Purpose
To report retinal findings for healthy newborn infants imaged with handheld spectral-domain optical coherence tomography (SD OCT).
Design
Prospective, observational case series.
Methods
Thirty-nine full-term newborn infants underwent dilated retinal examinations by indirect ophthalmoscopy and retinal imaging by handheld SD OCT, without sedation, at the Duke Birthing Center.
Results
Of the 39 infants imaged, 44% (17/39) were male. Race and ethnicity composition was 56% white, 38% black, 3% Asian, and 3% Hispanic. Median gestational age was 39 weeks (range, 36 to 41 weeks). Six (15%) of the 39 infants had bilateral subfoveal fluid on SD OCT not seen by indirect ophthalmoscopy. Eight infants (21%) had retinal hemorrhages noted on dilated retinal examination, 1 of which had subretinal fluid on SD OCT. Subretinal fluid was noted on follow-up examination to have resolved on SD OCT 1 to 4 months later. Infants with bilateral subretinal fluid had an older gestational age compared with infants without subretinal fluid (median, 40.4 vs 39.1 weeks, respectively; P = .03) and were more likely to have had mothers with diabetes (2/6 vs 0/33, respectively; P = .02). Vaginal versus Caesarian section delivery was not significantly different between the 2 groups.
Conclusions
Some healthy full-term infants have bilateral subfoveal fluid not obvious on dilated retinal examination. This fluid resolves within several months. The visual significance of this finding is unknown, but clinicians should be aware that it is common when evaluating newborn infants for retinal pathologic features using SD OCT.
Spectral-domain (SD) optical coherence tomography (OCT) provides reproducible retinal morphologic features and cross-sectional tissue measurements in vivo in a rapid, noninvasive, noncontact manner. Handheld OCT is well tolerated by children and infants and is more sensitive than clinical examination in detecting macular pathologic features.
OCT has been used to identify clinically important retinal pathologic features in premature infants, including retinoschisis, foveal hypoplasia, intraretinal cysts, preretinal neovascularization, and retinal detachment. Macular holes, hemorrhagic retinoschisis, vitreoretinal traction, and epiretinal membranes were identified in shaken baby syndrome using OCT, and in some cases influenced surgical management. Handheld SD OCT also was valuable in characterizing foveal hypoplasia in the eyes of infants with ocular and oculocutaneous albinism and in neonates with systemic diseases such as liver failure. Although handheld SD OCT may be performed during examination under anesthesia, anesthesia is not necessary to obtain useful images in infants and cooperative children.
Establishing a normative database of SD OCT findings in healthy full-term newborn infants is an important prerequisite for the proper diagnosis of retinal pathologic features using SD OCT in this population. We are not aware of any report on SD OCT imaging of healthy full-term neonates to date (PubMed Mesh search terms, optical coherence tomography AND infant ). In this study, a cohort of healthy full-term infants was examined by handheld SD OCT and indirect ophthalmoscopy shortly after birth.
Methods
Subjects
Thirty-nine healthy full-term infants were included in a prospective observational study. The study involved dilated retinal examination by indirect ophthalmoscopy and retinal imaging by handheld SD OCT, without sedation, at the Duke Birthing Center between August 2010 and October 2010. Infants’ and mothers’ medical records were reviewed for health history, delivery history, pregnancy history, gestational age of the infant at birth based on reconciliation of menstrual and ultrasound dating criteria, birthweight, and maternal age at the time of delivery. Infants were eligible for the study if they were born at 36 weeks’ gestation or later and did not have known systemic disease. If ocular abnormalities were identified in the original eye examination, parents were offered a repeat examination monthly until the findings resolved.
Procedures
All infants had both eyes dilated by instillation of 1 drop of Cyclomydril (phenylephrine hydrochloride 1% and cyclopentolate 0.2%; Alcon Laboratories, Fort Worth, Texas, USA), or cyclopentolate 0.5% and phenylephrine 2.5% were given to those infants with darkly pigmented irides. After pupillary dilation, a pediatric ophthalmologist (M.T.C. or S.F.F.) performed a clinical examination including indirect ophthalmoscopy with a 28-diopter lens and without an eyelid speculum.
A portable handheld SD OCT unit (Bioptigen, Inc, Research Triangle Park, North Carolina, USA) was used to image both eyes of all subjects after the age-customized method for SD OCT in infants described by Maldonado and associates, which allows imaging without sedation or a lid speculum. With this approach, multiple series of double-volumetric 800 A-scans × 80 B-scans centered on the optic nerve or fovea, measuring approximately 7 × 7 mm, were captured. Among the first 7 subjects, 2 infants were noted to have the unexpected finding of bilateral subretinal fluid at the foveal center. Because the clinician was aware of the SD OCT results, diagnosis using indirect ophthalmoscopy during the clinical examination of these 7 subjects was influenced by this knowledge. Starting with Patient 8, all infants were examined first with indirect ophthalmoscopy and then with SD OCT to mask the clinician from the SD OCT results. A study investigator later graded the images without knowledge of the indirect ophthalmoscopy results. The eyes of 14 infants were identified as having abnormal findings either by SD OCT or indirect ophthalmoscopy, and these subjects therefore were offered a repeat examination in the clinic approximately 1 month later, including repeat SD OCT imaging. Those infants with persistent pathologic features on either the dilated retinal examination or SD OCT were asked to return monthly until the abnormality resolved. Infants who were examined at 3 months of age or older underwent the preferential-looking test for an assessment of visual function, performed by an independent, masked, trained orthoptist, with age-matched normal ranges based on previous studies.
Image Processing
SD OCT images were converted into Digital Imaging and Communications in Medicine (DICOM) format and were graded qualitatively in OSIRIX medical imaging software (OSIRIX Foundation, Geneva, Switzerland) for the presence or absence of each retinal layer and for any pathologic abnormality present. Subretinal fluid was defined as an area of hyporeflectivity between the neurosensory retina and the retinal pigment epithelium. A cystoid space was defined as a distinctive area of hyporeflectivity within the neurosensory retina, extending in 3 dimensions and causing associated distortion of retinal layers. The highest quality scan containing the fovea, based on a subjective assessment of resolution and volume, was selected for quantitative analysis for each imaging session from each eye.
To quantify retinal features, the retinal layers were segmented semiautomatically on a single central scan using the MATLAB-based (Mathworks, Natick, Massachusetts, USA) software DOCTRAP version 10.2 (Duke University, Durham, North Carolina, USA). A custom MATLAB script was implemented on the segmentation output to acquire measurements for retinal thickness and dimensions of retinal pathologic features.
Statistical Analysis
Subjects with bilateral subretinal fluid on SD OCT were compared with subjects without subretinal fluid with respect to antenatal history (maternal diabetes and maternal age), birth outcomes (length of labor and method of delivery), postnatal characteristics (gestational age at birth calculated from reconciliation of menstrual and ultrasound dating criteria, birthweight, head circumference, Apgar scores, race, and sex), and other retinal parameters by SD OCT (presence of persistent inner retinal layers, total central foveal thickness, and foveal thickness of the neurosensory retina). Comparison of categorical variables was performed using the Fisher exact test, and comparison of continuous variables was performed using the Wilcoxon rank sum test. All statistics performed on ocular findings were adjusted for 2 eyes from each subject using a generalized estimating equations approach. All statistical analyses were performed with SAS software version 9.1.3 (SAS Institute, Inc, Cary, North Carolina, USA).
Results
Patient Demographic Characteristics
Of the 39 newborn infants recruited for the study, 17 (43.5%) were male, 22 (56.4%) were white, 15 (38.5%) were black, 1 (2.6%) was Asian, and 1 (2.6%) was Hispanic. One additional Asian male infant was recruited but later withdrawn by his parents before completion of the examination. The median gestational age of the infants was 39 weeks (range, 36 to 41 weeks). All infants were examined within the first 2 days of life. Five infants received follow-up examinations on time (4 infants at 1 month and 1 infant at both 1 and 2 months). An additional 2 infants did not return to the clinic at the requested 1-month follow-up, and instead came at later dates (1 infant at 2 months only and 1 infant at 4 months only; Table 1 ; Supplemental Table , available at AJO.com )
| Patient No. | Demographics | Systemic Findings | Delivery | Eye | Retinal Findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | PMA (wks) | Birth Weight (g) | Race | Maternal | Infant | Type & Events | Labor Length a | Clinical Examination Results | SD OCT | Follow-up of Abnormal Findings (mos) | ||
| 4 | M | 41 | 3825 | W | Gest DM | None | C/S | 11:00 | R | b | SRF | Less SRF (1), resolved SRF (2) |
| L | b | SRF | Less SRF (1), resolved SRF (2) | |||||||||
| 7 | F | 40 | 3635 | B | HTN, DM, obesity | None | C/S | 11:00 | R | b | SRF | Resolved SRF (4) |
| L | b | SRF | Resolved SRF (4) | |||||||||
| 11 | M | 40 | 3695 | W | None | None | V | 1:27 | R | Normal | SRF | Lost to follow-up |
| L | Normal | SRF | Lost to follow-up | |||||||||
| 15 | M | 41 | 3060 | W | AMA | None | V | 3:00 | R | Normal | SRF | Resolved SRF (1) |
| L | Normal | SRF | Resolved SRF (1) | |||||||||
| 17 | M | 40 | 3760 | W | None | None | V | 1:57 | R | RH | SRF | Lost to follow-up |
| L | RH | SRF | Lost to follow-up | |||||||||
| 22 | F | 39 | 3315 | W | AMA | None | V | 11:38 | R | Normal | SRF | Resolved SRF (2) |
| L | Normal | SRF | Resolved SRF (2) | |||||||||
a Time (in hours) from rupture of membranes to complete delivery.
b Early in the study, the examiner was not blinded to the SD OCT results during dilated retinal examinations. Therefore, assessment of the possible presence of subretinal fluid was not valid. In those cases, the retina appeared otherwise normal.
Subject Prenatal and Delivery History
Twenty-four of 39 infants (62%) were born by vaginal delivery without vacuum or forceps and 15 of 39 (38%) were born by Caesarean section (C-section). One of 39 infants (3%) was born after shoulder dystocia (Patient 12). Two of 39 infants (5%) were noted to have facial bruising (Patients 24 and 30), and another 2 of 39 infants (5%) were noted to have meconium on delivery (Patients 19 and 32). All infants were otherwise healthy ( Table 1 ; Supplemental Table , available at AJO.com ).
Retinal Findings by Indirect Ophthalmoscopy
Fifteen eyes (8/39 infants or 21%) had retinal hemorrhages noted on dilated retinal examination by standard indirect ophthalmoscopy. Hemorrhages were approximately one-quarter to one-half disk diameter and appeared intraretinal, discreet, and most dense in the temporal arcades; however, 2 extended to the macula (Patients 26 and 30). All 8 infants (100%) with retinal hemorrhages were born vaginally, compared with 39% (12/31) of infants without retinal hemorrhages ( P = .012). Only 1 of 15 infants (7%, Patient 17) with ocular retinal hemorrhages on clinical examination also had bilateral subretinal fluid on SD OCT ( Table 1 ; Supplemental Table , available at AJO.com ).
No infants with bilateral subretinal fluid noted on SD OCT had recognizable subretinal fluid or abnormal macular clinical findings on dilated ophthalmoscopic examination when the clinician was blinded to the imaging results. Four eyes of 3 additional infants had the equivocal appearance of foveal elevation based on lighter foveal pigmentation and abnormal contour on dilated ophthalmoscopic examination, without foveal abnormality seen on SD OCT ( Supplemental Table , available at AJO.com ).
Retinal Imaging at Birth by Spectral-Domain Optical Coherence Tomography
All 39 infants tolerated SD OCT imaging well, with adequate foveal images for the identification of subfoveal fluid obtained in all subjects. An additional infant was removed from the study because the parents became nervous during the SD OCT imaging and decided that they did not wish to proceed. That infant seemed comfortable during imaging, however. The median total central foveal thickness (including subretinal fluid, if present) for all 78 eyes (39 infants) was 85 μm (range, 55 to 303 μm). Six (15%) of the 39 infants had bilateral subfoveal fluid noted on SD OCT during the initial imaging session (without definitive subretinal fluid seen on clinical dilated retinal examination; Figure 1 ) . Subretinal fluid was hyporeflective and without intrafluid turbid or hyperreflective material. The overlying outer retina was hyperreflective. Among eyes with subretinal fluid at the initial SD OCT examination, the median height and width of subretinal fluid was 28 μm (range, 6 to 143 μm) and 651 μm (range, 421 to 1907 μm), respectively. The median total central foveal thickness (including subretinal fluid) was 109 μm (range, 62 to 303 μm) for eyes of infants with bilateral subretinal fluid versus 82.5 μm (range, 55 to 293 μm) for eyes of infants without bilateral subretinal fluid ( P = .056). Median thickness of the neurosensory retina (measured from the inner retinal border to the outermost edge of the photoreceptor outer segments) at the fovea was 102.5 μm (range, 88 to 160 μm) for eyes of infants with bilateral subretinal fluid, and this was significantly greater than that of those eyes without fluid (78 μm; range, 55 to 121 μm; P = .003).
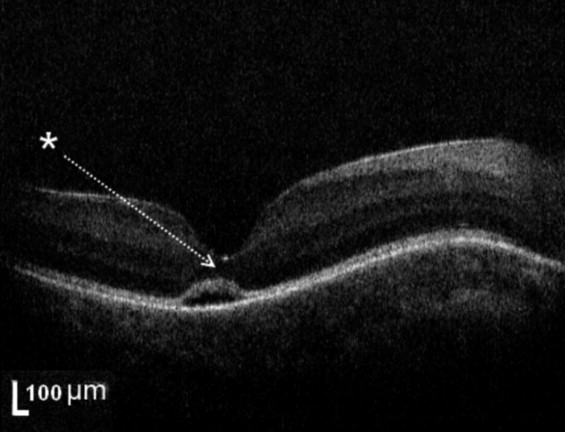
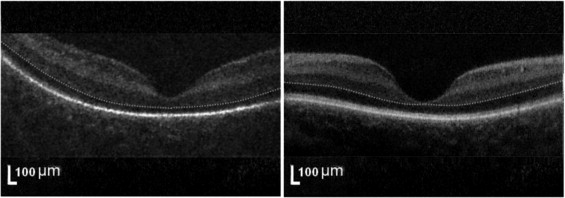
Seventy-two eyes (in 38/39 subjects or 97%) had SD OCT of sufficient quality for analysis of persistent inner retinal layers at the fovea at the initial examination. Among the 12 eyes (6 infants) with subretinal fluid detected on SD OCT, 11 (83%) of 12 eyes (5/6 infants) had SD OCT of sufficient quality for analysis of the inner retinal layers at the fovea. Of these, 7 (80%) of 11 eyes (4/5 infants) had persistent inner retinal layers at the fovea on SD OCT ( Figures 1 and 2 ) . Among the 66 eyes (33 infants) without subretinal fluid detected on SD OCT, 61 (97%) of 66 eyes (32/33 infants) had SD OCT of sufficient quality for analysis of inner retinal layers at the fovea. Of these, 34 (59%) of 61 eyes (19/32 infants) had persistent inner retinal layers at the fovea on SD OCT ( Figure 3 ) . The proportion of infants with at least 1 eye with persistent inner retinal layers did not differ significantly between the infants with and without bilateral subretinal fluid (80% vs 59%, respectively; P = .63).
In 1 of 39 cases (3%, Patient 20), 1 irregular intraretinal cystoid structure was noted parafoveally in each eye, measuring 450 μm in width at its widest diameter and 50 μm in height in the inner nuclear layer. This finding was not visualized by indirect ophthalmoscopy; the eyes of this infant demonstrated neither intraretinal hemorrhages on indirect ophthalmoscopy examination nor subretinal fluid on SD OCT imaging ( Supplemental Table , available at AJO.com ).
Associated Findings in Eyes of Infants With Subretinal Fluid
Four of the 6 infants (67%) with bilateral subretinal fluid were born vaginally, whereas the remaining 2 infants (33%) underwent the first stage of labor for 11 hours before a C-section for failure to progress. Both infants with bilateral subretinal fluid who underwent C-section (Patients 4 and 7) had a history of maternal prenatal diabetes (no infants without bilateral subretinal fluid had a prenatal history of maternal diabetes; P = .02). Infants with bilateral subretinal fluid had a significantly higher gestational age at birth (based on reconciliation of both menstrual and ultrasound dating criteria) compared with infants without subretinal fluid (median, 40.4 vs 39.1 weeks, respectively; P = .03). Otherwise, the 2 groups did not demonstrate statistically significant differences in sex or race distribution, head circumference, Apgar scores, method of delivery, birthweight, total length of labor, or maternal age ( Tables 1 and 2 ).
| Factors | Subretinal Fluid (n = 6) | No Subretinal Fluid (n = 33) | P Value |
|---|---|---|---|
| Gender | 4 (67%) male | 13 (39%) male | .37 |
| Race |
|
| .55 |
| 1 (17%) black | 14 (42%) black | ||
| 1 (3%) Asian | |||
| 1 (3%) Hispanic | |||
| Gestational age (weeks) | 40.4 (39.4 to 40.9) | 39.1 (36.1 to 41.6) | .03 a |
| Birthweight (g) | 3665 (3060 to 3825) | 3305 (2125 to 3920) | .06 |
| Head circumference (cm) | 34.7 (0.61) | 34.11 (1.32) | .39 |
| Apgar score at 1 min | 9 (7 to 9) | 9 (4 to 9) | .84 |
| Apgar score at 5 mins | 9 (8 to 9) | 9 (8 to 9) | .38 |
| Type of delivery | 4 (67%) vaginal | 19 (58%) vaginal | 1.00 |
| 2 (33%) Caesarian section | 14 (42%) Caesarian section | ||
| Total length of labor (hours) | 7.0 (1.5 to 11.6) | 1.9 (0 to 26.5) | .13 |
| Maternal diabetes | 2 (33%) | 0 (0%) | .02 a |
| Maternal age (years) | 30 (25 to 40) | 29 (18 to 41) | .40 |
a P < .05. Continuous variables are presented as mean (± standard deviation) for normally distributed variables and median (minimum to maximum) for others.
Retinal Examination of Infants With Bilateral Subretinal Fluid at Follow-Up by Spectral-Domain Optical Coherence Tomography and Indirect Ophthalmoscopy
Three infants with bilateral subretinal fluid underwent a follow up retinal examination and SD OCT 1 month later. At that time, 2 infants (Patients 15 and 22) were found to have normal-appearing foveas in both eyes, whereas 1 infant (Patient 4) was found to have persistent but diminished subretinal fluid in both eyes compared with the result of the initial examination (fluid height decreased from 140 to 71 μm in the right eye and from 143 to 55 μm in the left eye; fluid width decreased from 1839 to 544 μm in the right eye and from 1907 to 621 μm in the left eye). Although the subretinal fluid had resolved completely in both eyes of this infant on additional SD OCT imaging at 2 months of age, the appearance of the inner segment/outer segment photoreceptor junction was not entirely normal compared with other scans of similarly aged infants without subretinal fluid ( Figure 2 ). A fourth infant (Patient 7) with bilateral subretinal fluid on SD OCT at birth did not return for a follow-up examination until 4 months of age, at which point both eyes showed normal-appearing foveas by SD OCT and retinal examination; the eyes were aligned and vision was normal by the preferential-looking test (binocular vision, 4.7 cycles/degree, normal for age; Table 1 ).
Results
Patient Demographic Characteristics
Of the 39 newborn infants recruited for the study, 17 (43.5%) were male, 22 (56.4%) were white, 15 (38.5%) were black, 1 (2.6%) was Asian, and 1 (2.6%) was Hispanic. One additional Asian male infant was recruited but later withdrawn by his parents before completion of the examination. The median gestational age of the infants was 39 weeks (range, 36 to 41 weeks). All infants were examined within the first 2 days of life. Five infants received follow-up examinations on time (4 infants at 1 month and 1 infant at both 1 and 2 months). An additional 2 infants did not return to the clinic at the requested 1-month follow-up, and instead came at later dates (1 infant at 2 months only and 1 infant at 4 months only; Table 1 ; Supplemental Table , available at AJO.com )
| Patient No. | Demographics | Systemic Findings | Delivery | Eye | Retinal Findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | PMA (wks) | Birth Weight (g) | Race | Maternal | Infant | Type & Events | Labor Length a | Clinical Examination Results | SD OCT | Follow-up of Abnormal Findings (mos) | ||
| 4 | M | 41 | 3825 | W | Gest DM | None | C/S | 11:00 | R | b | SRF | Less SRF (1), resolved SRF (2) |
| L | b | SRF | Less SRF (1), resolved SRF (2) | |||||||||
| 7 | F | 40 | 3635 | B | HTN, DM, obesity | None | C/S | 11:00 | R | b | SRF | Resolved SRF (4) |
| L | b | SRF | Resolved SRF (4) | |||||||||
| 11 | M | 40 | 3695 | W | None | None | V | 1:27 | R | Normal | SRF | Lost to follow-up |
| L | Normal | SRF | Lost to follow-up | |||||||||
| 15 | M | 41 | 3060 | W | AMA | None | V | 3:00 | R | Normal | SRF | Resolved SRF (1) |
| L | Normal | SRF | Resolved SRF (1) | |||||||||
| 17 | M | 40 | 3760 | W | None | None | V | 1:57 | R | RH | SRF | Lost to follow-up |
| L | RH | SRF | Lost to follow-up | |||||||||
| 22 | F | 39 | 3315 | W | AMA | None | V | 11:38 | R | Normal | SRF | Resolved SRF (2) |
| L | Normal | SRF | Resolved SRF (2) | |||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


