Purpose
To evaluate the long-term effectiveness of improved ocular alignment using a suture/T-plate anchoring platform system.
Design
Retrospective, noncomparative, interventional case series.
Methods
setting: Institutional. study population: Seven consecutive patients with large angle deviations attributable to paralytic and/or restrictive strabismus managed jointly by orbital and strabismus surgeons. intervention procedure: The T-plate base is anchored to the orbital rim with the shaft projecting toward the orbital apex to simulate the origin of the affected muscle. A nonabsorbable suture serves as the coupling element linking the muscle insertion to the tip of the T-plate such that the suture coincides with the axis of the dysfunctional muscle and yields a pull vector to simulate the passive tensile force of the muscle. Information analyzed included patient demographics, etiology of strabismus and characteristics, prior muscle surgeries, secondary interventions, subjective appraisal of diplopia, and final ocular alignment measurements. main outcome measures: Subjective appraisal of diplopia, final ocular alignment in primary gaze, and late stability.
Results
All 7 patients showed marked reduction in ocular deviation with a median change of 33 prism diopters (PD) and a range of 7 to 72 PD. For the 6 patients with medial rectus dysfunction, the final ocular alignment ranged from 6 to 18 PD of residual exotropia in primary gaze. The patient with sixth nerve palsy had 5 PD of residual esotropia. There were no failures after an average of 59.4 months of follow-up.
Conclusions
A globe tethering technique using a suture/titanium T-plate anchoring platform system effectively treats refractory cases of paralytic and restrictive strabismus with large angles of deviation.
Paralytic strabismus associated with third and sixth nerve palsy or medial rectus muscle injury causes severe visual debilitation and poses formidable therapeutic challenges. The management principle is to rebalance the unequal and unopposed forces of the antagonist muscles on the globe. The principal surgical aims, regardless of the procedure employed, are to improve ocular alignment, reduce or eliminate diplopia, and provide a functional field of single vision in or near primary gaze.
Conventional recess-resect procedures often result in recurrent deviation, even with aggressive rectus recession. Conventional extraocular muscle procedures performed within the muscle cone often produce unsatisfactory long-term success because of compensatory antagonist muscle changes in the absence of counterbalancing adducting forces.
Various non-extraocular muscle-based methods have been devised to create an opposing mechanical restriction to balance the active contractile force of the antagonist muscle. These techniques typically passively tether the globe in a fixed primary position with permanent sutures, alloplastic materials, nonvascularized and vascularized autogenous tissues, or tendon to a fixation point outside the muscle cone on the side of the affected muscle. The most common fixation structure is the periosteum or bone. The long-term effectiveness of these indirect techniques depends on both the tensile strength and durability of the connecting and anchoring materials or tissues.
The 2 potential points of failure in the globe tethering model are the connecting element to the muscle insertion and the tension-bearing anchoring point. To overcome these 2 problems, we devised a suture/T-plate fixation platform system to allow for a more physiological pull vector that better simulates the passive tensile forces of a rectus muscle. We sought to determine the efficacy and long-term stability of our suture/T-plate fixation technique.
Methods and Materials
The clinical records of all patients undergoing suture/T-plate fixation for correction of complex strabismus from January 2003 to December 2007 were retrieved from the Medical Records Department of the Bascom Palmer Eye Institute.
Information analyzed included gender, patient age at diagnosis, etiology of strabismus and characteristics, prior muscle surgeries, pre- and post-T-plate insertion interventions, subjective appraisal of diplopia, and final ocular alignment measurement. Suture placement and T-plate fixation were performed by 1 orbital surgeon (D.T.T.) and postoperative suture adjustment was performed by 2 strabismus surgeons (C.A.M., H.C.). All ocular alignment measurements were obtained by 2 strabismus surgeons (C.A.M., H.C.). The final ocular alignment measurement in each patient was obtained while the antagonist muscle was devoid of any botulinum toxin type A influence, at least 6 months from the last injection. The duration of evaluation was measured from the surgery date of T-plate insertion to the most recent follow-up examination.
Surgical Technique
All procedures were performed under general anesthesia. Figure 1 depicts the concept of the suture/T-plate anchoring system. The T-plate is housed in the medial or lateral subperiosteal space for treatment of exotropia or esotropia, respectively.
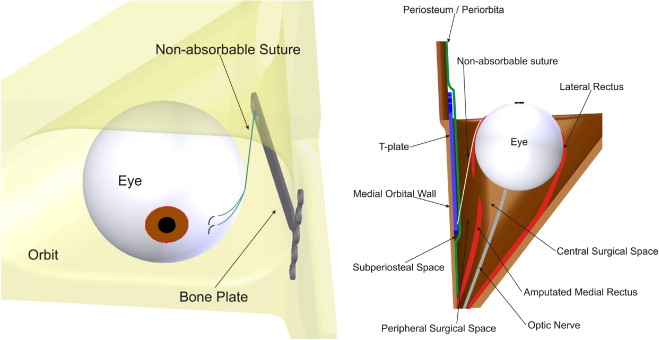
For medial rectus paresis, the crossbar of the T-plate is anchored to the nasal bone anterior to the anterior lacrimal crest while the shaft of the T-plate passes over the superior margin of the lacrimal sac fossa. The shaft is oriented along the same anterior-posterior axis and plane as the affected rectus muscle. The tip of the T-plate extends to the medial mid-orbit such that the shaft is situated below the frontoethmoidal suture line, away from the anterior and posterior ethmoidal arteries. For suture placement, a fornix-based medial conjunctival peritomy is made to delineate the medial rectus insertion. The extraocular muscle is not detached from its insertion. Orbital dissection is conducted in the peripheral surgical space, the compartment between the medial surface of the medial rectus muscle and the periorbita.
To illustrate the steps of this procedure, the surgical technique used to correct a large-angle exotropia attributable to complete left third nerve palsy (Case 1) is described.
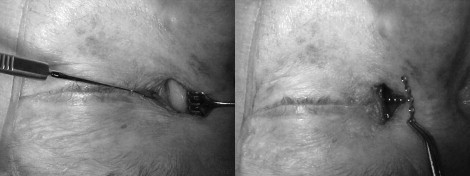
A 1.5-cm vertically oriented curvilinear skin incision is made at the midpoint between the medial canthus and the dorsum of the nose ( Figure 2 , Left). Only the thicker nasal skin is incised to avoid webbing. Sharp dissection toward the nasal bone is carried out until the medial canthal tendon is identified. A periosteal incision is made anterior to the tendon insertion ( Figure 2 , Left). The periorbita is reflected off the medial wall and subperiosteal dissection continues posteriorly toward the apex until the mid-orbit is reached. A 5-hole crossbar × 7-hole shaft T-plate (Synthes Craniofacial 1.0-mm Module 420.71; Synthes CMF, West Chester, Pennsylvania, USA) is inserted into the medial subperiosteal space to gauge the proper depth of dissection in accommodating the T-plate ( Figure 2 , Right). The crossbar of the T-plate measures 14 mm, and the shaft is 24 mm. The shaft of the T-plate is bent to conform to the contour of the anterior lacrimal crest and to assure proper alignment along the medial wall.
A 180-degree fornix-based medial conjunctival peritomy is made to expose the muscle insertion. The bulbar conjunctiva is elevated, and the intermuscular septae is separated from the nasal surface of the medial rectus in the peripheral surgical space using malleable retractors. A Freer periosteal elevator is introduced into the peripheral surgical space to create a periosteal opening to the subperiosteal space by incising the periorbita with the sharp end of the instrument. A 5-0 double-armed, nonabsorbable, braided, polyester (polyethylene terephthalate) suture on a spatulated needle (Mersilene; Ethicon, Inc, Somerville, New Jersey, USA) is folded in half, and the folded end of the suture is inserted into the medial peripheral surgical space with a bayonet forceps through the conjunctival peritomy incision. The tip of the bayonet forceps introduces the folded suture end into the subperiosteal space through the periosteal fenestration created by the periosteal elevator. The suture end is grasped by an alligator forceps in the subperiosteal space and retrieved through the skin incision ( Figure 3 , Left). The folded end of the suture is secured to the last hole on the shaft of the T-plate with multiple ties. The coupled unit is lowered into the subperiosteal space through the skin incision ( Figure 3 , Right). The shaft of the T-plate is situated below the frontoethmoidal suture line and away from the anterior and posterior ethmoidal arteries. The crossbar is permanently secured to the nasal bone anterior to the anterior lacrimal crest with 3 5-mm screws ( Figure 4 , Left). Screw placement into the suture line between the frontal process of maxilla and nasal bone should be avoided. The orbicularis muscle layer is reapproximated with 5-0 polyglactin 910 (Vicryl; Ethicon) sutures, and the skin is closed with 6-0 nylon sutures in an interrupted fashion.


The needle on each arm of the polyester suture (Mersilene; Ethicon) is passed in the sclera, adjacent to the medial rectus muscle insertion, and tied in an adjustable fashion with sufficient tension to adduct the eye into an orthophoric position as judged by the Hirschberg light reflex method ( Figure 4 , Right). The suture is tied in an adjustable fashion to allow for postoperative adjustment. The conjunctival peritomy incision is closed with 6-0 plain gut sutures. After recovery from anesthesia, the sutures are adjusted to align the eye into its final position.
For lateral placement, a curvilinear incision of the periosteum overlying the lateral orbital rim at lateral canthal tendon insertion is dissected off to expose a broad area of bone to accommodate the plate. The T-plate is bent at the junction between the crossbar and the shaft to conform to the contour of the rim to orient the shaft along the subperiosteal space of the lateral orbital wall. The crossbar of the T-plate is secured to the temporal surface of the lateral orbital rim and the shaft extends to a posterior depth of about 20 mm in the orbit.
Results
A total of 7 patients with complex paralytic strabismus underwent ocular realignment using the T-plate-based suture fixation technique. There were 6 women and 1 man with an average age of 55.7 years (range, 24–79 years).
The strabismus in 6 of the 7 patients was caused by third nerve palsy and/or medial rectus dysfunction. One of these patients had oculomotor nuclear complex damage causing limitation of upgaze in addition to exotropia. Another patient had concomitant medial rectus amputation sustained during functional endoscopic sinus surgery. The patient with esotropia had unilateral traumatic sixth nerve palsy. Patient demographics and treatment characteristics are summarized in the Table .
| Case | Age/Gender | Eye | Diagnosis/Etiology | Previous Procedures | T-Plate | Pre-op Deviation (PD) | Final Post-op Deviation (PD) | Change (Δ) (PD) a | Post-op Single Vision Near Primary Position | Complications | Follow-up (Months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 79/F | OS | Third nerve palsy – herpes | 1 | Medial | XT 20 | XT 6 | 14 | Binocular | None | 63 |
| 2 | 56/F | OD | Third nerve palsy/MR amputation – FESS | 3 | Medial | XT 50 | XT 10 | 40 | Binocular | None | 76 |
| 3 | 24/F | OS | Third nerve palsy – CVA | 1 | Medial | XT 25 | XT 18 | 7 | Binocular, face turn | Loose suture knots | 45 |
| 4 | 43/M | OS | Third nerve palsy – congenital | 3 | Medial | XT >90 | XT 18 | 72 | Monocular | None | 25 |
| 5 | 32/F | OD | Nuclear third nerve palsy – AVM | 1 | Medial | XT 70 | XT 10 | 60 | Binocular, chin elevation | Suture adjustment | 55 |
| 6 | 62/F | OD | Third nerve palsy – tumor/trauma | 0 | Medial | XT 45 | XT 12 | 33 | Monocular | None | 26 |
| 7 | 47/F | OD | Sixth nerve palsy – trauma | 3 | Lateral | ET 30 | ET 5 | 25 | Monocular | None | 63 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


