Purpose
To report the morphologic changes of the subfoveal choroidal thickness using spectral-domain optical coherence tomography following segmental scleral buckling.
Design
Retrospective, observational case series.
Methods
The study included 21 eyes of 20 patients who underwent segmental scleral buckling for the treatment of rhegmatogenous retinal detachment. All patients underwent the measurements of the subfoveal choroidal thickness preoperatively and 1 week, 1 month, and 3 months after the surgery. The changes in choroidal thickness, 4 mm from the fovea, before and 1 week after surgery were analyzed in the buckled and unbuckled side.
Results
The preoperative mean subfoveal choroidal thickness of operated eyes was 239.2 ± 91.0 μm. The postoperative mean subfoveal choroidal thicknesses of operated eyes at 1 week, 1 month, and 3 months were 267.6 ± 96.8 μm, 250.6 ± 95.8 μm, and 239.4 ± 95.6 μm, respectively. There were significant differences between preoperative subfoveal choroidal thickness and 1-week-postoperative and 1-month-postoperative subfoveal choroidal thicknesses ( P < .01, P = .03, ANOVA), and there was no significant difference between subfoveal choroidal thicknesses preoperatively and 3 months postoperatively ( P > .99, ANOVA). The changes in choroidal thickness of the buckled and unbuckled side preoperatively and 1 week postoperatively were not significantly different (n = 8, P = .589, 2-way ANOVA).
Conclusion
The subfoveal choroidal thickness may change temporarily following segmental scleral buckling surgery. This may be the result of reversible subclinical microcirculatory dysfunction of the choroid.
Scleral buckling is a well-established surgical treatment for rhegmatogenous retinal detachment (RRD). Despite the high anatomic success rate and simplicity of this procedure, postoperative complications, some of which are rare, do occur, such as refractive changes, infection, intrusion and extrusion of the buckling element, strabismus, glaucoma, macular edema and submacular fluid, subretinal fluid, anterior and posterior segment ischemia, choroidal detachment, and chorioretinal blood flow alterations. However, little is known about the effect of the scleral buckling procedure on morphologic changes of the subfoveal choroid because it is difficult to image even with optical coherence tomography (OCT). Enhanced depth imaging (EDI) is a simple technique first introduced by Spaide. Cross-sectional choroidal images are obtained using a commercially available OCT device by simply pushing the device close enough to the eye. This technique has furthered our knowledge of chorioretinal diseases such as central serous chorioretinopathy, polypoidal choroidal vasculopathy, and age-related macular degeneration. Changes in choroidal thickness have been reported in these diseases.
The aim of this study is to report the morphologic changes of the subfoveal choroid using EDI-OCT techniques following scleral buckling.
Patients and Methods
Patient medical records of 23 eyes of 22 consecutive patients with RRD repaired by segmental scleral buckling from January 1, 2011, to October 31, 2011, were retrospectively reviewed. Patients with previous ocular surgery histories other than cataract surgery or preexisting ocular diseases were excluded from this study. Patients with low-quality or blurred OCT images in which the chorioscleral interface could not be traced were also excluded.
All patients underwent a comprehensive ophthalmic examination at the preoperative and postoperative visits including measurement of best-corrected visual acuity (BCVA), measurement of intraocular pressure (IOP) by noncontact tonometry, axial length measurement (OA-1000; Tomey Corporation, Nagoya, Japan), slit-lamp examination, and fundus examination. Surgeries were performed by 4 of the coauthors (A.N., H.Y., T.O., and T.H.). Retinal breaks were identified in all patients and were treated by transscleral cryotherapy. Mattress sutures were placed 8.0 to 8.5 mm apart with 5-0 polyester (Mani, Tochigi, Japan) for the segmental buckle and a silicone sponge (Mira No. 506; Mira, Inc, Waltham, Massachusetts, USA) was sutured as an explant in all cases. Neither scleral dissection nor extraocular muscle disinsertion was required for any patient. Subretinal fluid drainage was performed if necessary. Dexamethasone (MSD K.K., Tokyo, Japan) was injected subconjunctivally at the end of surgery. Betamethasone 0.1% (Shionogi & Co Ltd., Osaka, Japan), moxifloxacin 0.5%, and bromfenac 0.1% were topically instilled postoperatively. Atropine (Santen Pharmaceutical Co Ltd, Osaka, Japan) was used at the surgeon’s discretion.
OCT scans were performed by a single examiner (M.K.), who is experienced at performing scans using the spectral-domain OCT device (Spectralis; Heidelberg Engineering, Heidelberg, Germany). Each session was performed at approximately 12 PM to avoid diurnal variations. Two high-quality, 10.5-mm horizontal and vertical line scans through the fovea were obtained for each eye. The line scans were saved for analysis after 100 frames were averaged using the automatic averaging and eye tracking features of the proprietary device. Fundus features were registered and tracked automatically to align follow-up scans with preoperative scans.
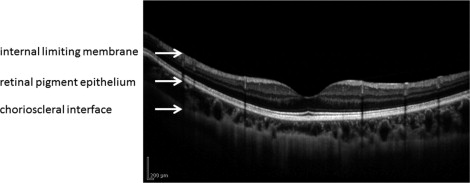
The retina was defined as the layer between the hyperreflective line corresponding to the internal limiting membrane and the outer part of the hyperreflective line corresponding to the base of the retinal pigment epithelium (RPE). The choroid was defined as the layer between the base of the RPE and the hyperreflective line or margin corresponding to the chorioscleral interface ( Figure 1 ). Because choroidal thickness is reported to vary significantly with location, axial length, refractive error, and age, we compared the preoperative and postoperative subfoveal choroidal thickness in the operated eye. Subfoveal choroidal thicknesses were measured using manual calipers provided with the software of the proprietary device. Each subfoveal choroidal thickness from the horizontal and vertical line scans was measured by 3 of the coauthors (M.K., A.N., and H.Y.), who were masked to the other test results, and values were averaged. The subfoveal choroidal thicknesses of 12 fellow eyes without any previous ocular surgery history served as controls. The asymmetry of choroidal thickness in vertical OCT scans was also assessed in cases of buckling within either the superior or inferior half. The choroidal thicknesses 4 mm superior and inferior from the fovea were measured.
Statistical analyses were performed using SPSS version 18.0 (SPSS Inc, Chicago, Illinois, USA). Analysis of variance (ANOVA) was used for the data obtained by sequential measurements. A value of P < .05 was considered statistically significant. In order to explore the clinical factors significantly associated with relative change in subfoveal choroidal thickness 1 week after surgery (Δ subfoveal choroidal thickness [%]), various factors such as age, sex, preoperative axial length, change in IOP at 1 week, preoperative refractive error, preoperative extent of retinal detachment, numbers of retinal holes/tears, the extent of quadrant-wise buckle, and preoperative macular status were assessed using linear regression analysis, the Mann-Whitney U test, and 1-way ANOVA. The changes in choroidal thickness, 4 mm from the fovea, before and 1 week after surgery were analyzed on the buckled and unbuckled side using 2-way ANOVA. Visual acuity (VA) was measured with a Japanese standard decimal visual chart and converted into logarithm of the minimal angle of resolution (logMAR) units for statistical analysis. Inter-rater reliability was analyzed for the measurements performed by 3 of the coauthors (M.K., A.N., and H.Y.) using intraclass correlation coefficients. The coefficient of repeatability (1.96 × standard deviation of differences between pairs of measurements in the same eye during the same OCT sessions) was calculated for the measurements of 1 of the coauthors (A.N.) according to the methods outlined by Bland and Altman. Coefficient of repeatability, expressed as a percentage of the mean measurement, was also calculated (this was equal to 1.96 × coefficient of variation).
Results
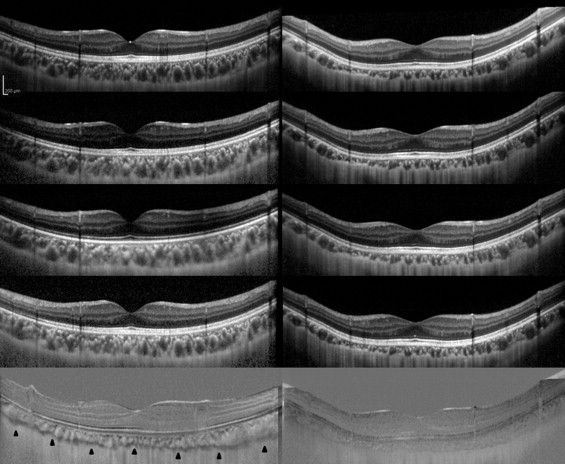
A total of 21 eyes of 20 patients were included in the present study. The excluded cases were 1 patient with a previous buckling surgery and 1 patient with low-quality, immeasurable OCT images. The demographic and clinical characteristics of the patients are shown in Table 1 . There were no cases of scleral buckling straddling extraocular vortex veins. Representative preoperative and postoperative OCT images of the operated eye and the fellow eye are shown in Figure 2 .
| Age (years) | 40.0 ± 20.1 (16–71) |
| Male sex (%) | 57.1 |
| Preoperative BCVA (logMAR) | 0.089 ± 0.18 (0–0.80) |
| IOP (mm Hg) | 14.2 ± 3.2 (8.1–19.5) |
| Refractive error (diopter) | −5.6 ± 3.8 (−11.5 to +1.875) |
| Axial length (mm) | 25.6 ± 1.5 (23.11–27.34) |
| Pseudophakic lens status (%) | 4.8 |
| Preoperative macula status; macula off (%) | 33.3 |
| Extent of retinal detachment (%) | |
| 1 quadrant | 61.9 |
| 2 quadrants | 23.8 |
| 3 quadrants | 14.3 |
| 4 quadrants | 0 |
| No. of retinal holes/tears (%) | |
| 1 | 85.7 |
| 2 | 14.3 |
| Location(s) of retinal holes/tears (%) | |
| Superior half | 72.7 |
| Inferior half | 27.3 |
| Superior | 18.2 |
| Nasal superior | 18.2 |
| Nasal | 0 |
| Nasal inferior | 4.5 |
| Inferior | 9.1 |
| Temporal inferior | 18.2 |
| Temporal | 4.5 |
| Temporal superior | 27.3 |
a All data are represented by mean ± standard deviation (range), except those representing percent (%).
Comparisons of preoperative and postoperative clinical factors are shown in Table 2 . The preoperative mean subfoveal choroidal thickness of operated eyes was 239.2 ± 91.0 μm (range: 110.2–414.5 μm). The postoperative mean subfoveal choroidal thicknesses at 1 week, 1 month, and 3 months were 267.6 ± 96.8 μm (range: 110.2–443.2 μm), 250.6 ± 95.8 μm (range: 16.0–425.8 μm), and 239.4 ± 95.6 μm (range: 102.3–437.0 μm), respectively. There were statistically significant differences between preoperative subfoveal choroidal thickness and those at 1 week and 1 month postoperatively ( P < .01, P = .045, 1-way repeated ANOVA), but there was no significant difference between subfoveal choroidal thicknesses preoperatively and 3 months postoperatively ( P > .99, 1-way repeated ANOVA).
| Time | Subfoveal Choroidal Thickness of Operated Eye (μm) | Subfoveal Choroidal Thickness of Fellow Eye (μm) | IOP (mm Hg) | BCVA (logMAR) |
|---|---|---|---|---|
| Before surgery | 239.2 ± 91.0 | 221.7 ± 81.8 | 14.2 ± 3.2 | 0.089 ± 0.18 |
| After surgery | ||||
| 1 week | 267.6 ± 96.8 (<.01) | 224.6 ± 81.6 (.45) | 12.7 ± 2.8 (.12) | — |
| 1 month | 250.6 ± 95.8 (.045) | 220.0 ± 81.0 ( P > .99) | 11.8 ± 2.7 (<.01) | 0.048 ± 0.084 (.58) |
| 3 month | 239.4 ± 95.6 ( P > .99) | 219.3 ± 80.8 (.88) | 12.4 ± 2.6 (.031) | 0.018 ± 0.032 (.079) |
a All data are represented by mean ± standard deviation. P values calculated by repeated ANOVA are given in parentheses for comparisons before and after surgery.
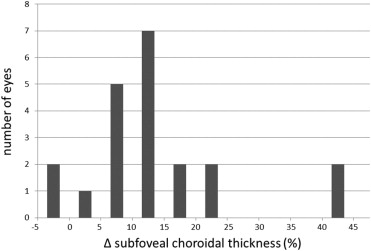
Distribution of Δ subfoveal choroidal thickness (%) at 1 week is shown in Figure 3 . No clinical factors were significantly associated with Δ subfoveal choroidal thickness (%) by linear regression analysis, the Mann-Whitney U test, or 1-way ANOVA ( Table 3 ). The changes in choroidal thickness of the buckled and unbuckled side before and 1 week after surgery were not significantly different (n = 8, P = .589, 2-way ANOVA, Table 4 ).
| Adjusted R 2 Value, P Value | ||
|---|---|---|
| Relative change in subfoveal choroidal thickness (%) (mean ± SD) a | 112.9 ± 12.5 | — |
| Age (y) (mean ± SD) | 40.0 ± 20.1 | R 2 = 0.023, P = .240 b |
| Sex, male/female | 12/9 | P = .120 c |
| Preoperative axial length (mm) (mean ± SD) | 25.6 ± 1.5 | R 2 = −0.016, P = .418 b |
| Change in IOP (mm Hg) (mean ± SD) a | −1.5 ± 2.8 | R 2 = 0.037, P = .200 b |
| Preoperative refractive error (diopter) (mean ± SD) | −5.6 ± 3.8 | R 2 = −0.010, P = .384 b |
| Preoperative extent of retinal detachment (quadrants) | 1.5 ± 0.75 | P = .759 d |
| Preoperative number(s) of retinal hole/tear | 1.1 ± 0.36 | P = .270 d |
| Extent of quadrant-wise buckle (degrees) (mean ± SD) | 107 ± 38.8 | R 2 = 0.141, P = .053 b |
| Preoperative macula status, on / off | 14/7 | P = .815 c |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


