Purpose
To evaluate serum soluble Flt-1 (sFlt-1) in age-related macular degeneration (AMD) patients.
Design
Case-control study.
Methods
Study involved 56 non-AMD participants, 53 early AMD patients, and 97 neovascular AMD patients from Belfast in Northern Ireland. Serum samples were collected from each patient. Serum sFlt-1 was measured by human sVEGFR1/sFlt-1 ELISA kit. The results were analyzed by Excel and SPSS.
Results
Serum sFlt-1 concentration of non-AMD, early AMD, and neovascular AMD were 90.8 ± 2.9 pg/mL (±standard error of the mean), 88.2 ± 2.6 pg/mL, and 79.9 ± 2.2 pg/mL. sFlt-1 from neovascular AMD patients was significantly decreased compared to non-AMD and early AMD patients (ANOVA, P < .01). For each 10-point increase in sFlt-1, the odds for having neovascular AMD compared with non-AMD and neovascular AMD decrease by 27.8%, odds ratio (OR) = 0.722 (95% confidence interval [CI]: 0.588–0.888, P = .002) and 27.0%, OR = 0.730 (95% CI: 0.594–0.898, P = .003), respectively. In patients over 73 years of age, serum sFlt-1 <80 pg/mL was associated with a >6-fold higher risk of neovascular AMD.
Conclusions
Reduced serum sFlt-1 differentiates those patients with neovascular AMD from both early AMD and non-AMD participants. In those aged over 73, serum sFlt <80 pg/mL seems to indicate a particularly high risk of neovascular AMD. Our results indicate serum sFlt-1 could be a biomarker for development of neovascular AMD.
Age-related macular degeneration (AMD) is the leading cause of irreversible visual blindness over the age of 50 in the western world. Prior to the development of visual loss, degenerative changes manifest initially as the accumulation of extracellular protein and lipid, which occur at the Bruch membrane, retinal pigment epithelium (RPE), and photoreceptor interfaces and characteristically manifest as drusen. These features are not associated with overt sight loss and are termed early AMD. Approximately 1 in 2 persons with extensive macular drusen will progress within 5 years to sight-threatening geographic atrophy (GA) and/or neovascularization (neovascular AMD), which are late-stage manifestations of the condition. In a large long-term epidemiologic study, roughly a quarter of patients over the age of 75 were found to have some features of AMD, about 80% of whom have dry AMD and are at risk of converting to exudative AMD. The onset of neovascular AMD generally results in sudden acute vision loss and, if left untreated, can cause permanent loss of sight. Neovascular AMD accounts for 90% of the blindness attributable to AMD.
While age is the strongest demographic risk factor associated with AMD, there is also a significant genetic component with at least 19 loci reported to be associated with AMD. The most significant associations are found with a tyrosine-histidine change at amino acid 402 of complement factor H (CFH), which is involved in innate immunity and with the HTRA1/ARMS2 locus, which is thought to affect matrix stability. Compared with genetic risk factors, serum markers are less well characterized. Although various candidates have been proposed as risk factors for AMD, currently the most studied serum biomarker is elevated C-reactive protein (CRP). CRP is a systemic marker of inflammation and is associated with a variety of different diseases, including heart disease, collagen-vascular disorders, and temporal arteritis; a recent meta-analysis has confirmed that high serum levels (>3 mg/L) of CRP are associated with a 2-fold likelihood of late AMD.
Vascular endothelial growth factor (VEGF) plays an important role in the pathogenesis and treatment of neovascular AMD. Soluble fms-like tyrosine kinase-1 (sFlt-1 or VEGFR1) is an antiangiogenic receptor for VEGF that binds and sequesters VEGF, reducing its angiogenic activity. Recently, we demonstrated that the decoy VEGF receptor, sFlt-1, in RPE is mechanistically required for subretinal vascular demarcation. Moreover, patients with neovascular AMD expressed less sFlt-1 in the RPE and conditional knockout of sFlt-1 in the RPE showed spontaneous choroidal neovascularization. As sFlt-1 is also found in serum, we hypothesized that serum sFlt-1 might be reduced in patients with neovascular AMD, either as a byproduct or as a cause of their condition. To further explore this potential link, we examined sFlt-1 in sera from non-AMD (controls), early AMD, and neovascular AMD patients.
Methods
The study adhered to the tenets of the Declaration of Helsinki on research into human volunteers, and the design was approved by the Research Ethics Committee of Queen’s University of Belfast. After informed consent, serum samples were collected in Northern Ireland (50-mile radius around Belfast) and then analyzed in a deidentified manner. To examine sFlt-1 level in patients’ serum, we used Human sVEGF R1/Flt-1 Quantikine ELISA Kit (R&D Systems Inc., Minneapolis, USA) following the manufacturer’s instructions.
Sample Collection
Controls
These were obtained as part of a population-based study cohort collected in Belfast according to the methods outlined previously. In brief, adult men and women 65 years or older were randomly identified from 2 general practice registers. The study participants’ general practitioner excluded those with severe physical disability, dementia, or other debilitating disease that would preclude a visit to the study clinic. From the 205 who participated we randomly selected 52 with no evidence of early or late AMD in either eye with the classification based on systematic grading of their color fundus photographs.
Cases
These were obtained from the Belfast participants in the CARMA study, whose recruitment and data collection methods are outlined elsewhere. A random sample of those with bilateral drusen ≥63 μm and unilateral neovascular AMD who had serum samples and gradable fundus photographs were obtained.
Cigarette smoking
Participants were categorized as nonsmokers or ever smokers.
Age-related macular degeneration grade
Fundus photographs were graded in the photographic reading center at Queen’s University of Belfast by trained graders using the definitions of the Wisconsin Age-Related Maculopathy Grading System. In brief, the presence and type of drusen and pigmentary irregularities were evaluated within segments of the 3000-μm-radius grid, which was placed with its center on the fovea. A graded categorical approach was used to obtain an estimate of the number of drusen within the grid. Geographic atrophy (GA) was defined as areas of atrophy in excess of 175 μm with well-delineated margins within which choroidal vessels could be observed. Choroidal neovascularization was said to be present if stereoscopic examination showed subretinal fluid, exudate, hemorrhage, and/or scar tissue in the macular region of the fundus. When both GA and choroidal neovascularization were present in the same eye, the person was classified as having neovascular AMD. Participants were categorized based on the features observed in the more severely affected eye. In the absence of drusen >63 μm or pigmentary irregularities in either eye, participants were designated as non-AMD (controls). Participants with drusen ≥63 μm or pigmentary irregularities in at least 1 eye were classified as early AMD. The remaining participants had neovascular AMD.
Statistical Analysis
Student t test (2-tailed), χ 2 test, and ANOVA were performed using Microsoft Excel (Microsoft, Redmond, USA). Logistic regressions were performed using SAS software version 9.3 (SAS Institute Inc., Cary, USA). A logistic regression model was used to determine the effects of sFlt-1 level, age, sex, and smoking history on the stage of macular degeneration (AMD stage). When considering the levels of non-AMD, early AMD, and neovascular AMD in a polytomous (multilevel) logistic regression, the results of the score test indicated that the proportional odds assumption was not met. Therefore outcomes were considered in pairs of non-AMD vs early AMD, early AMD vs neovascular AMD, and non-AMD vs neovascular AMD.
Results
Demographics
Table 1 displays the age, sex, and smoking status of those participants from whom the samples were derived. Participants with neovascular AMD were older and more likely to have been smokers compared to those with early AMD or non-AMD.
| All Participants (n = 206) | AMD Grade | Age | Sex | Smoking | Missing | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-AMD (n = 56) | Early AMD (n = 53) | Neovascular AMD (n = 97) | P Value | <73 (n = 96) | ≥73 (n = 109) | P Value | Female (n = 108) | Male (n = 92) | P Value | Non (n = 87) | Past (n = 78) | Current (n = 35) | P Value | |||
| Age (y, ± SD) | 73.0 ± 6.9 | 71.9 ± 4.7 | 70.4 ± 7.4 | 75.1 ± 7.0 | <.001 | 67.0 ± 4.4 | 78.3 ± 3.6 | 73.3 ± 6.7 | 72.6 ± 7.1 | .47 | 73.9 ± 6.7 | 73.3 ± 7.1 | 70.0 ± 6.5 | .017 | 1 | |
| Sex, F/M | 110/95 | 30/25 | 32/21 | 48/49 | .44 | 51/45 | 59/50 | .89 | – | – | 64/23 | 26/52 | 18/17 | <.001 | 1 | |
| Non/past/current smoker | 87/78/35 | 24/9/17 | 27/20/6 | 36/49/12 | <.001 | 38/33/23 | 49/45/12 | .050 | 67/26/18 | 23/52/17 | <.001 | – | – | – | 6 | |
| Non-AMD (%) | 27.2 | – | – | – | 37.5 | 17.4 | <.001 | 27.3 | 26.3 | .20 | 27.6 | 11.5 | 48.6 | <.001 | ||
| Early AMD (%) | 25.7 | – | – | – | 35.4 | 17.4 | 29.1 | 22.1 | 31.0 | 25.6 | 17.1 | |||||
| Neovascular AMD (%) | 47.1 | – | – | – | 27.1 | 65.1 | 43.6 | 51.6 | 41.4 | 62.8 | 34.3 | |||||
| Serum sFlt-1 concentration (pg/mL, ± SEM) | 85.0 ± 1.5 | 90.8 ± 2.9 | 88.2 ± 2.6 | 79.9 ± 2.2 | .0043 | 84.7 ± 2.1 | 84.8 ± 2.1 | .99 | 81.7 ± 2.0 | 88.3 ± 2.2 | .027 | 87.4 ± 2.2 | 83.7 ± 2.6 | 79.8 ± 3.0 | .19 | |
Serum Soluble Flt-1 Is Lower in Neovascular Age-Related Macular Degeneration Patients
Serum sFlt-1 concentrations from non-AMD, early AMD, and neovascular AMD cohorts were 90.8 ± 2.9 pg/mL (±standard error of the mean [SEM]), 88.2 ± 2.6 pg/mL, and 79.9 ± 2.2 pg/mL, respectively ( Table 1 ). sFlt-1 serum levels in neovascular AMD patients were significantly lower than in sera from non-AMD and early AMD patients ( Figure 1 , P = .0033 and P = .019, respectively).

We also analyzed serum sFlt-1 levels of all participants by age, sex, and smoking history ( Table 1 ). When the participants were divided into 2 groups by age 73 (the median age of our population sample), serum sFlt-1 levels were 84.7 ± 2.1 pg/mL (<73 years) and 84.8 ± 2.1 pg/mL (≥73 years), respectively. Serum sFlt-1 level in female subjects (81.7 ± 2.0 pg/mL) was lower than that in male subjects (88.3 ± 2.2 pg/mL), significantly ( P = .027). Serum sFlt-1 was not significantly different between nonsmoker (87.4 ± 2.2 pg/mL), past smoker (83.7 ± 2.6 pg/mL), and current smoker (79.8 ± 3.0 pg/mL).
Reduced Serum Soluble Flt-1 Was Associated With Neovascular Age-Related Macular Degeneration in Patients Over 73 Years of Age
Since participants with neovascular AMD were older than those with early AMD and non-AMD, we compared serum sFlt-1 concentration in patients aged <73 years or ≥73 years ( Table 2 ). In those aged <73 years, serum sFlt-1 concentrations from non-AMD, early AMD, and neovascular AMD were 87.9 ± 3.8 pg/mL, 85.3 ± 3.3 pg/mL, and 79.7 ± 3.3 pg/mL, respectively. This was not statistically significant (ANOVA P = .31). In subjects with age ≥73 years, serum sFlt-1 concentrations from non-AMD, early AMD, and neovascular AMD were 93.9 ± 4.1 pg/mL, 93.5 ± 4.0 pg/mL, and 80.0 ± 2.6 pg/mL, respectively. Serum sFlt-1 in neovascular AMD subjects was significantly decreased compared with non-AMD and early AMD subjects ( P = .014 and P = .016, respectively).
| Age <73 Years (n = 96) | Age ≥73 Years (n = 109) | Missing | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-AMD (n = 36) | Early AMD (n = 34) | Neovascular AMD (n = 26) | P Value | Non-AMD (n = 19) | Early AMD (n = 19) | Neovascular AMD (n = 71) | P Value | ||
| Sex, F/M | 20/16 | 20/14 | 11/15 | .42 | 10/9 | 12/7 | 37/34 | .68 | 5 |
| Non/past/current smoker | 18/4/12 | 13/16/5 | 7/13/6 | .008 | 6/5/5 | 14/4/1 | 29/36/6 | .007 | |
| Serum sFlt-1 concentration (pg/mL, ± SEM) | 87.9 ± 3.8 | 85.3 ± 3.3 | 79.7 ± 3.9 | .31 | 93.9 ± 4.1 (0.32) | 93.5 ± 4.0 (0.13) | 80.0 ± 2.6 (0.95) | .007 | |
Sex and Smoking Status Did Not Affect Serum Soluble Flt-1
To determine if sex impacted the relationship between AMD stage and sFlt-1 concentration, we stratified the data by sex ( Table 3 ). In female subjects, serum sFlt-1 levels of non-AMD, early AMD, and neovascular AMD were 88.4 ± 3.8 pg/mL (±SEM), 83.2 ± 3.6 pg/mL, and 76.5 ± 2.9 pg/mL, respectively. In male subjects, serum sFlt-1 levels of non-AMD, early AMD, and neovascular AMD were 91.8 ± 4.4 pg/mL, 95.9 ± 2.9 pg/mL, and 83.2 ± 3.3 pg/mL, respectively. In both male and female subjects, sFlt-1 was lower in neovascular AMD subjects than in non-AMD and early AMD subjects. Male serum sFlt-1 levels were relatively higher than those in female subjects in early AMD ( P = .0148).
| Female | ||||
|---|---|---|---|---|
| Non-AMD (n = 30) | Early AMD (n = 32) | Neovascular AMD (n = 48) | P Value | |
| Age (±SD) | 71.7 ± 4.7 | 70.5 ± 7.6 | 76.2 ± 6.0 | <.001 (ANOVA) |
| Non/past/current smoker | 17/4/7 | 21/6/5 | 26/16/6 | .26 (χ 2 test) |
| Serum sFlt-1 concentration (pg/mL, ± SEM) | 88.4 ± 3.8 | 83.2 ± 3.6 | 76.5 ± 2.9 | .041 (ANOVA) |
| Male | ||||
|---|---|---|---|---|
| Non-AMD (n = 25) | Early AMD (n = 21) | Neovascular AMD (n = 49) | P Value | |
| Age (±SD) | 72.2 ± 4.8 | 70.2 ± 7.6 | 73.9 ± 7.8 | .127 (ANOVA) |
| Non/past/current smoker | 7/5/10 | 6/14/1 | 10/33/6 | <.001 (χ 2 test) |
| Serum sFlt-1 concentration (pg/mL, ± SEM) | 91.8 ± 4.4 | 95.9 ± 2.9 | 83.2 ± 3.3 | .045 (ANOVA) |
To examine whether smoking affected serum sFlt-1 in our data set, we compared serum sFlt-1 level across AMD groups stratified by smoking state ( Table 4 ). In nonsmokers, serum sFlt-1 levels of non-AMD, early AMD, and neovascular AMD were 95.2 ± 4.4 pg/mL, 87.5 ± 3.8 pg/mL, and 82.0 ± 3.4 pg/mL, respectively. In past smokers, serum sFlt-1 levels of non-AMD, early AMD, and neovascular AMD were 93.0 ± 8.8 pg/mL, 88.0 ± 4.7 pg/mL, and 80.2 ± 3.4 pg/mL, respectively. In current smokers, serum sFlt-1 levels of non-AMD, early AMD, and neovascular AMD were 80.9 ± 3.9 pg/mL, 92.5 ± 9.3 pg/mL, and 72.0 ± 8.5 pg/mL, respectively. We found that the sFlt-1 level of neovascular AMD patients is lowest in all groups. When comparing serum sFlt-1 between nonsmokers, past smokers, and current smokers, we could not find any significant differences among non-AMD, early AMD, and neovascular AMD groups.
| Nonsmoker | ||||
|---|---|---|---|---|
| Non-AMD (n = 24) | Early AMD (n = 27) | Neovascular AMD (n = 36) | P Value of Row | |
| Age (±SD) | 71.1 ± 4.1 | 72.2 ± 7.7 | 76.9 ± 6.1 | <.001 (ANOVA) |
| Sex, F/M | 17/7 | 21/6 | 26/10 | .83 (χ 2 test) |
| Serum sFlt-1 concentration (pg/mL, ± SEM) | 95.2 ± 4.4 | 87.5 ± 3.6 | 82.0 ± 3.4 | .055 (ANOVA) |
| Past Smoker | ||||
|---|---|---|---|---|
| Non-AMD (n = 9) | Early AMD (n = 20) | Neovascular AMD (n = 49) | P Value | |
| Age (±SD) | 73.9 ± 5.4 | 68.7 ± 6.9 | 75.0 ± 6.7 | .0028 (ANOVA) |
| Sex, F/M | 4/5 | 6/14 | 16/33 | .74 (χ 2 test) |
| Serum sFlt-1 concentration (pg/mL, ± SEM) | 93.0 ± 8.8 | 88.0 ± 4.7 | 80.2 ± 3.4 | .19 (ANOVA) |
| Current Smoker | ||||
|---|---|---|---|---|
| Non-AMD (n = 17) | Early AMD (n = 6) | Neovascular AMD (n = 12) | P Value | |
| Age (±SD) | 71.2 ± 5.1 | 67.5 ± 5.9 | 69.6 ± 8.5 | .49 (ANOVA) |
| Sex, F/M | 7/10 | 5/1 | 6/6 | .20 (χ 2 test) |
| Serum sFlt-1 concentration (pg/mL, ± SEM) | 80.9 ± 3.9 | 92.5 ± 9.3 | 72.0 ± 8.5 | .066 (ANOVA) |
| P Value of Column | ||||
|---|---|---|---|---|
| Age | .29 (ANOVA) | .16 (ANOVA) | .006 (ANOVA) | |
| Sex | .13 (χ 2 test) | .002 (χ 2 test) | .002 (χ 2 test) | |
| Serum sFlt-1 concentration | 0.10 (ANOVA) | .85 (ANOVA) | .38 (ANOVA) | |
Logistic Regression Model
A logistic regression model was used to investigate the relationship between sFlt-1 concentration and AMD group, corrected for age, sex, and smoking ( Table 5 ).
| Effect | Non-AMD vs Early AMD | Non-AMD vs Neovascular AMD | Early AMD vs Neovascular AMD | |||
|---|---|---|---|---|---|---|
| Odds Ratio [95% CI] | P Value | Odds Ratio [95% CI] | P Value | Odds Ratio [95% CI] | P Value | |
| Age units = 1 | 0.959 [0.897–1.026] | .222 | 1.083 [1.019–1.152] | .011 | 1.128 [1.066–1.193] | <.001 |
| sFlt-1 units = 10 | 0.972 [0.787–1.200] | .789 | 0.722 [0.588–0.888] | .002 | 0.730 [0.594–0.898] | .003 |
| Sex, F vs M | 1.572 [0.643–3.843] | .321 | 0.759 [0.335–1.720] | .509 | 0.470 [0.201–1.099] | .082 |
| Ever smoker vs nonsmoker | 0.365 [0.120–1.112] | .076 | 0.496 [0.183–1.344] | .168 | 2.577 [0.733–9.058] | .140 |
| Past smoker vs never smoker | 2.688 [0.955–7.566] | .061 | 4.225 [1.624–10.996] | .003 | 1.884 [0.792–4.481] | .152 |
When non-AMD and early AMD groups were compared, none of the effects were significant. Next, non-AMD and neovascular AMD were compared. Controlling for sex, smoking history, and age, for each 10-point increase in serum sFlt-1 the odds of having neovascular AMD decreased by 27.8%, odds ratio (OR) = 0.722 (95% confidence interval [CI]: 0.588–0.888, P = .002). Controlling for sex, sFlt-1 level, and smoking history, for each increase in year of age the odds of having neovascular AMD increased by 8.3%, OR = 1.083 (95% CI: 1.019–1.152, P = .011). Sex and smoking history were not significant. Knowledge of the serum sFlt-1 improved the prediction of neovascular AMD vs non-AMD subjects.
Finally, we compared early AMD and neovascular AMD. Controlling for sex, smoking history, and age, for each 10-point increase in sFlt-1 the odds for having neovascular AMD decreased by 27%, OR = 0.730 (95% CI: 0.594–0.898, P = .003). Controlling for sex, smoking history, and serum sFlt-1 level, for each increase in year of age the odds of having neovascular AMD increased by 12.8%, OR = 1.128 (95% CI: 1.066–1.193, P < .001). Sex and smoking history were not significant. To estimate whether knowledge of the serum sFlt-1 level improves the prediction of neovascular AMD, we determined receiver operating curves and compared the area under the curve (AUC) in >73 patients in a model accounting for sex and smoking status ( Table 6 ). Adding sFlt to the model increased the AUC for prediction of neovascular AMD, but this difference did not meet statistical significance ( P = .097).
| AUC | SE | 95% CL for AUC | P Value a | |
|---|---|---|---|---|
| Full model: Sex + smoking Hx + sFlt level for neovascular vs early AMD where age ≥73 years | 0.76 | 0.05 | 0.65–0.87 | |
| Full model without sFLT | 0.68 | 0.06 | 0.55–0.81 | .097 |
a Difference in AUC for full model vs full model without sFlt.
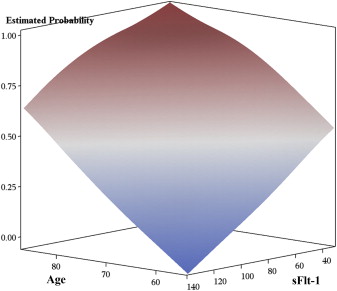
The predicted probability analyses for neovascular AMD vs early AMD from the above logistic regression are graphically represented in Figure 2 . As shown, rising age and declining serum sFlt-1 concentration are associated with neovascular AMD.
Serum Soluble Flt-1 <80 pg/mL Is Highly Associated With Neovascular Age-Related Macular Degeneration in Subjects Over 73 Years of Age
To clarify the potential clinical relevance, we categorized the data by patient age greater than or less than 73 years and patient serum sFlt-1 greater than or less than 80 pg/mL ( Table 7 ). From our analysis, serum sFlt <80 pg/mL has a very high association with neovascular AMD in the over-73 population. From Table 7 , we also calculated a more than 6-fold odds ratio for neovascular AMD in this subpopulation, relative to both no AMD and early AMD ( Table 8 ). This would seem to indicate a synergistic interaction between declining sFlt in the serum and rising age in raising the risk of neovascular AMD. Stratification by decade of life did not affect the statistically significant association between declining serum sFlt-1 and risk of neovascular AMD ( Supplemental Table , available at AJO.com ).
| Age ≥73 Years | Age <73 Years | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-AMD | Early AMD | Neovascular AMD | P Value | Non-AMD | Early AMD | Neovascular AMD | P Value | ||
| Serum sFlt-1 concentration | <80 pg/mL | 3 | 3 | 39 | <.001 | 17 | 13 | 16 | .196 |
| ≥80 pg/mL | 15 | 16 | 32 | 20 | 21 | 10 | |||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


