Purpose
To determine the functional and anatomic outcome of early surgical repair with vitrectomy and silicone oil in open-globe injuries with retinal detachment (RD).
Design
Retrospective consecutive interventional case series.
Methods
All patients with open-globe injuries with RD treated between 1997 and 2007 underwent primary repair including vitrectomy with silicone oil within 8 hours after presentation. For data analysis, patients were divided into 3 groups according to the BETT classification: Group 1, intraocular foreign body; Group 2, penetrating injury; Group 3, globe rupture. Outcome measures were final reading visual acuity (0.4 logMAR or better), final ambulatory visual acuity (1.6 logMAR or better), endophthalmitis, and postoperative proliferative vitreoretinopathy (PVR).
Results
Eighty-eight patients were included (Group 1, n = 13; Group 2, n = 36; Group 3, n = 39). Mean follow-up was 22 months (standard deviation [SD] = 23, range 6-107 months). Eight percent of patients retained reading vision without significant difference between the 3 groups. Fewer patients in Group 3 than in Group 1 or 2 retained ambulatory visual acuity (Group 1, 62%; Group 2, 64%; Group 3, 33%, P = .024). Endophthalmitis occurred in 3.4% of eyes (1 eye in each group). PVR grade B-C, type 1–3 developed in 44% of patients without significant difference between the 3 groups. Re-RD occurred in 38% of eyes.
Conclusions
Few patients achieved reading vision while 50% of patients retained ambulatory visual acuity. Final visual outcome is related to the severity of the injury. The frequency of postoperative endophthalmitis is low. Postoperative development of advanced PVR is avoided in most patients.
Ocular trauma of the posterior segment is a significant cause of visual loss. In the past, the prognosis for vision following such injuries was poor. Modern closed intraocular surgical techniques have transformed the management of ocular trauma and allowed salvage of vision in many previously hopeless cases. Visual prognosis is often dictated by the mechanism and location of injury, extent of initial damage, and the presenting visual acuity. Open-globe injuries with rhegmatogenous retinal detachment (RD) are a subgroup of particularly severe injuries that can be expected to have an even worse prognosis than open-globe injuries involving the posterior segment without RD. Despite a general consensus about the indication for the use of vitrectomy in this type of injury, the timing of the intervention and the type of primary tamponade (gas or silicone oil) remains controversial. The rationale of our therapeutic approach of an early comprehensive surgical repair including vitrectomy was to minimize the rate of posttraumatic endophthalmitis and to reduce early development of proliferative vitreoretinopathy (PVR) in the posttraumatic phase, which may occur in the more commonly applied 2-step approach between early primary wound closure and delayed vitrectomy. The rationale for the instillation of silicone oil as a primary tamponade was to confine the progression of PVR in the postoperative phase.
The purpose of this retrospective study was to determine the functional and anatomic outcome of open-globe injuries with RD in different types of ocular injury treated with early comprehensive surgical repair including vitrectomy and instillation of silicone oil.
Patients and Methods
The medical records of all patients with open-globe injuries involving the posterior segment with RD treated at the Eye Hospital of the University of Regensburg between January 1997 and December 2007 were reviewed. Age, sex, time interval between trauma and presentation to our hospital, length of follow-up (minimum 6 months), best-corrected Snellen visual acuity at presentation and at last follow-up, and the outcome measures were recorded. All patients were operated by an experienced vitreoretinal trauma surgeon at the earliest opportunity within 8 hours after first presentation. The operating surgeon based decisions regarding type of intervention on injury severity. The comprehensive surgical procedure included, as required, corneal suture, scleral suture, and removal of the lens with or without intraocular lens implantation. All patients underwent standard 20-gauge 3-port vitrectomy with or without intraocular foreign body (IOFB) removal, cryopexy, or laser retinopexy. All patients received silicone oil (Oxane 5700; Bausch&Lomb, Rochester, New York, USA) as primary tamponade. All patients received topical antibiotics and intravenous ceftriaxon and vancomycin for 3 to 7 days followed by oral cefaclor for 10 to 14 days. Intravitreal antibiotics were not applied. Primary enucleations were not performed. In case of re-detachment all patients underwent re-vitrectomy with membrane peeling in case of PVR membranes when possible, retinectomy and encircling band when needed, and reinfusion of silicone oil.
For data analysis patients were divided into 3 groups according to the standardized BETT classification : Group 1, intraocular foreign body; Group 2, penetrating injury; Group 3, globe rupture.
The outcome measures were: 1) number of patients with final reading visual acuity (0.4 logMAR or better), 2) number of patients with final ambulatory visual acuity (1.6 logMAR or better), 3) number of patients with endophthalmitis, and 4) number of patients with PVR.
Other recorded patient data were location of entrance or impact wound, number of retinal breaks, retinal tear ≥3 clock hours, macula-off detachment, vitreous hemorrhage, endophthalmitis, traumatic aniridia, retinectomy, additional procedures at initial repair, frequency of re-detachment, time to re-detachment, additional procedures at repair of re-RD, final cornea status (clear, keratoplasty, corneal scar), final lens status (clear lens, traumatic cataract, pseudophakia, aphakia), silicone oil at last follow-up, phthisis bulbi, enucleation, and total number of microsurgical operations.
Diagnosis of PVR was based on the standardized classification of Machemer and associates. For this study, any grade B or C of postoperative PVR developing over any clock hour made the diagnosis of PVR.
Statistical Methods
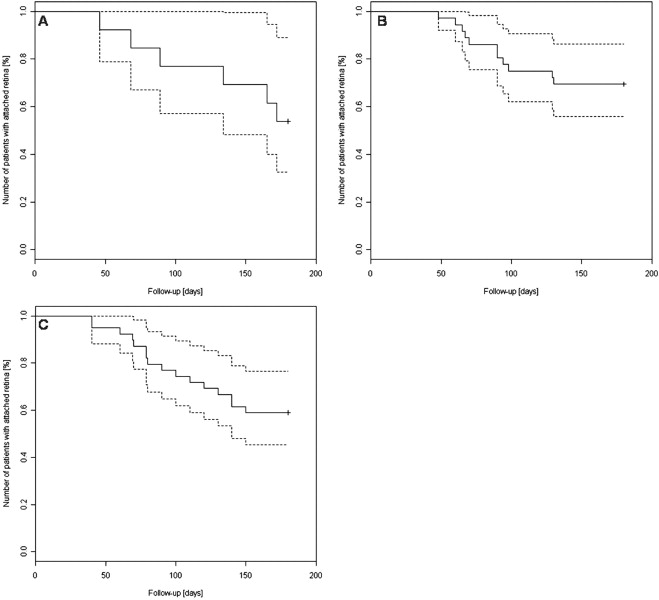
The χ 2 test was performed to analyze the outcome measures. P values below .05 were considered statistically significant. If there was a significant difference between the 3 patient groups, Fisher exact test with Bonferroni correction for multiple testing was used for pairwise comparison. To investigate whether any of the preoperative characteristics—group, time interval between trauma and presentation, preoperative ambulatory visual acuity (“ambulatory visual acuity preop”), location of entrance/impact wound, number of retinal breaks, retinal tear ≥3 clock hours, macula-off detachment, or traumatic aniridia—were related to the outcome measure postoperative ambulatory visual acuity (“ambulatory visual acuity postop”), a predictive logistic regression model with backward selection (Wald statistic) was calculated. The same model was used to test whether group, time interval between trauma and presentation, ambulatory visual acuity preop, number of retinal breaks, retinal tear ≥3 clock hours, or macula-off detachment were related to the outcome measure postoperative proliferative vitreoretinopathy (“PVR postop”). The analyses were performed by using the PASW Statistic 18 (Version 18.0.2; SPSS Inc, Chicago, Illinois, USA). The survival curves with 95% confidence intervals for re-detachment ( Figure ) were generated with R 2.1.0 statistical software (URL http://www.R-project.org ).
Results
The patient data are summarized in Tables 1 and 2 . A total of 88 patients were included (Group 1, n = 13; Group 2, n = 36; Group 3, n = 39). Patients were predominantly male (82%; 72/88) with a mean age of 50 years (SD = 20, range 7–96). Mean follow-up was 22 months (SD = 23, range 6–107 months). Patients presented 4 to 12 hours after trauma, with a mean of 7.2 hours. A total of 2.3% (2/88) of patients presented with reading vision and 16% (14/88) with ambulatory visual acuity. Clinical signs of endophthalmitis were not observed at presentation. There were no perforating (formerly named double-penetrating) ocular injuries.
| Characteristics | Group 1 (IOFB) | Group 2 (Pentrating Injury) | Group 3 (Globe Rupture) | All Groups | P Value |
|---|---|---|---|---|---|
| No. of patients | 13 | 36 | 39 | 88 | |
| Age (years, mean, SD, range) | 54 (15) | 44 (18) | 54 (23) | 50 (20) | >.05 |
| 33–77 | 7–72 | 17–96 | 7–96 | ||
| Sex | 12 male | 32 male | 28 male | 72 male | >.05 |
| 1 female | 4 female | 11 female | 16 female | ||
| Time interval between trauma and presentation (hours, mean, SD, range) | 7.5 (1.9) | 7.3 (1.5) | 6.9 (1.9) | 7.2 (1.7) | >.05 |
| 5–11 | 5–11 | 4–12 | 4–12 | ||
| Reading vision a preop | 1 (8%) | 1 (3%) | 0 | 2 (2.3%) | >.05 |
| Ambulatory visual acuity b preop | 4 (31%) | 7 (19%) | 3 (8%) | 14 (16%) | >.05 |
| Location of entrance/impact wound (cornea or sclera or both?) | 6 cornea | 8 cornea | 5 cornea | 19 cornea | >.05 |
| 5 sclera | 12 sclera | 21 sclera | 38 sclera | ||
| 2 both | 16 both | 13 both | 31 both | ||
| No. of retinal breaks (mean, SD, range) | 2 (1.3) | 2.2 (0.9) | 2.4 (0.9) | 2.3 (1) | >.05 |
| 1–5 | 1–4 | 2–5 | 1–5 | ||
| Retinal tear ≥3 clock hours | 2 (15%) | 10 (28%) | 11 (28%) | 23 (26%) | >.05 |
| Macula-off detachment | 9 (69%) | 24 (67%) | 34 (87%) | 67 (76%) | >.05 |
| Vitreous hemorrhage | 12 (92%) | 36 (100%) | 39 (100%) | 87 (99%) | >.05 |
| Traumatic aniridia | 1 (8%) | 4 (11%) | 6 (15%) | 11 (13%) | >.05 |
a Reading vision = 0.4 logMAR or better.
| Group 1 (IOFB) | Group 2 (Pentrating Injury) | Group 3 (Globe Rupture) | All Groups | P Value | |
|---|---|---|---|---|---|
| No. of patients | 13 | 36 | 39 | 88 | |
| Follow-up (months, mean, SD, range) | 33 (29) | 22 (22) | 20 (21) | 22 (23) | >.05 |
| 6–86 | 6–88 | 6–107 | 6–107 | ||
| Reading vision a postop | 1 (8%) | 4 (11%) | 2 (5%) | 7 (8%) | >.05 |
| Ambulatory visual acuity b postop | 8 (62%) | 23 (64%) | 13 (33%) | 44 (50%) | .024 (Group 2 vs 3) |
| Ambulatory visual acuity b postop in patients with retinectomy | 0 of 2 | 1 of 2 | 3 of 7 | 4 of 11 | >.05 |
| Additional procedures at initial repair | 8 corneal suture | 24 corneal suture | 18 corneal suture | 50 corneal suture | >.05 |
| 7 scleral suture | 28 scleral suture | 34 scleral suture | 69 scleral suture | ||
| 9 lensectomy | 27 lensectomy | 32 lensectomy | 68 lensectomy | ||
| PVR postop | 7 (54%) | 16 (44%) | 16 (41%) | 39 (44%) | >.05 |
| re-RD | 6 (46%) | 11 (31%) | 16 (41%) | 33 (38%) | >.05 |
| Time to re-RD (days, mean, SD, range) | 112 (52) | 86 (27) | 94 (35) | 94 (36) | >.05 |
| 46–172 | 48–130 | 40–150 | 40–172 | ||
| Additional procedures at repair of re-RD | 2 retinectomy | 2 retinectomy | 7 retinectomy | 11 retinectomy | >.05 |
| 4 encircling band | 8 encircling band | 13 encircling band | 25 encircling band | ||
| Endophthalmitis | 1 (8%) | 1 (3%) | 1 (3%) | 3 (3.4%) | >.05 |
| Final cornea status | 5 clear | 11 clear | 21 clear | 37 clear | >.05 |
| 7 scar | 21 scar | 14 scar | 42 scar | ||
| 1 Kp | 4 Kp | 4 Kp | 9 Kp | ||
| Final lens status | 7 pseudophakic | 17 pseudophakia | 10 pseudophakia | 34 pseudophakia | .04 (aphakia in Group 3 vs Groups 1 and 2), otherwise <.05 |
| 4 aphakic | 14 aphakic | 25 aphakic | 43 aphakic | ||
| 1 cataract | 3 cataract | 3 cataract | 7 cataract | ||
| 1 clear | 2 clear | 1 clear | 4 clear | ||
| Silicone oil at last follow-up | 6 (46%) | 15 (42%) | 22 (56%) | 43 (49%) | >.05 |
| Phthisis bulbi | 1 (8%) | 2 (6%) | 4 (10%) | 7 (8%) | >.05 |
| Enucleation | 1 (8%) | 1 (3%) | 1 (3%) | 3 (3.4%) | >.05 |
| Total number of microsurgical operations (mean, SD, range) | 2.4 (1.1) | 2.6 (1.3) | 2.4 (1.2) | 2.4 (1.2) | >.05 |
| 1–5 | 1–6 | 1–5 | 1–6 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


