Purpose
To study the morphologic characteristics of corneal nerves in patients with advanced keratoconus using the acetylcholinesterase technique in corneal whole mounts.
Design
Prospective, observational case series.
Methods
Fourteen corneal buttons from 14 keratoconic patients (9 males and 5 females; mean age, 34.3 years) who had undergone keratoplasty for advanced keratoconus and 6 corneal buttons from 6 normal corneas were included. Whole mounts were stained for acetylcholinesterase and were scanned with a novel digital pathology scanning microscope.
Results
Seventy-one percent of keratoconic corneas demonstrated central stromal nerve changes, which included thickening, tortuosity, nerve spouting, and overgrowth. The nerve changes ranged from early to extensive and could be separated into 3 different grades. The central stromal nerves were abnormally thicker (18.9 ± 14.7 μm) than in controls (8.11 ± 3.31 μm; P < .001). The thickness of peripheral stromal nerves (12.6 ± 3.1 μm) was similar to that of controls (14.86 ± 5.60 μm; P = .072). Subbasal nerves showed changes in the form of loss of radial orientation and increased tortuosity, especially at the cone apex. At the cone base, a concentric arrangement of subbasal nerves was found in 43% of cases. Localized thickenings of subbasal nerves also were observed at their origin from the bulbous terminations of sub-Bowman nerves. The terminal bulbs, too, were enlarged. The mean diameter of the subbasal nerves in keratoconus (4.11 ± 0.60 μm) did not differ from that of the controls (4.0 ± 0.61 μm; P = .422).
Conclusions
This study provides additional histologic evidence of the involvement of corneal nerves in keratoconus and suggests further that they may play a role in the pathophysiologic factors and progression of the disease.
Keratoconus is a bilateral noninflammatory corneal ectasia that principally develops in the second and third decades of life, with an incidence of approximately 1 per 2000 in the general population. The exact cause and pathogenesis remains poorly understood, although genetic, biochemical, and biomechanical factors have been implicated. The association of keratoconus to other corneal and systemic diseases also has been documented. The involvement of corneal nerves in the pathogenesis of keratoconus has not received attention in the past, and only the prominence and visibility of central corneal nerves have been reported as an early clinical sign of keratoconus.
Recent advances in corneal in vivo confocal imaging have provided new and interesting data on the microstructural alterations of the corneal tissue in keratoconus. Several in vivo confocal microscopy studies consistently have shown a significant derangement in the morphologic and morphometric features of central subbasal and stromal nerves.
In keeping with these in vivo confocal microscopy findings, Brooks and associates have demonstrated the involvement of corneal nerves in the progression of keratoconus using immunohistochemical analysis. Whether these changes are primary or secondary pathologic manifestations is not clear. However, one theory suggests that accelerated apoptosis and lysis of basal epithelial cells with the release of intracellular proteolytic enzymes are the key triggers of subsequent destructive events involving the underlying corneal tissue, including the nerves in the close vicinity of the affected area. Although this hypothesis could explain the reduction of central subbasal nerve density frequently reported in in vivo confocal microscopy investigations, other observations, like loss of the normal subbasal nerve organization and thickening of subbasal and stromal nerves, require other explanations.
The histochemical technique of acetylcholinesterase involving endogenous tissue cholinesterase has been proven to be an excellent technique for in vitro 3-dimensional visualization of nerves in corneal whole mounts of animal eyes. We recently published 2 studies describing several novel features of normal human corneal innervation and aberrant features in bullous keratopathy using the Karnovsky and Roots modification of this technique.
The aim of the current study was to use the above method to evaluate human corneal nerves in patients with advanced keratoconus. Corneal buttons freshly obtained after penetrating and deep anterior lamellar keratoplasty for advanced keratoconus were stained and studied by the novel NanoZoomer digital microscopy system (Hamamatsu, Hamamatsu City, Japan), enabling us to obtained detailed, panoramic, and high-magnification images of the corneal nerves in 3 dimensions.
Methods
Patients
Fourteen corneal buttons obtained from 14 keratoconic patients (9 males, 5 females; mean age, 34.3 years) who had undergone keratoplasty for advanced keratoconus, mainly as a result of poor vision that did not improved with contact lenses (CLs) or who were intolerant to CLs. The research was conducted at Nottingham University Hospital, United Kingdom, and ethical approval was obtained from the Nottingham Research Ethics Committee (REC no. 06/Q2403/46). Before surgery, patients were evaluated by taking a full history and by slit-lamp biomicroscopy examination. Only corneas demonstrating 1 or more of the following clinical signs were included: subepithelial or apical stroma scarring, stromal thinning, ectasia, Fleischer ring, Vogt striae, and Descemet membrane breaks. Pentacam examination (Oculus, Inc, Lynnwood, Washington, USA) of the corneas was performed to confirm the diagnosis and to provide an indication of the disease severity. The Pentacam software provides an objective topographic classification of keratoconus severity (from prestage keratoconus and mild keratoconus, KK-1, through to advanced keratoconus, KK-4) based on 8 indices derived from the anterior surface topography and corneal thickness progression. Patient demographic and clinical data are shown in Table 1 . Ten patients (72%) were white, 3 (21%) were Asian, and 1 (7%) was black. Eleven patients (79%) underwent deep anterior lamellar keratoplasty and 3 (21%) underwent full-thickness penetrating keratoplasty. All patients included in the study had keratoconus grade KK3 to KK4. The freshly obtained corneal buttons were subjected to the Karnovsky and Roots modification of acetylcholinesterase method for corneal nerve demonstration.
| Patient | Eye | Sex | Age (y) | Race | History of Hydrops | Apical Scarring | Duration of Disease (y) | Duration of Contact Lens Wear (y) | Thickening of the Terminal Bulbs | Aberrant Stromal Nerves/Grade | Grade of KCN (KK) | Procedure |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | R | M | 39 | White | − | − | 5 | 4 | + | −/NA | 3 to 4 | DALK |
| 2 | R | M | 18 | White | + | + | 1 | 0 | + | +/2 | 3 to 4 | DALK |
| 3 | L | M | 31 | Asian | − | − | 6 | 6 | + | +/1 | 3 to 4 | DALK |
| 4 | L | F | 31 | White | + | + | 5 | 2 | − | +/2 | 3 to 4 | DALK |
| 5 | R | M | 51 | White | − | + | 17 | 0 | − | +/2 | 4 | DALK |
| 6 | R | F | 24 | White | − | + | 3 | 3 | − | −/NA | 4 | DALK |
| 7 | L | M | 41 | White | − | + | 13 | 20 | + | +/2 | 4 | PKP |
| 8 | R | M | 63 | White | − | + | 21 | 25 | − | +/3 | 4 | DALK |
| 9 | R | F | 32 | Black | − | − | 18 | 10 | − | −/NA | 3 to 4 | DALK |
| 10 | R | M | 22 | Asian | − | + | 1.5 | 0 | + | +/2 | 3 to 4 | DALK |
| 11 | L | F | 36 | White | − | + | 5 | 0 | − | +/2 | 4 | PKP |
| 12 | L | F | 32 | Asian | + | + | 1.5 | 0 | − | +/1 | 4 | PKP |
| 13 | L | M | 18 | White | − | + | 2 | 1 | − | −/NA | 3 to 4 | DALK |
| 14 | L | M | 42 | White | − | − | 4 | 3 | − | +/1 | 4 | DALK |
Acetylcholinesterase Method for Corneal Nerve Demonstration
The method has been described in detail previously. Briefly, corneal buttons were fixed in cold 4% formaldehyde (pH 7) for 4 hours and then rinsed overnight in phosphate buffered saline. Specimens were incubated in the stock solution containing acetylthiocholine iodide as a substrate for 24 hours at 37 C. The acetylcholinesterase enzyme in the nerves reacted with acetylthiocholine iodide in the substrate to produce a brown coloration of the nerves. The color was intensified with a dilute solution of ammonium sulfide. Specimens were dehydrated by immersion in alcohol and were cleared in xylene, as is standard for histologic preparation. The specimens finally were mounted between a slide and cover slip and were prepared for image analysis.
Image Analysis
The stained corneas were scanned en face using a Hamamatsu NanoZoomer digital pathology microscope system. The corneal buttons were examined at ×40 magnification in multilayers at 10-μm intervals. The images then were stacked and merged to give a single, holistic, detailed, anatomic view of the stained corneal nerves. A z-stacking software, AllFocus (AllFocus—Extended Depth of Field Software; Saphicon, Palo Alto, California, USA) was used for this purpose. Image analysis was carried out using the software provided by the manufacturer, and the areas of interest then were selected, automatically scaled and exported to JPEG format. Oil immersion technique using a light microscope (Leica DM4000B; Leica Microsystems, Nussloch, Germany) was used to examine the basal epithelial layer–Bowman zone interface at a higher magnification (×100). Adobe Photoshop CS4 (Adobe Systems, Inc, San Jose, California, USA) was required for additional image processing. Subbasal and stromal nerves were evaluated qualitatively and quantitatively in the study and control groups. Three measurements of the width of the central and peripheral stromal and subbasal nerves were obtained from each cornea in study and control groups. For the measurement of the terminal bulb size, the widest diameter was considered.
Statistical Testing
Data were analyzed using an analysis tool pack for Microsoft Excel 2007 (Microsoft Corp, Redmond, Washington, USA) and SPSS software version 16.0 (SPSS, Inc, Chicago, Illinois, USA). A P value of < .05 was taken as the threshold of statistical significance. The Student t test for independent samples was used to establish whether any differences in the peripheral stromal nerve diameter between the normal subjects and keratoconic patients were significant. It also was used to test the difference in the terminal bulb size and main subbasal nerve diameter. The Mann–Whitney U test was used to test the difference in the central stromal nerve diameters in keratoconic patients and controls.
Control
Six fresh postmortem corneas donated with family consent from 3 deceased patients (2 males, 1 female; mean age, 57.3 years) with no previous ocular pathologic features or surgery also were stained with the acetylcholinesterase technique and used as controls. Causes of death were metastatic prostate carcinoma, adenocarcinoma of the lung, and postrenal transplantation sepsis.
Results
Control Corneas
All corneas from the control group showed the normal architecture of nerves described in detail previously using the same technique. Briefly, thick nerve bundles enter the corneal limbus in an equal distribution around the circumference and move randomly toward the central cornea. As they move from the periphery toward the center of the cornea, these large stromal nerve trunks divide dichotomously or trichotomously into thinner nerve branches. The mean stromal nerve diameter was 8.11 ± 3.31 μm in the central cornea and 14.86 ± 5.60 μm at the periphery. In the anterior stroma, nerves showed a characteristic budding and branching pattern predominantly at the midperipheral zone of the cornea. After passing through the Bowman zone, they were noted to terminate into bulb-like thickenings from which multiple subbasal nerves arose. The average size of the bulb was 10.66 ± 2.52 μm. The perforation sites mainly were located in the midperipheral cornea. Subbasal nerves from all quadrants converged toward the inferocentral cornea to form a characteristic clockwise whorl pattern. The mean diameter of the main subbasal nerves was 4.0 ± 0.61 μm. Illustrative images of normal nerve architecture are provided in the previous report.
Keratoconic Corneas
Corneas showed a significant alteration in the subbasal and stromal nerves at the corneal apex. However, peripheral stromal corneal innervation (outside the conal region) showed normal morphologic features in most cases similar to the architecture of nerves in the control subjects.
Stromal Nerves
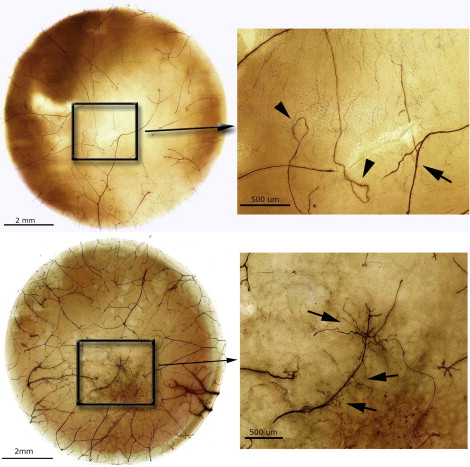
Stromal nerve changes were noted in the central cornea in 10 of 14 samples (71%). Nerve changes were classified into 3 grades based on the extent and severity of the morphologic alterations. In grade 1, mild changes were observed in the form of mild looping and coiling of the central stromal nerves ( Figure 1 , Top row). In grade 2, abnormal growth of nerves showing advanced tortuosity, looping, and coiling with characteristic sprouting of smaller nerve bundles from the main stromal trunks were seen ( Figure 1 , Bottom row). They were of irregular size and bizarre orientation. In grade 3, exuberant overgrowth of tortuous nerves within the central cornea was seen that formed a very complex network. A notable reduction in the paracentral stromal innervation was seen ( Figure 2 ). Three of 10 (30%) patients had grade 1 nerve changes, 6 (60%) had grade 2 changes, and only 1 (10%) demonstrated grade 3 changes.

The central stromal nerves were thick and densely stained. The thickness of central stromal nerves was 18.9 ± 14.7 μm and was thicker than the central stromal nerves in the controls (8.11 ± 3.31 μm; P < .001; Figure 3 , Top left and right). Some of these nerves were very thick and measured at 92.6 μm in diameter along their course, reaching up to 157 μm in diameter at the region of bifurcation ( Figure 3 , Middle left). The thickness of peripheral stromal nerves was 12.6 ± 3.1 μm and was not statistically different from the peripheral stromal nerve diameter in the controls (14.86 ± 5.60 μm; P = .072; Figure 3 , Middle right and Bottom left and right). In most of the cases, patchy networks of thin, tortuous subepithelial nerves were observed in the anterior stroma mainly in the paracentral region.

Eighty percent of patients (n = 8) with aberrant stromal nerves had clinical evidence of central scarring and only 30% (n = 3) had history of acute corneal hydrops. In patients with normal stromal nerves by histologic analysis, 2 of 4 had central scarring. No history of hydrops was noted in this group. The mean duration of disease since diagnosis in patients with aberrant stromal nerves was 7.5 ± 7.0 years and in those without stromal nerve changes, the duration was 7.0 ± 7.4 years. Five patients, who demonstrated abnormal stromal nerves by histologic analysis, did not use CLs during their course of management because of problems with lens fitting. The mean duration of CL wear in the remaining 5 patients with aberrant stromal nerves was 11.2 ± 10.56 years. Patients without nerve alterations by histologic analysis had a mean duration of 4.5 ± 3.87 years of CL use.
Subbasal Nerves
Subbasal nerve organization was abnormal in all patients. Subbasal nerves showed loss of their radial orientation and demonstrated a characteristic multidirectional radiation at the point of their origin from the terminal bulbs ( Figure 4 ). Most of these nerves also had a very tortuous course ( Figure 5 , Top left and right). Localized thickenings of subbasal nerves often were observed at their origin from the terminal bulbs ( Figure 5 , Middle left, and Figure 6 ), along their course ( Figure 5 , Middle right), or both. In 5 patients, the terminal bulb itself was found to be enlarged and its mean diameter was measured at 14.60 ± 5.08 μm, the largest being of 24 μm in diameter ( Figure 6 ). This was significantly larger than the width of the terminal bulbs in the controls ( P = .006). However, most of these nerves and their bulbous terminations were of normal thickness ( Figure 5 , Bottom left and right, and Figure 7 ). The diameter of the main subbasal nerves was measured at 4.11 ± 0.60 μm and was comparable with that in the controls ( P = .422).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


