Purpose
To evaluate the prognostic value of the cone outer segment tips (COST) and other features using spectral-domain optical coherence tomography (SD-OCT) in patients undergoing epiretinal membrane (ERM) surgery.
Design
Retrospective observational case series.
Methods
Fifty eyes of 49 patients that underwent vitrectomy for idiopathic ERM were studied. Best-corrected visual acuity (BCVA) and SD-OCT images were examined preoperatively and at 1 and 6 months postoperatively. The SD-OCT features evaluated included central foveal thickness (CFT) and the status and defect diameter of the external limiting membrane (ELM), the photoreceptor inner/outer segment (IS/OS) junction, and the COST line. The associations between SD-OCT parameters and BCVA were analyzed.
Results
There was no ELM disruption found, and thus the eyes were categorized into 3 groups: Group A, with a continuous IS/OS and COST line; Group B, with a continuous IS/OS but disrupted COST line; and Group C, with a disrupted IS/OS and COST line. At 6 months, Group A showed a significantly better BCVA than Group B ( P < .005), and poorer BCVA was noted in Group C ( P = .034). Defect diameters of IS/OS and COST line were also significantly correlated with BCVA postoperatively. The BCVA at 6 months was better in order of Group A, B, and C as assigned at baseline ( P < .05) or 1 month ( P < .001). There was no significant correlation between CFT and BCVA.
Conclusions
The status of the COST line, in conjunction with the IS/OS junction, is a useful prognostic factor after ERM surgery.
Idiopathic epiretinal membrane (ERM) is a frequently diagnosed pathology in ophthalmologic practice. It induces tangential traction on the retina, leading to visual disturbance or metamorphopsia. Surgical removal of the ERM is a standard procedure for improving vision by releasing its tractional force. However, functional results are sometimes unsatisfactory despite successful removal of the ERM. Several prognostic factors, such as preoperative visual acuity and symptom duration, have been proposed as affecting postoperative visual acuity.
The introduction of optical coherence tomography (OCT) has provided critical insights into various retinal conditions including ERM. OCT, which allows noninvasive visualization of retinal morphology, has been widely accepted as a standard tool for diagnosis and management of ERM. One of the prognostic factors suggested using OCT includes macular thickness. Although conventional time-domain OCT was limited in delineating subtle pathologic changes, spectral-domain OCT (SD-OCT), with its high resolution of up to 5 μm and high scanning speed, has allowed layer-by-layer evaluation of the retina. Many studies using SD-OCT have highlighted the impact of the integrity of the photoreceptor inner/outer segment (IS/OS) junction on visual acuity in various macular pathologies including ERM.
The higher resolution and signal-to-noise ratio of the SD-OCT have also facilitated visualization and evaluation of other fine foveal microstructures besides the IS/OS junction. One of the features is the external limiting membrane (ELM). For example, a relationship between ELM status and visual acuity has been reported for retinal detachment, macular holes (MHs), age-related macular degeneration (AMD), and others. Another SD-OCT hallmark recently identified is the cone outer segment tips (COST), also known as the Verhoeff membrane. The disruption of the COST line has been observed in several macular pathologies and seems to indicate an early sign of photoreceptor damage. Thus, this feature could be optimal for evaluating the subtle photoreceptor changes expected in the clinical course of ERM. However, the association between the status of the COST line and visual function has yet to be well documented in ERM and other diseases.
In this study, we assessed macular morphologic features such as the COST line, the IS/OS junction, and the ELM on SD-OCT images in patients undergoing ERM surgery and evaluated the prognostic value of these features.
Patients and Methods
We retrospectively studied a consecutive series of patients that had undergone successful vitrectomy for an idiopathic ERM at Kobe City Medical Center General Hospital from March 27, 2009 through June 29, 2010 and were followed for at least 6 months postoperatively. Cases with any ocular diseases that could affect visual potential, such as diabetic retinopathy, macular degeneration, rhegmatogenous retinal detachment, glaucoma, cataract of more than grade III in Emery-Little classification, and corneal pathologies, were excluded from the study.
A standard 3-port 23-gauge pars plana vitrectomy was performed. A core vitrectomy was performed with induction of a posterior vitreous detachment if not already present. ERM peeling was carried out using end-gripping forceps. The internal limiting membrane (ILM) was subsequently peeled at the surgeon’s discretion using 0.05% indocyanine green (ICG) dye. The area of ERM or ILM peeling was 2 to 3 optic disc diameters around the fovea. Phacoemulsification and aspiration with intraocular lens implantation was performed simultaneously if a clinically significant cataract was present.
All patients underwent a comprehensive clinical examination preoperatively and at 1 and 6 months postoperatively. These examinations included best-corrected visual acuity (BCVA) measurements and fundus examination by indirect ophthalmoscopy and slit-lamp biomicroscopy. SD-OCT imaging was performed in each patient on the same day as the clinical examination.
SD-OCT images were obtained using Spectralis (Spectralis Family Acquisition Module, version 4.0.2.0; Heidelberg Engineering, Heidelberg, Germany) with Heidelberg Eye Explorer (version 1.6.1.0; Heidelberg Engineering). The measurements were performed under sufficient pupillary dilation. Horizontal and vertical scans through the fovea were recorded for each patient. The eye tracking system of the device was used to detect and keep the correct scanning position; care was taken to ensure that each scan exactly passed through the foveal center. To enhance signal-to-noise ratio, more than 40 scans were averaged for each record.
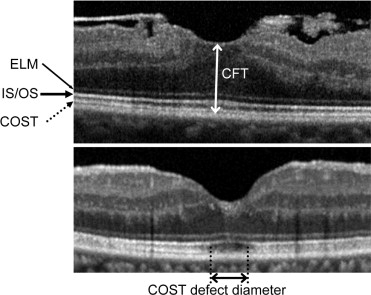
The continuity of the ELM, the IS/OS junction, and the COST line were evaluated on preoperative and postoperative SD-OCT images. A disruption of the line was diagnosed when there was a loss of each hyperreflective line at the fovea. ELM defect diameter (the length of region where the back-reflection line corresponding to the ELM was absent), IS/OS defect diameter, COST defect diameter, and central foveal thickness (CFT; the distance between the inner surface of the retina and the inner border of the retinal pigment epithelium [RPE] at the fovea) were also measured preoperatively and postoperatively ( Figure 1 ). Defect diameter of each line was measured for a 2-mm-diameter area, based on the diameter of the physiologic fovea being 1.85 mm. That is, a total or >2 mm defect of the line on an SD-OCT image was regarded as a defect diameter of 2 mm. The caliper function of the software package was used for data collection, and the 2 measurements on horizontal and vertical scans were averaged. Two of the authors (M.S., M.H.), who were masked as to the clinical conditions of the participants, interpreted the SD-OCT images. For quantitative parameters, the average of 2 measurements was taken. When there were discrepancies in the judgments of qualitative parameters, another author (A.O.) was consulted for the final decision.
Statistical analyses were conducted using SPSS software (version 11.0.1; SPSS Inc, Chicago, Illinois, USA). Descriptive analyses were recorded as means ± standard deviation unless otherwise specified. The BCVA was measured with a Landolt C chart and then converted to logarithm of the minimal angle of resolution (logMAR) equivalents. A paired t test was carried out to assess changes over time. Group differences in BCVA according to photoreceptor status were evaluated with a Mann-Whitney U test or Kruskal-Wallis test followed by the Dunn post hoc test. Correlations between BCVA and quantitative SD-OCT parameters were investigated using the Spearman rank correlation test. The Fisher exact probability test was performed to compare the incidence of photoreceptor disruption. P values <.05 were considered to be statistically significant.
Results
A total of 50 eyes of 49 patients with a successful ERM removal met the study criteria. The patients had a mean age of 69.1 ± 8.0 years (range, 52 to 87 years) and were composed of 22 men and 27 women. Three eyes (6%) were pseudophakic preoperatively and 47 eyes (94%) underwent a simultaneous cataract surgery. ILM peeling was performed on 43 eyes (86%). There were no significant surgical complications that might affect visual acuity and SD-OCT changes.
The time-course changes in logMAR BCVA and the status of the ELM, IS/OS junction, COST line, and CFT are shown in Table 1 . The mean decimal BCVA significantly improved from 0.52 (0.28 ± 0.25, logMAR) preoperatively to 0.79 (0.10 ± 0.22, logMAR) at 6 months postoperatively ( P < .001). There were no eyes with ELM disruption during the study period. At baseline, the IS/OS junction retained its continuity in all cases, while the COST line was disrupted in 24 eyes (48%). The disruption of the IS/OS junction and the COST line temporarily increased at 1 month and decreased to near the baseline level thereafter. CFT showed a significant decrease from 356 ± 145 μm preoperatively to 303 ± 92 μm at 6 months postoperatively ( P = .005), though the decrease at 1 month was not significant ( P = .104). In the fellow eyes, the ELM, IS/OS junction, and COST line were intact at baseline except in 2 eyes with COST line disruption attributable to branch retinal vein occlusion or ERM.
| Baseline | 1 Month | 6 Months | |
|---|---|---|---|
| logMAR BCVA | 0.28 ± 0.25 | 0.15 ± 0.28 | 0.10 ± 0.22 |
| ELM | |||
| Disrupted, no. (%) | 0 (0%) | 0 (0%) | 0 (0%) |
| IS/OS | |||
| Disrupted, no. (%) | 0 (0%) | 5 (10%) | 2 (4%) |
| Defect diameter (μm) | 0 | 17 ± 73 | 5 ± 28 |
| COST | |||
| Disrupted, no. (%) | 24 (48%) | 35 (70%) | 27 (54%) |
| Defect diameter (μm) | 323 ± 519 | 493 ± 536 | 304 ± 399 |
| CFT (μm) | 356 ± 145 | 329 ± 106 | 303 ± 92 |
Since there were no ELM disruptions found, we categorized the study eyes into 3 groups according to the integrity of the IS/OS junction and the COST line at each time point: continuous IS/OS junction and COST line (Group A); continuous IS/OS junction but disrupted COST line (Group B); and disrupted IS/OS junction and COST line (Group C). There were various patterns of changes from baseline to 1 month: of the 26 eyes in Group A at baseline, 14 eyes were reassigned to Group B (13 eyes) or Group C (1 eye) at 1 month, and of the 24 eyes in Group B at baseline, 3 eyes improved to Group A, whereas 4 eyes worsened to Group C at 1 month. No patients worsened from 1 month to 6 months. Figure 2 shows logMAR BCVA in the 3 groups before, 1 month after, and 6 months after the surgery. Although the BCVA did not differ significantly among the groups at baseline ( P = .463), the BCVA at 1 month differed significantly ( P < .001); Group A had the best BCVA, Group B was intermediate, and Group C had the worst BCVA. At 6 months, the BCVA in Group A was significantly better than that in Group B ( P < .001). Although the differences in BCVA between Group C and Group A or B were not significant at 6 months ( P = .072, P = .165, respectively), the BCVA in Group C was significantly worse than in Group A plus B ( P = .034).
The correlation coefficients between logMAR BCVA and SD-OCT parameters, including IS/OS defect diameter, COST defect diameter, and CFT preoperatively and at 1 and 6 months postoperatively, are given in Table 2 . Although none of the parameters showed significant correlations with BCVA preoperatively, IS/OS defect diameter and COST defect diameter were significantly correlated with BCVA at 1 and 6 months postoperatively, with COST defect diameter showing higher correlations than IS/OS defect diameter. There were no significant correlations between CFT and BCVA at any point.
| Baseline | 1 Month | 6 Months | |
|---|---|---|---|
| IS/OS defect diameter | — | 0.42 ( P = .002) | 0.30 ( P = .032) |
| COST defect diameter | 0.13 ( P = .356) | 0.66 ( P < .001) | 0.73 ( P < .001) |
| CFT | 0.22 ( P = .129) | 0.05 ( P = .755) | −0.03 ( P = .843) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


