for different skull base surgeries, and conclude with a discussion and recommendations for achieving high-level proficiency.
| EBM Question | Level of Evidence | Grade of Recommendation |
|---|---|---|
| How many cases are needed to achieve proficiency in endoscopic endonasal skull base surgery? | 4 | C |
What is the definition of surgical proficiency? A proficient surgeon can be defined as one who is “competent or skilled in doing or using something.” The road to proficiency is a progression through 5 stages: novice, advanced beginner, competent, proficient, and expert. Not all surgeons reach this level and few will achieve expert status. There are multiple potential obstacles to the achievement of proficiency by a surgical team. Of these, the volume of cases is probably the most important factor, and will establish the length of the learning curve.
Learning curve
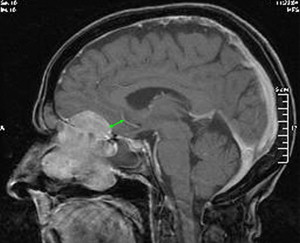
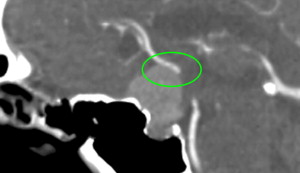
Endoscopic endonasal surgery has a long learning curve that is attributable to multiple factors: unfamiliar endoscopic anatomy, lack of endoscopic skills, potential risk of neural and vascular injury, and reconstructive challenges. The learning curve must deal with issues of endoscopic anatomy, instrumentation, 2-dimensional visualization, team dynamics, and dealing with complications. An incremental training plan has been proposed that is applicable to both otolaryngologists and neurosurgeons performing endonasal skull base surgery ( Table 1 ). The levels are based on level of technical difficulty, potential risk of vascular and neural injury, and unfamiliar endoscopic anatomy. Levels I to III are extradural procedures. Most pituitary surgeons will be between levels III and IV. Levels IV and V are intradural procedures and require a greater level of anatomic knowledge, surgical finesse, and teamwork. Level IV is further divided into pathology that has a cuff of cortical brain tissue between the tumor and the cerebral vasculature ( Fig. 1 ). Absence of a cortical cuff ( Fig. 2 ) increases the risk of vascular injury and may prevent complete tumor removal. Mastery of each level is recommended before attempting procedures at a higher level.
| Level | Description | Examples |
|---|---|---|
| I | Sinus surgery | Endoscopic sphenoethmoidectomy Sphenopalatine artery ligation |
| II | Advanced sinus surgery Basic skull base surgery | Endoscopic frontal sinusotomy Cerebrospinal fluid leaks Lateral recess sphenoid Sella/pituitary (intrasellar) Medial orbital decompression |
| III | Extradural skull base | Sella/pituitary (extrasellar) Optic nerve decompression Transodontoid approach (extradural) Transclival approaches (extradural) Petrous apex (medial expansion) |
| IV |
| Petrous apex (exposure of carotid) Transplanum approach (intradural) Craniofacial resection Transclival approaches Transodontoid approach (intradural) Suprapetrous carotid approach |
| V | Coronal plane Vascular dissection | Infrapetrous carotid approach Parapharyngeal space Aneurysms Vascular malformations Highly vascular tumors |
Before examining the limited data regarding the learning curve for endonasal skull base surgery, it is instructive to review the extensive literature regarding the learning curve for endoscopic cholecystectomy. Following the application of laparoscopic techniques to gallbladder surgery, there was a large spike in complications such as common bile duct injury that gradually returned to baseline as the surgical community gained more experience. Possible predictors of surgical expertise included proficiency in traditional techniques, endoscopic experience with other procedures, duration of practice, and number of cases performing a specific procedure. Of these, only the number of cases performing a specific procedure was significant. Various investigators have suggested that the threshold of proficiency is 25 to 30 cases for laparoscopic fundoplication and 15 to 20 cases for laparoscopic cholecystectomy. Whether these numbers could be applied to other endoscopic procedures is not known.
In skull base surgery, one can also look at microscopic surgeries that require a similar level of expertise to gain insight about the learning curve. Moffat and colleagues looked at facial nerve outcomes in vestibular schwannoma surgery. In 300 consecutive surgeries, postoperative facial nerve function was House grades I to III in 52% of the first 50 cases and 78% of the second 50 cases. Functional preservation continued to improve at a slower rate with 92% House grades I to III in the last 50 cases. Most of the learning curve was associated with the translabyrinthine approach.
Evidence-based review
A PubMed review of the medical literature was performed using the search terms “learning curve, skull base” and “learning curve, cranial base.” Article selection was restricted to the period 1996 to 2010. Guidelines established by the Oxford Center for Evidence-Based Medicine levels of evidence were used to grade the publications.
Specific data regarding endoscopic endonasal skull base surgery is limited and deals primarily with pituitary surgery ( Table 2 ). Most surgical teams have evaluated their experience as they transitioned from microscopic to endoscopic pituitary surgery. Sonnenburg and colleagues investigated the learning curve in their first 45 endoscopic pituitary surgeries. The series of patients was divided into 3 cohorts of 15 patients each and outcomes such as complication rates, blood loss, length of stay, and histology within each group were compared [level of evidence: IV]. Because there was no difference between the groups, they concluded that there was “no learning curve.” Their study, however, did not account for the complexity of cases, extent of resection, or experience of the neurosurgeon. In a study by Leach and colleagues, patients undergoing endoscopic pituitary surgery were divided into two consecutive groups of 53 and 72 patients [level of evidence: IV]. A comparison of the two time periods demonstrated that outcome measures (operative time, improvement in vision, remission of Cushing disease, and length of stay) were better in the second group. There was no change in the incidence of postoperative hypopituitarism. This study would suggest that proficiency is achieved after approximately 50 surgeries.



