Purpose
To investigate the clinical outcome of a frontalis sling using preserved fascia lata in the treatment of vision-obscuring congenital ptosis in patients less than 2 years of age.
Design
Retrospective, interventional case series.
Methods
The study was conducted in an institutional setting and included 82 patients with visual axis–obscuring congenital ptosis. All patients underwent frontalis sling surgery with preserved fascia lata between November 1994 and December 2008, and had a minimum follow-up of 6 months. Visual and surgical outcomes were assessed by reviewing clinical photographs and medical charts. Surgical outcomes were defined as good, fair, or poor, based on the postoperative lid level.
Results
The mean age at surgery was 15.3 ± 4.8 months. After a mean follow-up of 54.8 ± 41.4 months, 64 patients (78.0%) showed good or fair surgical outcomes. Reoperation was performed in 16 of the patients with poor or fair results. Amblyopia was treated postoperatively in 75 of the 82 patients (91.5%) and had improved in 65 patients at the last follow-up. Postoperative entropion was identified in 5 cases, all of which were treated successfully. No other significant complications occurred.
Conclusions
For patients younger than 2 years of age, preserved fascia lata may be an appropriate substitute for autogenous fascia lata in frontalis sling surgery. Its long-term stability may enable a permanent effect in a certain proportion of patients, and may not require secondary surgery, which is common with synthetic materials.
Ptosis surgery is usually recommended, when appropriate, between 3 and 5 years of age, prior to entering school, to allow for the development of the eyelid structure, patient cooperation, and decreased anesthetic risks. However, the optimal timing of surgery remains controversial.
At a young age, in patients susceptible to amblyopia, earlier surgery may be considered to enable the functional development of binocular vision. The surgery could improve chin-up head posture and developmental problems related to severe congenital ptosis. However, early surgery presents a greater surgical risk associated with general anesthesia. In addition, visual function and levator muscle function are difficult to properly assess in young patients because of poor cooperation.
For patients with congenital ptosis younger than 2 years of age, special attention should be focused on the prevention of amblyopia. For severe ptosis in this age group, a frontalis sling is an appropriate corrective option.
Autogenous fascia lata is considered the best material for frontalis sling surgery. However, because of the difficulty in obtaining it, alternative materials are needed, especially for use in children below the age of 3 years. Although Mersilene mesh, e-polytetrafluoroethylene, polyfilament cable–type sutures (Supramid sutures), Prolene sutures, and silicone rods have been used, success rates and complications related to synthetic materials should be considered. Preserved fascia lata has been used for congenital ptosis of poor levator function. However, the efficacy and long-term outcome has not been established in patients less than 2 years of age.
We present a study of congenital ptosis correction using preserved fascia lata in patients with amblyopia under 2 years of age. To the best of our knowledge, this is the largest reported case series addressing this patient population. We investigated surgical and visual outcomes and evaluated the role of surgery at an early age for congenital ptosis.
Methods
Patient Characteristics and Assessments
This was an interventional case series study. A retrospective review was conducted in consecutive patients less than 2 years of age who had congenital ptosis with amblyopia. The patients underwent unilateral or bilateral frontalis sling surgery using preserved fascia lata between November 1, 1994 and December 31, 2008. The Samsung Medical Center Institutional Review Board approved the retrospective review of patient data. The study adhered to the tenets of the Declaration of Helsinki.
Surgical indications were unilateral or asymmetric bilateral ptosis severe enough to cover the center of the pupil in 1 eye and cause amblyopia. Surgery was delayed for patients without amblyopia. Patients who were followed for less than 6 months after surgery were excluded from the analysis.
Amblyopia was defined as a lack of fixation by the affected eye and objection to covering of the contralateral eye, or as a lack of fixation as assessed by the induced tropia test in the examined eye. During follow-up, cooperative patients were diagnosed with amblyopia when the difference of the best-corrected visual acuities (BCVA) between the 2 eyes was greater than 2 logMAR lines on the Snellen chart.
Preoperative and postoperative assessments included margin reflex distance-1 (MRD1), orthoptic evaluation, cycloplegic refraction, and 10-prism base-down tests. Postoperative complications were also described.
The surgical outcome was judged as good, fair, or poor based on the criteria described by Katowitz. A good result was defined as a postoperative lid level resting 2-3 mm below the superior corneal limbus without use of the frontalis muscle in bilateral cases, or within 1 mm of the opposite (normal) lid level in unilateral cases. A fair result was defined as a lid level in the same position as described above, but requiring the use of the frontalis muscle. A poor result was defined as a postoperative lid level 4 mm or more below the superior corneal limbus, even with maximal use of the frontalis muscle. Recurrence or failure was defined as a change in the surgical outcome from “good” or “fair” to “poor.”
Surgical Techniques
All surgeries were performed by 1 surgeon (Y.-D. Kim) using general anesthesia. Preserved fascia lata (Tutoplast; Tutogen Medical GmbH, Neunkirchen am Brand, Germany) was used in all patients, using a pentagonal configuration, as reported by Fox.
Two stab incisions were made 2 mm above the eyelid margin. Two additional stab incisions were made above the eyebrow, and a third forehead incision was centrally placed, 5 mm higher than the other incisions. The forehead incision was undermined 10 mm upward for sling material anchoring.
The preserved fascia lata was rehydrated prior to surgery, using gentamicin sulfate in saline. Using a Wright fascia needle, each end of the fascia strip was passed through the incisions and pulled up from the forehead incision until the eyelid margin was at the superior limbus. The overlapped fascia lata were sutured together using 6-0 black silk sutures. The ends of the fascia strips were cut short and buried beneath the frontalis muscle, and they were anchored superiorly to the frontalis muscle with 6-0 chromic gut sutures.
Statistical Analysis
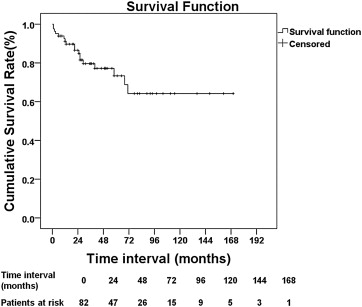
The time to recurrence of ptosis after surgery was calculated using the Kaplan-Meier survival analysis. The Wilcoxon signed rank test was used to compare the differences between preoperative and postoperative MRD1. The Fisher exact test was employed to analyze categorical data, including the unilateral and bilateral ptosis group comparisons. Statistical analysis was performed using SPSS software for Windows, version 18.0 (SPSS Inc, Chicago, Illinois, USA). Statistical significance was considered at P values <.05.
Results
Patient Characteristics
Eighty-two consecutive patients (59 male, 23 female) were included in the analysis. Two patients were excluded because of an insufficient follow-up during the study periods. Nineteen of these patients had bilateral surgery and 63 patients underwent unilateral surgery, representing a total of 101 eyelids. Bilateral surgery was performed only for the patients who had asymmetric bilateral ptosis with severe ptosis and amblyopia in 1 eye. The mean age of the patients at the time of surgery was 15.3 ± 4.8 months ( Table 1 ). The mean follow-up time was 54.8 ± 41.4 months, with a range of 6-170 months ( Table 2 ).
| Unilateral (n = 63 Patients) | Bilateral (n = 19 Patients) | Total (n = 82 Patients) | |
|---|---|---|---|
| Age at operation (m) | |||
| Mean ± SD | 15.0 ± 4.9 | 16.4 ± 4.4 | 15.3 ± 4.8 |
| Range | 6-24 | 6-22 | 6-24 |
| Sex, n (%) | |||
| Female | 19 (30.2%) | 4 (21.1%) | 23 (28.0%) |
| Male | 44 (69.8%) | 15 (78.9%) | 59 (72.0%) |
| Lid, n (%) | |||
| Right | 40 (63.5%) | 19 (100%) | 59 (58.4%) |
| Left | 23 (36.5%) | 19 (100%) | 42 (41.6%) |
| Unilateral | Bilateral | Total | |
|---|---|---|---|
| Surgical results (patients) | |||
| Good | 39 | 12 | 51 |
| Fair | 11 | 2 | 13 |
| Poor | 13 | 5 | 18 |
| Follow-up (mo, mean ± SD) | 52.5 ± 39.6 | 62.6 ± 46.5 | 54.8 ± 41.4 |
Amblyopia was identified exclusively in the ptotic eyes of patients with unilateral ptosis. In bilateral cases, amblyopia was identified in the eye with more severe ptosis. Associated ophthalmic findings included strabismus (8/82 cases), anisometropia (16/49 cases), a combination of strabismus and anisometropia (3 cases), epiblepharon (7 cases), Marcus-Gunn jaw winking syndrome (1 case), congenital nasolacrimal duct obstruction (1 case), and congenital lacrimal fistula (1 case).
Surgical Results
Fifty-one of the 82 cases (62.2%) showed good results and 13 (15.9%) showed fair results at the last follow-ups ( Figure 1 ). Hence, a satisfactory result was achieved in 64 of the 82 cases (78.0%) and a poor result was recorded in 18 cases (22.0%) ( Table 2 ). The success rates did not statistically differ between the unilateral and bilateral ptosis groups (50/63, 79.4%, vs 14/19, 73.7%, respectively, P = .600).

The mean ptosis recurrence time in the 18 failed cases was 27 ± 23 months from the first surgery; 12 of these patients underwent reoperation. Because 4 of the 13 patients with fair results chose to have surgical correction, 16 patients underwent reoperation (performed by 1 surgeon, Y.-D. Kim). The average age at reoperation was 56 ± 23 months, and the average time after the first surgery was 41 ± 22 months.
In performing follow-up surgeries, there were neither scar adhesions affecting the procedure nor any difficulties related to the sling material that was previously placed. Frontalis sling surgery was performed in 11 patients: 5 with autogenous fascia lata and 6 with preserved fascia lata, according to parental preferences. Maximal levator resection, with Whitnall’s sling surgery, was performed in 5 patients ( Table 3 ).
| Method of second surgery | |
| Frontalis sling with autogenous fascia lata | 5 patients |
| Frontalis sling with preserved fascia lata | 6 patients |
| Maximal levator resection with Whitnall’s sling surgery | 5 patients |
| Age at second surgery (mean ± SD) | 56 ± 23 mo |
| Time interval between the initial and second surgery (mean ± SD) | 41 ± 22 mo |
All but 1 patient retained good results after the second surgery and throughout the 90 months of the average follow-up period. The patient whose reoperation failed had undergone a frontalis sling procedure with preserved fascia lata 6 months after the first surgery. Ptosis recurred 30 months later; the patient underwent frontalis sling surgery with autogenous fascia lata 52 months after the second surgery.
Kaplan-Meier survival analysis was performed for the time from the initial surgery to recurrence over a 14-year period (170 months), and results suggested that recurrence started to occur as soon as 1 month after surgery. However, after a follow-up of 71 months, no recurrences were recorded ( Figure 2 ). The preoperative MRD1 of −0.94 ± 0.91 mm (range, −3.0 to +1.5 mm) increased to +1.86 ± 1.25 mm (range, −2.5 to +4.5 mm) postoperatively ( P < .0001, Figure 3 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


