Purpose
To investigate the optimal amount of safe under-correction in patients with refractive accommodative esotropia.
Design
Prospective noncomparative interventional case series.
Methods
Patients with refractive accommodative esotropia wore trial glasses based on cycloplegic refraction, then −0.25 diopters (D) of minus sphere lenses were placed on both lenses of the trial glasses and the deviation was measured. Minus spheres of −0.25 D were continuously added until the angle of deviation increased; the minus spheres added just before the deviation increase were defined as the maximal tolerable amount of under-correction. A total of 38 patients were prescribed under-corrected spectacles up to −1.5 D and followed for 6 months.
Results
Thirty-one patients underwent the maximal tolerable amount of under-correction and 7 underwent −1.5 D of under-correction. A mean −0.89 D of under-correction was performed. We observed no deterioration in visual acuity, stereoacuity, or fusional ability during the follow-up period in any of the patients. Small increase in the angle of deviation of 2 prism diopters was noted in 2 patients. The mean spherical equivalent refractive error of both eyes ( P = .012) and age of onset ( P = .006) showed strong positive correlations with the maximal tolerable amount of under-correction.
Conclusions
A reduction in hyperopic correction by the maximal tolerable amount of under-correction was performed without notable short-term side effects. The spherical equivalent refractive error and age of onset appear to be useful clinical indices in determining the appropriate amount of under-correction.
Accommodative esotropia is a common type of childhood esodeviation. Misalignment of the eyes in patients with accommodative esotropia is closely related to hyperopia and using spectacles to correct refractive errors can reduce or completely resolve eye misalignment. However, the full correction of hyperopia has been suspected as a cause of impeded emmetropization in accommodative esotropes. Animal studies have shown that spectacle lenses can alter eye growth, resulting in compensatory refractive changes. In human studies, various authors observed an association between spectacle use and a relatively small decrease in hyperopia, and 1 clinical study suggested that gradual under-correction may help wean patients from spectacles by increasing divergence amplitudes.
However, possible negative impact of under-correction has also been investigated. In a recent prospective study of 30 patients, decompensation of esotropia was noted in many patients prescribed spectacles under-corrected by 1.0 to 2.0 diopters (D). The authors of that study suggested that the maximum hyperopic correction should be prescribed in order to control the deviation and to promote the potential restoration and continued development of binocular single vision. In another report, under-correction did not result in a faster decrease in hyperopia in children with accommodative esotropia. Furthermore, several studies have suggested that strabismic eyes have different patterns of refractive change than nonstrabismic eyes and that the etiology of impeded emmetropization is not attributable to wearing spectacles, but rather the innate characteristics of strabismic eyes.
The hypothesis regarding the positive role of under-correction has not yet achieved strong universal acceptance. However, it is possible that under-correction may have a valid role in some cases and therefore merits further investigation.
The scientific basis regarding the optimal amount of under-correction has not yet been firmly established. The method of under-correction is usually determined on an ad hoc basis at the discretion of individual clinicians, primarily based on previous experience. The purpose of this study was to evaluate the question “How much reduction can be performed without producing side effects?” We prospectively evaluated the maximal tolerable amount of under-correction and its short-term safety in a series of patients with refractive accommodative esotropia. We discuss both the appropriate amount of under-correction and other factors to consider for safe under-correction.
Methods
Forty-one patients with refractive accommodative esotropia were recruited prospectively between May 1, 2009 and November 30, 2009. Patients with +1.5 D or more of hyperopia and a corrected esophoria or esotropia of no more than 8 prism diopters (PD) at both distance and near with the use of fully corrected hyperopic spectacles were considered for inclusion in this study. Patients with any of the following conditions were excluded: age less than 3 or greater than 10 years; inability to complete visual acuity testing; presence of amblyopia; no measurable stereoacuity; presence of suppression or diplopia on the Worth 4-Dot test; less than 1 year of spectacle use; use of bifocal glasses; anisometropia of more than 1.0 D; more than 2 PD of change in angle of esophoria or esotropia within 1 year; other forms of strabismus including vertical deviation; previous extraocular muscle surgery; developmental delay; any form of neurologic impairment; or other diseases of the visual pathways.
All patients underwent a full ophthalmologic assessment including visual acuity testing, slit-lamp biomicroscopy, fundus examination, evaluation of ocular alignment status, and tests for fusion and stereoacuity. The corrected visual acuities were transformed to a logarithmic scale (logMAR) for statistical analysis. Fusion was tested with the Worth 4-Dot test at near (33 cm) and stereoacuity was tested with the Titmus stereo test (both fly and circles). The stereoacuities were converted to a logarithmic scale for statistical analysis. A significant change in stereoacuity was defined as a change of 0.6 or more log seconds of arc. The AC/A ratio was calculated using the heterophoria method: AC/A = PD + ([N – D]/K), where PD is the interpupillary distance in cm, N is the deviation at near, D is the deviation at distance, and K is the near fixation distance in diopters (normal range: 5 to 6 Δ/D). Amblyopia was defined as an inter-eye difference in best-corrected visual acuity (BCVA) of 2 or more logMAR lines.
In all patients, ocular alignment was tested by the cover test, cover-uncover test, and the prism and alternate cover test at 6 m fixation and at 33 cm fixation. For fixation a 6/9 visual acuity symbol was used. All tests for ocular alignment were performed with and without hyperopic correction by a single examiner (S.Y.O.). Cycloplegic refractions were performed using retinoscopy 60 minutes after the instillation of 1% cyclopentolate and 0.5% tropicamide.
Estimation of the potential effect of under-correction was performed 5 to 7 days after cycloplegic refraction. After the patient had worn trial glasses based on cycloplegic refraction, −0.25 D of minus sphere lenses were placed simultaneously on both lenses of the trial glasses and the deviation for distance and near was measured. Minus spheres of −0.25 D were continuously added until the angle of esophoria or esotropia increased; the amount of minus spheres added just before the increase in deviation was observed was defined as the maximal tolerable amount of under-correction. To estimate the correlation between each patient’s spherical equivalent (SE) refractive error and the amount of maximal tolerable under-correction, we defined the mean SE refractive error of both eyes as the “baseline SE refractive error.”
A reduction in hyperopic correction by the maximal tolerable amount of under-correction from full cycloplegic refractive error was prescribed for the patients’ spectacles. The maximal amount of under-correction did not exceed −1.5 D, even if a patient tolerated more, to avoid unexpected side effects. Astigmatic refractive error was fully prescribed for all patients.
Follow-up examinations were scheduled at 1 week, 1 month, 3 months, and 6 months after the patients began wearing under-corrected spectacles. At every visit, symptoms such as asthenopia, diplopia, or blurred vision were documented and ocular examinations, including visual acuity and ocular alignment status for distance and near, were performed. Tests of fusion and stereoacuity were performed at the 1-month, 3-month, and 6-month follow-up visits. Cessation of under-corrected spectacles was considered under any of the following conditions: a significant deterioration in stereoacuity, loss of fusion, more than 2 PD of increase in esophoria or esotropia with correction, more than 1 logMAR line decrease in visual acuity, or more than 1 week of prolonged asthenopia.
Data were analyzed using SPSS software version 11.0 for Windows (SPSS, Inc, Chicago, Illinois, USA). To compare visual acuity, ocular alignment, and stereoacuity between baseline and 6 months, 95% confidence intervals were estimated using the Wilcoxon signed rank test. To investigate the relationship between possible factors and the maximal tolerable amount of under-correction, we performed Spearman correlation tests and multivariable analyses. A P value less than .05 was regarded as statistically significant.
Results
Of the 41 subjects enrolled, 39 were included in the results analysis; 2 participants were excluded because they were lost to follow-up. The mean patient age was 6.9 ± 2.5 years (mean ± standard deviation; range 3 to 10 years). Nineteen patients (48.7%) were male and 20 (51.3%) were female. The mean age of onset noted by parents was 28.8 ± 16.8 months (range 4 to 72 months) and the patients underwent confirmatory examination by ophthalmologists at a mean age of 36.6 ± 16.7 months (range 7 to 74 months). The mean SE refractive error was +4.25 ± 1.53 D (range +1.50 to +7.50 D) for right eyes and +3.91 ± 1.54 D (range +1.50 to +8.00 D) for left eyes. The mean astigmatism was 0.73 ± 0.56 D (range 0.00 to 1.75 D) for right eyes and 0.51 ± 0.57 D (range 0.00 to 1.75 D) for left eyes. The mean AC/A ratio was 5.41 ± 0.59/1 Δ/D (range 4.70 to 7.67 Δ/D). The mean logMAR visual acuity was 0.03 ± 0.05 (range 0.00 to 0.15) in right eyes and 0.03 ± 0.05 (range 0.00 to 0.15) in left eyes. Seventeen patients (43.6%) had a stereoacuity of 100 seconds of arc or better, 14 (35.9%) had less than 100 to 400 seconds of arc, and the remaining 8 patients (20.6%) had 800 to 3000 seconds of arc. The mean deviation with and without glasses at distance was 1.7 ± 2.6 PD (range 0 to 8 PD) and 24.2 ± 9.8 PD (range 12 to 50 PD), respectively. The mean deviation with and without glasses at near was 2.1 ± 2.7 PD (range 0 to 8 PD) and 24.6 ± 9.9 PD (range 12 to 50 PD), respectively.
Table 1 displays the results of progressive under-correction with trial lenses. More patients with an increased angle of deviation at distance or near were noted as the degree of under-correction increased. One patient failed to tolerate −0.25 D of under-correction and was prescribed fully corrected hyperopic glasses. Seven patients tolerated more than −1.5 D of under-correction and were prescribed −1.5 D under-corrected spectacles. The maximal tolerable amount of under-correction was performed for 31 patients. As a result, a mean −0.89 D of under-correction was performed for 38 patients.
| Amount of under-correction (diopter) | −0.25 | −0.5 | −0.75 | −1.0 | −1.5 | −2.0 |
| Number (%) of patients with increased angle of deviation | 1 (2.6%) | 5 (12.8%) | 12 (30.8%) | 22 (56.4%) | 31 (79.5%) | 36 (92.3%) |
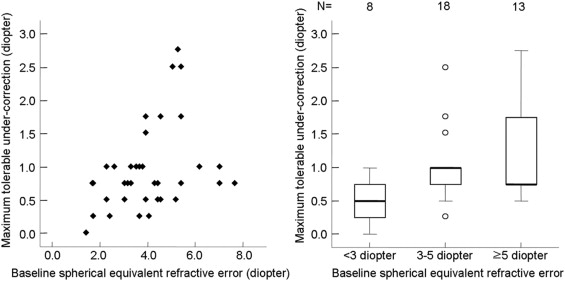
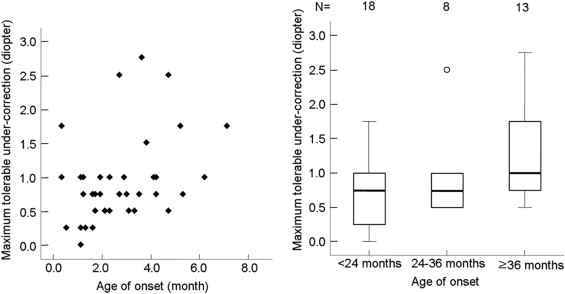
Table 2 shows the correlation of baseline characteristics with maximum tolerable amount of under-correction. The maximum tolerable amount of under-correction was greater in patients with the following conditions: greater baseline SE refractive error ( Figure 1 ), later age of onset ( Figure 2 ), orthotropia with hyperopic correction, and a smaller angle of deviation without hyperopic correction. In the multivariable model, factors significantly associated with the maximum tolerable amount of under-correction included the mean baseline SE refractive error and age of onset ( Table 3 ). Patients with a greater baseline SE refractive error and later age of onset tolerated more under-correction.
| Baseline Characteristics | No. | Maximum Tolerable Under-correction (D) | r | P Value |
|---|---|---|---|---|
| Sex | −0.002 | .989 | ||
| Female | 20 | 0.95 ± 0.60 (0.25-2.75) | ||
| Male | 19 | 0.97 ± 0.70 (0.00-2.50) | ||
| Age (years) | −0.021 | .901 | ||
| <5 | 9 | 0.89 ± 0.65 (0.25-2.50) | ||
| 5-8 | 18 | 1.04 ± 0.60 (0.25-2.50) | ||
| ≥9 | 12 | 0.90 ± 0.73 (0.00-2.75) | ||
| Onset (months) | 0.455 | .004 | ||
| <24 | 18 | 0.68 ± 0.42 (0.00-1.75) | ||
| 24-36 | 8 | 0.94 ± 0.66 (0.50-2.50) | ||
| ≥36 | 13 | 1.37 ± 0.70 (0.50-2.75) | ||
| Baseline SE refractive error (D) | 0.361 | .024 | ||
| <3 | 8 | 0.50 ± 0.33 (0.00-1.00) | ||
| 3-5 | 18 | 1.01 ± 0.57 (0.25-2.50) | ||
| ≥5 | 13 | 1.19 ± 0.76 (0.50-2.75) | ||
| Stereopsis (log seconds) | −0.114 | .489 | ||
| <2 | 10 | 1.10 ± 0.83 (0.00-2.75) | ||
| 2-3 | 23 | 0.97 ± 0.62 (0.25-2.50) | ||
| ≥3 | 6 | 0.71 ± 0.29 (0.25-1.00) | ||
| Angle of deviation with glasses (PD) | −0.385 | .016 | ||
| Orthotropia | 25 | 1.12 ± 0.70 (0.00-2.75) | ||
| >0 | 14 | 0.68 ± 0.39 (0.25-1.75) | ||
| Angle of deviation without glasses (PD) | −0.417 | .008 | ||
| <20 | 13 | 1.27 ± 0.73 (0.25-2.75) | ||
| 20-30 | 16 | 0.91 ± 0.64 (0.00-2.50) | ||
| ≥30 | 10 | 0.65 ± 0.29 (0.25-1.00) | ||
| AC/A ratio (ΔA/D) | 0.058 | .726 | ||
| <5 | 12 | 0.92 ± 0.62 (0.25-2.50) | ||
| 5-5.5 | 9 | 1.06 ± 0.76 (0.25-2.75) | ||
| ≥5.5 | 18 | 0.94 ± 0.62 (0.00-2.50) | ||
| Baseline Characteristics | Estimate | t | P Value |
|---|---|---|---|
| Sex | 0.09 | 0.55 | .585 |
| Age | 0.07 | 0.36 | .720 |
| Onset | 0.48 | 3.01 | .006 |
| Baseline SE refractive error | 0.46 | 2.74 | .012 |
| Stereopsis | 0.12 | 0.67 | .508 |
| Angle of deviation with glasses | −0.16 | −0.92 | .368 |
| Angle of deviation without glasses | −0.31 | −1.68 | .106 |
| AC/A ratio | 0.01 | 0.05 | .963 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


