Purpose
To investigate whether Fourier-domain (FD) optical coherence tomography (OCT) can measure the tear meniscus of anophthalmic patients using prosthetic eyes and to compare the characteristics of normal and artificial eyes.
Design
Prospective, nonrandomized, observational case series.
Methods
Thirty-one patients who had undergone anophthalmic surgery in 1 eye and had been wearing artificial eyes for more than 6 months were included. Subjects with socket inflammation, contracted sockets, or other known lid disorders were excluded. Patients were asked to complete a questionnaire regarding their demographic status and dry eye symptoms before treatment, and FD OCT scanning and the Schirmer test were performed. Three images were obtained by FD OCT on each normal and anophthalmic eye, and the tear meniscus height, tear meniscus depth, and tear meniscus angle were measured with computer calipers.
Results
FD OCT was able to visualize the tear meniscus of both normal and artificial eyes. The mean tear meniscus height of artificial eyes was significantly lower than that of normal eyes (200.59 ± 79.68 μm vs 261.24 ± 86.17 μm; P < .001). Mean tear meniscus depth, tear meniscus area, and tear meniscus volume also were significantly lower in artificial eyes than in normal eyes. The dry eye symptom score showed significantly negative correlation with tear meniscus height. The Schirmer test results correlated with tear meniscus parameters in normal eyes, but not in artificial eyes.
Conclusions
FD OCT is a valuable clinical tool in the evaluation of tear meniscus height in normal and artificial eyes. In addition, tear meniscus height can be a useful clinical parameter that estimates symptoms of ocular dryness and discomfort in both normal and artificial eyes.
Many anophthalmic patients wearing prosthetic eyes report varying degrees of dryness and discomfort. This may be caused by roughened prosthesis surfaces, glutinous surface deposits, and infection of the anophthalmic socket. However, some patients continue to experience dryness and discomfort even if the above causes have been eliminated. Allen and associates suggested that tear insufficiency may be another cause of discomfort for those patients. They conducted a study using the Schirmer I and Schirmer II tests and reported that anophthalmic patients have less tears in the anophthalmic socket in comparison with their normal side because of the absence of a tear reflex. They found severe tear deficiencies in up to 50% of patients with anophthalmic sockets.
However, there have been no recent studies that examined tear deficiency in anophthalmic patients despite new developments in dry eye diagnostic methods. Minimally invasive objective tests recently have been introduced that enhance our ability to diagnose dry eye. The new testing methods include tear interferometry, tear evaporimetry, and tear meniscus height evaluation.
The evaluation of tear meniscus height is an easily accessible and noninvasive indirect measure of tear volume and also provides valuable diagnostic information to the clinician on lacrimal gland function and drainage and patency of the nasolacrimal route. Several techniques have been used to measure tear meniscus height, including slit-lamp evaluation, image capture methods, and more recently, optical coherence tomography (OCT). The application of OCT has evolved to include the evaluation of anterior structures such as the cornea, limbus, the tear film, and tear meniscus height with the increasing popularity of OCT in the ophthalmic field. In addition, a newly developed technology called Fourier-domain (FD) OCT has enabled much faster image acquisition with higher definition. The purpose of this study was to investigate whether FD OCT can provide objective information about the tear meniscus in anophthalmic patients using prosthetic eyes and about characteristics of artificial eyes in comparison with normal eyes.
Methods
Thirty-one patients (14 males, 17 females; mean age, 41.5 ± 17.9 years; range, 16 to 69 years) were included in this prospective study. All subjects had undergone evisceration (18 eyes) or enucleation (13 eyes) in 1 eye and had been wearing carefully fitted prosthetic eyes for more than 6 months. Subjects with socket inflammation, contracted sockets, or other known organic lid disorders were excluded. The contralateral eyes in all patients were healthy and served as an internal normal control.
Patients were asked to complete a questionnaire regarding their demographic status, ophthalmic operations, duration of prosthesis use, and ophthalmic treatments. Patients reported the frequency of symptoms related to dry eye such as pain, grittiness, dryness, feeling of the eyelid sticking shut, and sensitivity to windy conditions or in an air-conditioned area at one of the following 5 grades: none of the time (0), some of the time (1), half of the time (2), most of the time (3), and all of the time (4). The questionnaire was based on the ocular surface disease index, with some alterations to be more applicable to anophthalmic eyes. The final dry eye symptom score was calculated by the total sum of the scores.
A high-speed, high-resolution, FD OCT (RTVue; Optovue Inc., Fremont, California, USA) was used to perform a vertical 2-mm scan across the lower tear meniscus below the center of the cornea at the 6-o’clock position. We used a scan angle of 90 degrees in which a vertical beam originated from the cornea and scanned downward toward the lid margin. Three images per eye were obtained by the same examiner (S.E.K.). Each participant was instructed to fixate an external fixation target positioned in primary gaze. The participants were instructed to blink normally so as to distribute the tear film evenly and to minimize ocular surface dehydration. Just before obtaining measurements, the participants were asked to refrain from blinking during the acquisition of the scan. The OCT scans were obtained from the normal and anophthalmic eye in the same manner. OCT settings remained constant throughout the experiment for all subjects.
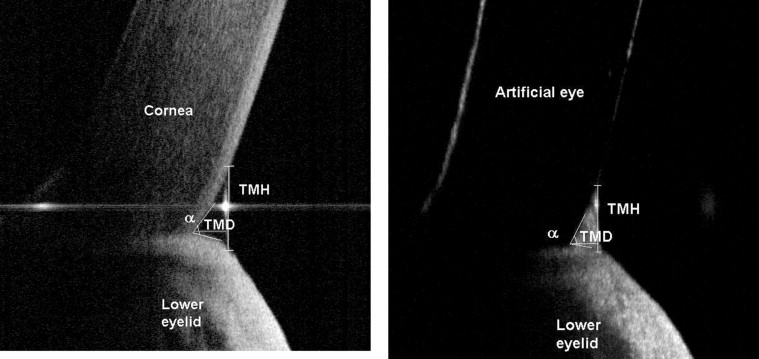
The tear meniscus height (TMH), tear meniscus depth, and tear meniscus angle (a) were measured with a computer caliper. The tear meniscus area was calculated by the formula based on a triangular approximation (tear meniscus area = 0.5 × tear meniscus height × tear meniscus depth; Figure 1 ). The estimation of tear meniscus volume was obtained by multiplying the tear meniscus area and eyelid length, assuming the tear meniscus was uniform across the entire eyelid. This protocol was also used by Mainstone and associates.
After OCT scanning, a Schirmer I test (without anesthesia) was performed on both normal and artificial eyes. A filter paper strip was placed in the lower fornix near the lateral canthus to avoid corneal stimulation and was left in place for 5 minutes. Subjects were asked to blink normally during the procedure. After 5 minutes, the filter paper was removed and the amount of wetting was measured in millimeters.
Data were analyzed using SPSS software version 15.0 (SPSS Inc., Chicago, Illinois, USA). Comparisons of mean values, such as tear meniscus height, tear meniscus depth, tear meniscus angle, tear meniscus area, tear meniscus volume, dry eye symptom score, and Schirmer test results between normal and artificial eyes were performed using the paired t test. Correlations were analyzed using the Pearson correlation for parametric data and the Spearman correlation for nonparametric data. P values less than .05 was considered statistically significant.
Results
FD OCT was able to visualize the tear meniscus in both normal eyes and artificial eyes in all patients. Mean tear meniscus height, tear meniscus depth, tear meniscus area, and tear meniscus volume values were significantly lower in artificial eyes than in normal eyes. Tear meniscus angle did not differ significantly between the 2 groups ( Figure 2 ; Table 1 ).
| Variable | Normal Eyes (n = 31) | Artificial Eyes (n = 31) | P Value a |
|---|---|---|---|
| TMH (μm) | 261.24 ± 86.17 | 200.59 ± 79.68 | <.001 b |
| TMD (μm) | 192.71 ± 60.75 | 156.81 ± 63.90 | .002 b |
| TM angle (degree) | 53.97 ± 10.27 | 51.05 ± 9.29 | .084 |
| TMA (10 −9 m 2 ) | 27.60 ± 17.36 | 18.04 ± 14.25 | .001 b |
| TMV (nL) | 762.30 ± 462.47 | 480.95 ± 423.02 | .001 b |
Mean dry eye symptom score of the artificial eyes was 7.52 ± 2.79 (range, 3 to 14) and was 2.83 ± 2.63 (range, 0 to 11) in normal eyes. There was statistically significant difference in the dry eye symptom score between the normal and artificial eyes ( P < .001, paired t test).
The Schirmer I test showed 13.39 ± 12.17 mm in normal eye and 10.35 ± 9.44 mm in artificial eyes. There was no statistically significant difference in the Schirmer test score ( P = .090, paired t test).
In normal eyes, tear meniscus parameters by FD OCT measurement had a significantly negative correlation with dry eye symptom score and a positive correlation with the Schirmer test ( Figures 3 and 4 ; Table 2 ). In artificial eyes, tear meniscus height also correlated negatively with the dry eye symptom score ( Figure 3 , Table 2 ), but the Schirmer test score did not show a statistically significant correlation ( Figure 4 , Table 2 ).
| Variable | Schirmer Test Score a | Symptom Score b | ||
|---|---|---|---|---|
| r | P Value | r | P Value | |
| Normal eyes (n = 31) | ||||
| TM height | 0.496 | .005 c | −0.361 | .046 c |
| TM depth | 0.404 | .024 c | −0.475 | .007 c |
| TM area | 0.456 | .010 c | −0.429 | .016 c |
| TM volume | 0.462 | .009 c | −0.457 | .010 c |
| Artificial eyes (n = 31) | ||||
| TM height | 0.049 | .794 | −0.367 | .042 c |
| TM depth | −0.029 | .876 | −0.270 | .142 |
| TM area | −0.030 | .872 | −0.342 | .060 |
| TM volume | −0.003 | .988 | −0.334 | .067 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


