When the airways are overwhelmed by noxious particles, gases, or microorganisms, inflammatory and immune responses occur that may cause permanent structural changes. One consequence may be an overproduction of mucus and this may overwhelm mucociliary clearance mechanisms and cause a chronic cough phlegm syndrome. The expectorated mucus is usually clear or white (mucoid) but when it becomes infected, the mucus may become purulent and have a yellow or green color. Diseases associated with chronic productive cough discussed in this article include chronic bronchitis, bronchiectasis, and infectious and noninfectious bronchiolitis and their diagnosis and treatment.
Mucus secretion and cough provide a normal first-line defense against inhaled gases, particles, and microorganisms. Normally, approximately 50 mL of sputum is produced each day by the airway mucus-secreting tissue, the goblet cells in the epithelium, and submucosal seromucus glands. The viscoelasticity of the mucus is conferred by glycoproteins, called mucins, whose components are encoded by specific mucin (MUC) genes. The mucus is eliminated by the action of mucociliary clearance to the hypopharynx, where it is swallowed and rarely noticed. When the burden of gases, particles, or microorganisms that are inhaled becomes excessive, for example, as seen in cigarette smokers, those with noxious occupational exposures, or those with an influenza infection, it results in inflammatory and immune responses in the airways. One consequence is an overproduction of mucus. This may overwhelm mucociliary clearance mechanisms and cause chronic productive cough. The expectorated mucus is usually clear or white (mucoid) unless there is a high bacterial load in the respiratory secretions that causes the mucus to have a yellow or green color (purulent). The production of green sputum is a surrogate marker for intense bronchial inflammation and the presence of bacterial pathogens in increasing concentrations. A change of sputum from mucoid to purulent reflects an increased number of neutrophils containing the green pigment myeloperoxidase. Syndromes associated with chronic productive cough discussed in this article include chronic bronchitis, bronchiectasis, and infectious and noninfectious bronchiolitis ( Box 1 ). Bacterial bronchitis and unsuspected bacterial suppurative airway disease are discussed elsewhere in this issue.
Chronic bronchitis is a disease of the bronchi characterized by abnormal inflammatory response to noxious particles and gases (primarily cigarette smoking) and progressive airflow limitation. Its is usually manifested by cough and chronic sputum expectoration occurring on most days for at least 3 months of the year and for at least 2 consecutive years, when other pulmonary or cardiac causes for the chronic productive cough are excluded.
Bronchiectasis is an airway disorder associated with chronic cough and production of mucopurulent sputum related to chronic inflammation and infection. This eventually leads to bronchial wall damage, dilation, and permanent destruction. The pathologic features include intense inflammation, thickening, and constrictions of the airway wall, and resulting tortuosity, dilatation, ectasia, and eventual destruction of the distal bronchi and bronchioles.
Bronchiolitis encompasses a spectrum of infectious/postinfectious, inflammatory, and idiopathic syndromes that can affect the small airways less than or equal to 2 mm in diameter. This process can lead to variable degrees of injury to the bronchiolar epithelium and reversible or irreversible structural damage. Bronchiolitis can be the only manifestation of various clinical syndromes or may be a part of a spectrum of histopathologic and radiographic findings that may also involve the large airways and lung parenchyma.
Chronic bronchitis
Most smokers produce excessive amounts of sputum each day, as much as 100 mL/d more than normal. This results in cough and sputum production. The term, chronic bronchitis , has been used to describe this cough phlegm syndrome since the early nineteenth century, and in the mid–twentieth century, the British Medical Research Council definition became widely accepted: “a disease of the bronchi that is manifested by cough and sputum expectoration occurring on most days for at least 3 months of the year and for at least 2 consecutive years when other pulmonary or cardiac causes for the chronic productive cough are excluded.” Many, but not all, patients with chronic bronchitis develop expiratory flow limitation. Spirometry testing shows that reduced expiratory flow and measures, such as the forced expiratory volume in the first second of expiration (FEV 1 ), have been used to identify and stage the degree of airflow obstruction. Often in smokers with chronic bronchitis, destruction of alveolar walls (emphysema) also develops and this contributes to airflow limitation. The presence of chronic bronchitis without airflow obstruction has been referred to as simple chronic bronchitis and when accompanied by airflow obstruction the term, chronic obstructive bronchitis , or, more commonly, chronic obstructive pulmonary disease (COPD) , is used.
The excess mucus production in patients with chronic bronchitis occurs as a result of an increase in the size and number of the submucosal glands and an increase in the number of goblet cells on the surface epithelium. Mucous gland enlargement and hyperplasia of the goblet cells are, therefore, the pathologic hallmarks of chronic bronchitis and the amount of the gland correlates with the amount of intraluminal mucus. Goblet cells are normally absent in the small airways, and their presence there (often referred to as mucous metaplasia) is important to the development of COPD. The increase in mucus is linked specifically with an increase in MUC5B in the bronchiolar lumen. There is also upregulation of MUC5AC in the airway epithelium of patients with COPD and chronic cough compared to smokers without COPD and nonsmokers. In the larger airways of patients with chronic bronchitis, there is a reduction in the serous acini of the submucosal glands. This depresses local defenses to bacterial adherence, because these glands are known to produce microbial deterrents, such as lactoferrin, antiproteases, and lysozyme. Other epithelial alterations that are seen in patients with chronic bronchitis are a reduction in the number and length of the cilia and squamous metaplasia. The mucociliary abnormalities of chronic bronchitis cause the formation of a continuous sheet or blanket of mucus lining the airways instead of the discreet deposits of mucus seen in normal airways. Pooling of the secretions also may occur. This provides an additional source of bacterial growth and is likely important in the establishment of a chronic colonization in the tracheobronchial tree. These bacteria cause a release of toxins that can further damage the cilia and epithelial cells. Bacterial exoproducts are known to stimulate mucus production, slow ciliary beating, impair immune effector cell function, and destroy local immunoglobulins. This vicious cycle is especially seen in current smokers acompared with former smokers.
The cause of cough in patients with chronic bronchitis is multifactorial. Airway inflammation and excessive bronchial secretions are likely to activate the afferent limb of the cough reflex. There is evidence that the cough receptors are heightened in patients with chronic bronchitis as it has been demonstrated that capsaicin-induced cough is increased. When airflow obstruction is present, it often leads to an ineffective cough as a result of decreased expiratory flow, which, coupled with impaired mucociliary clearance, results in the further retention of secretions and a vicious cycle of chronic recurrent coughing. Even in the absence of airflow obstruction and with a short smoking history, impaired mucociliary clearance has been shown in young smokers. This occurs because of abnormal clearance in the small airways. Patients with advanced disease and evidence of airway obstruction have mucus retention in the small peripheral airways and larger central airways. This cycle is worsened during episodes of acute viral and bacterial infections that are common in patients with chronic bronchitis, referred to as an acute exacerbation of COPD.
Smoking and Chronic Bronchitis
The association of chronic cough and excessive mucus production with cigarette smoking has been established for decades. The pioneering work of Comstock and colleagues in middle-aged smokers showed that cigarette smokers had considerably more cough and phlegm than nonsmokers and that pipe and cigar smokers had intermediate levels of these symptoms. Those who quit smoking showed considerable improvement in these symptoms. Two decades later, the longitudinal Scottish Heart Health Study showed that current cigarette smokers had rates of chronic cough and chronic phlegm four to five times those of never-smokers and symptoms were more prevalent in men than in women (32.3% versus 6.5% for men and 24% versus 5.5% for women for chronic cough; 31% versus 8.3% for men and 21% versus 5.5% for women for chronic phlegm). The higher symptom rates in men were found in smokers, exsmokers, and never-smokers. There were substantially lower rates of chronic cough and chronic phlegm within a year of stopping smoking. Even 10 years after stopping, rates of symptoms among exsmokers remained a little above those of never-smokers. These studies emphasize the importance of smoking cessation in relieving cough and sputum production with chronic bronchitis. A widely held belief is that smoking cessation will lead to an increase in cough but this has proved unlikely among relatively healthy smokers who stop smoking and should not be a barrier to maintaining abstinence for most smokers.
More recently a 30-year Finnish study on the cumulative incidence of chronic bronchitis in middle-aged men was reported. The cumulative incidence of chronic bronchitis and COPD was 42% and 32%, respectively, in continuous smokers and 22% and 12% in nonsmokers. The symptoms of chronic bronchitis began at a median age of 55 years in smokers and in never-smokers at the age of 60 years. In this study the presence of chronic bronchitis resulted in a 13 mL per year excess in the longitudinal decline in pulmonary function and a higher mortality rate. The study was done in a rural environment, hence many were farmers. Occupational exposure to organic dusts, such as grain dust, may explain these findings in nonsmokers.
Thus, there is a strong association between smoking and cough and mucus production and there is evidence that excessive mucus production has a negative effect on the decline in pulmonary function with aging. In prospective studies of a middle-aged population, a rapid decline of FEV 1 has also been associated with the presence of severe airflow obstruction (FEV 1 /forced vital capacity <70% and FEV 1 <50% predicted), age 50 or older, female gender, and black race. The presence of chronic productive cough in a smoker should raise suspicion of underlying COPD and should prompt vigorous smoking cessation measures and lung function testing.
Acute Exacerbation of Chronic Bronchitis (Chronic Obstructive Pulmonary Disease)
In 2000, an international panel of chest physicians proposed a definition for an acute exacerbation of chronic bronchitis in patients with COPD that is widely accepted: “a sustained worsening of the patient’s condition, from the stable state and beyond normal day-to-day variations, that is acute in onset and necessitates a change in treatment in patients with underlying COPD.” Three subtypes (types 1, 2, and 3) have been identified that helped direct therapy. They were based on the occurrence of all or some of three specific symptoms: increased shortness of breath, increased cough and sputum volume, and increased sputum purulence. The presence of all three symptoms (type 1) implies a greater severity of disease and calls for treatment with antibiotics. Nonspecific systemic symptoms, such as fatigue, malaise, and fever, may be present and evidence of a systemic inflammatory response during a COPD exacerbation can be demonstrated by elevated blood levels of IL-6, tumor necrosis factor α, and C-reactive protein.
Causes of Chronic Obstructive Pulmonary Disease Exacerbations
Viral and bacterial infections are the main causative agents associated with COPD exacerbations and there is also epidemiologic evidence that high levels of air pollution with SO 2 , NO 2 , ozone, and airborne particulates may play a contributory role. The use of polymerase chain reaction technology has led to a greater recognition of the importance of respiratory viruses in the pathogenesis of exacerbations. At least 30% to 50% of all exacerbations are associated with a respiratory virus and this is especially seen in the winter months when these infections are more prevalent in the general community. In one prospective community study, rhinovirus was detected in 58% of virus-induced exacerbations and 23% of all COPD exacerbations. Other viruses that have been detected are the coronovirus, influenza virus, parainfluenza virus adenovirus, and respiratory syncytial virus. Bacteria are also an important cause of COPD exacerbations but viruses are associated with more severe exacerbations and recovery is more prolonged. Pathogenic bacteria can be found in approximately 50% of exacerbations and the acquisition of a new strain of bacterial pathogen is associated with a twofold risk of a new exacerbation. Typical bacteria associated with a COPD exacerbation are Haemophilus influenzae, Moraxella catarrhalis , and Streptococcus pneumoniae . Empiric therapy is usually given to cover these organisms as the sputum is not routinely cultured. There is evidence that multidrug-resistant bacteria, most commonly nonfermenting gram-negative bacilli, such as Pseudomonas aeruginosa, Acinetobacter baummani and Stenotrophomonas maltophilia , are becoming increasingly common with severe exacerbations. For severe exacerbations or those refractory to first-line treatment, a sputum culture and sensitivity may prove useful. Also, many patients hospitalized with an acute exacerbation of COPD have concomitant viral and bacterial infections. Such patients tend to have greater severity of illness and longer lengths of hospital stay. A severe exacerbation of COPD can lead to hypoxemic and hypercarbic respiratory failure that requires an ICU level of care and carries a high mortality. Patients with a higher frequency of exacerbations, in general, have a more profound deterioration in overall health status and a greater decline in lung function over time.
There are few clinical clues that may be helpful to distinguish viral-induced from bacterial-induced exacerbations of COPD. It is usually difficult to make this distinction. Patients with cold symptoms (nasal congestion, rhinorrhea, sore throat) and fever are more likely to have viruses detected from nasal aspirates. Sputum purulence as a result of increased numbers of white blood cells can be seen with viral or bacterial infection but the presence of green purulent sputum is especially predictive of a high bacterial load.
Treatment of an Acute Exacerbation of Chronic Obstructive Pulmonary Disease
Bronchodilator therapy has a role in the prevention and treatment of COPD exacerbations and is recommended for stable chronic bronchitis and for an acute exacerbation. Short-acting inhaled β-agonists, such as albuterol, and anticholinergics, such as ipratropium, are effective in improving symptoms and lung function in patients with an exacerbation. They are often given together but there is no evidence that the combination is more effective than a single agent. Oral corticosteroids (such as prednisone [40–60 mg]) have been shown to reduce hospitalizations and relapses after emergency department visits and for patients who require hospitalization; systemic corticosteroids improve symptoms more quickly and reduce hospital length of stay compared with placebo. Long-acting inhaled β-agonists, such as formoterol and salmeterol, and anticholinergics, such as tiotropium, reduce exacerbation rates in patients with COPD. The combination treatment with a long-acting β-agonist and inhaled corticosteroid reduces exacerbation rates greater than the individual components alone. The use of antibiotics for treatment of an acute exacerbation of chronic bronchitis is recommended as it shortens the course of the illness. There is, however, some uncertainty about their use because of conflicting clinical trial results. Antibiotics are most effective in patients with purulent sputum and in those with a greater severity of illness (those with the three cardinal symptoms of increased cough, increased sputum volume, and increased dyspnea) and in those with more severe airflow obstruction at baseline. The choice of antibiotics should be based on local bacterial resistance patterns and first-line drugs include macrolides, cephalosporins, doxycycline, and amoxicillin. For treatment failures and those who are hospitalized, other agents, such as fluoroquinolones and amoxicillin/clavulanate, are required. The use of antibiotics (macrolides) for prophylaxis in patients with frequent (three or more per year) exacerbations is effective and further clinical trials are necessary to confirm the risks ands benefits. Mucolytic agents and expectorants have not proved useful in the prevention or treatment of exacerbations of chronic bronchitis.
Bronchiectasis
Bronchiectasis is another cough phlegm syndrome caused by chronic inflammation and infection of the airways. Like chronic bronchitis, bronchiectasis is associated with chronic cough, production of mucopurulent sputum, and, when there is extensive lung involvement, shortness of breath. Unlike chronic bronchitis, the inflammation and infection seen with bronchiectasis causes the bronchial walls to become damaged and dilated, and this results in permanent destruction of bronchi. The pathologic features include intense inflammation, thickening, and constrictions of the airway wall and resulting tortuosity, dilatation, ectasia, and eventual destruction of the distal bronchi and bronchioles. Earlier changes include squamous metaplasia, desquamation of the lining epithelium, and extensive areas of necrotizing ulceration. The mucus found in the airways contains large numbers of neutrophils, and metalloproteinases and collagenases released by these cells are thought to play an important role in the destructive process of bronchiectasis. As the disease progresses, fibrosis of bronchial or bronchiolar walls occurs and peribronchiolar fibrosis also develops, leading to varying degrees of subtotal or total obliteration of bronchiolar lumens. The bronchi may become so dilated (up to four times their size) that on cut surfaces of pathologic specimens they appear as cysts filled with mucopurulent secretions. Clearance of mucus and bacteria by normal mucociliary mechanisms from bronchiectatic areas is impaired and a vicious cycle of repeated or prolonged bronchial infections, suppuration, and destruction ensues. This is the cause of the cough phlegm syndrome, the chronic infection with frequent exacerbations, the progressive decline of lung function and quality of life, and, for some, eventual mortality.
Clinical Features of Bronchiectasis
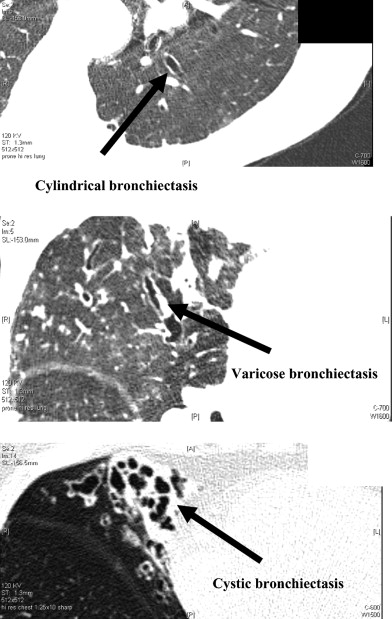
The physical findings of bronchiectasis are nonspecific and may include localized or diffuse crackles or wheezes and coarse rhonchi caused by retained airway secretions. The routine chest roentgenogram may be unable to detect the abnormalities or may underestimate the degree of bronchiectasis. High-resolution CT scan (HRCT) has become the standard method of diagnosis. A common classification of bronchiectasis is based on the anatomic variations demonstrated by HRCT; the terms, cylindrical, varicose , and cystic (saccular) bronchiectasis , have been used to describe the extent of bronchial distortion and destruction ( Fig. 1 ). More extensive involvement of the lungs and the presence of the cystic changes predict a much poorer prognosis. The natural history of this disease is usually associated with recurrent exacerbations of bronchial infection and decline of lung function. In later stages of the disease, progressive dyspnea, poor quality of life, cachexia, and cor pulmonale may occur and hemoptysis may complicate the course of the illness as a result of new and enlarged bronchial circulation to the areas of destroyed lung. In milder forms of the disease, patients may be relatively asymptomatic and may not demonstrate bacteria in their sputum, unless an acute infection (exacerbation) occurs. The organisms that usually infect patients with bronchiectasis are similar to those associated with chronic bronchitis: H influenzae, M catarrhalis , and S pneumoniae . Nonenteric gram-negative bacteria and Staphylococcus aureus are also commonly seen, however, and colonization and infection with P aeruginosa are frequently found in more advanced stages. Patients with P aeruginosa are more likely to have a more accelerated decline of lung function and more frequent exacerbations. Nontuberculous mycobacteria, Nocardia , and Aspergillus also may be cultured from the sputum of patients with bronchiectasis and their presence may represent airway colonization in a compromised airway or active infection. Anerobic bacteria are less frequently isolated from bronchiectatic airways.
Causes of Bronchiectasis
The causes and predisposing factors for bronchiectasis are usually categorized as (1) local bronchiectasis, caused by a local bronchial obstruction, poor airway clearance, and distal infection or by a primary local infection, such as pneumonia, that does not completely resolve, or (2) diffuse bronchiectasis, associated with a systemic disease or immune deficiency that causes diffuse airway abnormalities, which impair mucociliary clearance and lead to chronic infection and the cycle of wall distortion and destruction. These causes are listed in Box 2 . A review of these causes with an overview of this topic has recently been published.
Focal disease
Airway obstruction
- ■
Foreign body aspiration
- ■
Bronchial stricture (right middle lobe syndrome)
- ■
Endobronchial mass (carcinoma, adenoma)
- ■
Postinfection
- ■
Bacterial
- ■
Viral
- ■
Mycobacterial (tuberculosis and nontuberculous mycobacteria)
- ■
Diffuse disease
Postinfection
- ■
Measles, pertussis
- ■
Mycobacterial (tuberculosis and nontuberculous mycobacteria)
- ■
Congenital syndromes
- ■
CF
- ■
Primary ciliary dyskinesia
- ■
Young’s syndrome
- ■
Tracheobronchomegaly
- ■
Cartilage deficiency (Williams-Campbell syndrome)
- ■
Marfan syndrome
- ■
α 1- Antitrypsin deficiency
- ■
Yellow nail syndrome
- ■
Immunodeficiency states
- ■
Primary immunoglobulin deficiency (IgG, IgA)
- ■
HIV/AIDS
- ■
Chronic lymphatic leukemia
- ■
Chemotherapy immune depression
- ■
Immune modulation post transplantation
- ■
Immune-mediated diseases
- ■
Allergic bronchopulmonary aspergillosis
- ■
Rheumatoid arthritis
- ■
Relapsing polychondritis
- ■
Sjögren’s syndrome
- ■
Inflammatory bowel disease
- ■
Gastroesophageal reflux disease
Chronic aspiration
- ■
Esophageal dysmotolity
- ■
Dysphagia
- ■
Chronic illicit drug abuse
- ■
Idiopathic
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


