The mainstay of frontal sinus surgery for chronic rhinosinusitis is to achieve and maintain an adequate frontal outflow tract. Using a stepwise approach and identifying critical endoscopic anatomic landmarks, to minimize complications and obtain long-term good endoscopic surgical results, should achieve this. The goal is to relieve the patient’s symptoms, restore functional mucociliary flow, achieve a wide frontal sinus ostium and prevent long-term scarring and stenosis. Meticulous dissection and appropriate use of instrumentation and techniques aids in preventing unnecessary damage to normal mucosa while achieving one’s goal of an adequate surgical ostium.
Key points
- •
Successful frontal sinus surgery relies on a complete frontal sinus surgery, and surgeons should approach management in a stepwise fashion from least invasive to advanced procedures depending on the case in hand and underlying pathophysiology.
- •
When performing a Draf III (EMLP), all intersinus septations need to be removed and a wide cavity created to facilitate postoperative medical therapy and improve symptoms.
- •
Maintaining dissection anterior to the coronal plane of the posterior frontal sinus wall prevents skull base injury.
- •
Before frontal sinus surgery, a complete anterior ethmoidectomy with identification of the fovea ethmoidalis and skeletonization of the medial orbital wall is necessary.
- •
Postoperative debridements and appropriate topical medical therapy are crucial in maintaining patency of the frontal drainage pathway.
Video content accompanies this article at http://www.oto.theclinics.com .
Introduction
Frontal sinus surgery has always been considered a challenge. This is mainly attributed to its wide array of variable and complex anatomy, extent of disease, and associated scarring and osteoneogenesis that can ensue, either due to the primary disease process or previous incomplete surgery. It is crucial to highlight that the mainstay of frontal sinus surgery for chronic rhinosinusitis, as it is with any of the sinuses, is to achieve and maintain an adequate frontal outflow tract (frontal recess and infundibulum) while preserving minimally diseased mucosal membranes where possible. This has to be achieved by using a stepwise approach, identifying critical endoscopic anatomic landmarks, to minimize complications and obtain long-term good endoscopic surgical results.
In this article, we present the various endoscopic operative techniques and approaches to frontal sinus surgery in a systematized manner. We discuss the pertinence of useful anatomic landmarks to achieve safe frontal sinus surgery.
Introduction
Frontal sinus surgery has always been considered a challenge. This is mainly attributed to its wide array of variable and complex anatomy, extent of disease, and associated scarring and osteoneogenesis that can ensue, either due to the primary disease process or previous incomplete surgery. It is crucial to highlight that the mainstay of frontal sinus surgery for chronic rhinosinusitis, as it is with any of the sinuses, is to achieve and maintain an adequate frontal outflow tract (frontal recess and infundibulum) while preserving minimally diseased mucosal membranes where possible. This has to be achieved by using a stepwise approach, identifying critical endoscopic anatomic landmarks, to minimize complications and obtain long-term good endoscopic surgical results.
In this article, we present the various endoscopic operative techniques and approaches to frontal sinus surgery in a systematized manner. We discuss the pertinence of useful anatomic landmarks to achieve safe frontal sinus surgery.
Treatment goals and outcomes
The most common causes of surgical failure are polyp recurrence, stenosis, and consequent scarring and/or osteoneogenesis. This can be attributed, in part, to inadequate surgery, failure to recognize contributing anatomic barriers, and/or surgeon inexperience.
The goal is to relieve the patient’s symptoms, restore functional mucociliary flow, achieve a wide frontal sinus ostium, and prevent long-term scarring and stenosis.
Multiple factors contribute to failure, and selecting the appropriate procedure for patients represents a challenge.
Mucociliary Flow
Messerklinger first described frontal sinus ciliary flow. Knowledge of the ciliary flow pattern aids in successful frontal recess surgery. The cilia sweep up mucus along the interfrontal septum, laterally across the roof, medially along the floor toward the natural ostium. Mucosal preservation is fundamental when conceivable, although there are select situations in which this is impossible. Meticulous dissection and appropriate use of instrumentation and techniques aids in preventing unnecessary damage to normal mucosa while achieving one’s goal of an adequate surgical ostium.
Osteoneogenesis
Controversies exist regarding the management of new bone formation in the region of the frontal sinus ostium. Some investigators advocate minimally invasive surgery with placement of stents and administration of oral and topical steroids in the postoperative period to prevent restenosis. The objective should be removal of the new bone to achieve a wide and adequate anteroposterior (AP) and lateral diameter, culture-directed postoperative antibiotics, office debridement, and close follow-up so as to intervene early in the event of symptomatic restenosis or closure of the frontal outflow tract. It is therefore very important to have proper visualization and instrumentation in the office setting to maximize the chances of a successful outcome.
Preoperative planning
Before working in the region of the frontal sinus, it is imperative to have a robust conceptualization of the radiological anatomy and be conscious of the different anatomic relationships in this complex anatomic area. Being unfamiliar with the intricate anatomy of the inverted funnel, like frontal recess, predisposes to incomplete dissection and consequent failure with restenosis.
The challenging location of the frontal sinus prompts anxiety for the surgeon because of the risk of injury to the anterior ethmoid artery, anterior cribriform plate, olfactory apparatus, and anterior skull base. Familiarizing oneself with a mental picture of the complex anatomy of the frontal recess and its surrounding cells gives the surgeon confidence in performing a safe surgery.
Once a decision for surgery has been made, a critical review of the axial, coronal, and sagittal cuts of the computed tomography (CT) scan must be performed.
Anatomy of the Frontal Recess
The frontal drainage outflow tract is bordered anteriorly by the posterior wall of the agger nasi or frontal infundibular cells, posteriorly by suprabullar air cells, laterally by the orbital roof, and medially by the vertical lamella of the middle turbinate ( Fig. 1 ). The fovea ethmoidalis (ethmoid roof) forms the roof of the frontal recess. This is important to acknowledge, as it has been reported that the right fovea ethmoidalis slopes higher than the left in 59% of patients. Regardless of the asymmetries that may exist, it is more important to recognize this sloping for the potential of inadvertent penetration in the most medial aspect of the fovea ethmoidalis, particularly close to the insertion of the vertical lamella of the middle or superior turbinates, in the area corresponding to the lateral lamella of the cribriform plate. The depth of the olfactory fossa according to Keros (type I: <3 mm, type II: 3–7 mm, type III: >7 mm) needs to be noted preoperatively and care should be taken when aggressively dissecting the medial fovea ethmoidalis, especially in patients with deeper olfactory fossae (type III Keros). It is crucial to keep in mind that variable degrees of pneumatization may exist between patients, and from one side to the other. In addition, aplastic or hypoplastic frontal sinus cavities may be present.
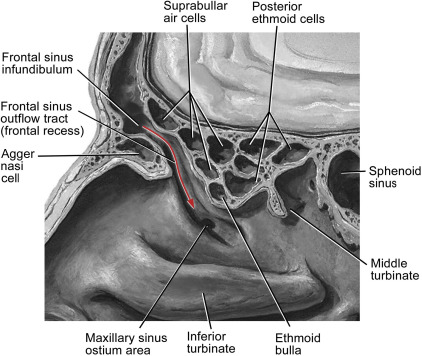
Anatomic variants and cellular configurations along the frontal sinus outflow tract can contribute to obstruction and consequent disease. Having a clear understanding of the cells of the frontal sinus outflow tract leads to an appropriate initial approach to the frontal sinus.
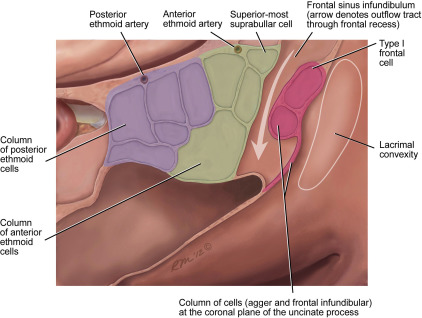
Agger Nasi
The agger nasi cell is the most anterior ethmoid air cell. It is located in the lateral nasal wall, anterior to the middle turbinate. It is found in 93% of the population and is best evaluated on coronal views. It aids in understanding the transition from frontal recess to frontal sinus on coronal cuts of the preoperative CT scan. The superolateral attachment of the uncinate inserts into the inferior wall of the agger nasi cell. It also identifies the coronal plane leading superiorly to the frontal infundibular cells and frontal infundibulum ( Fig. 2 ).
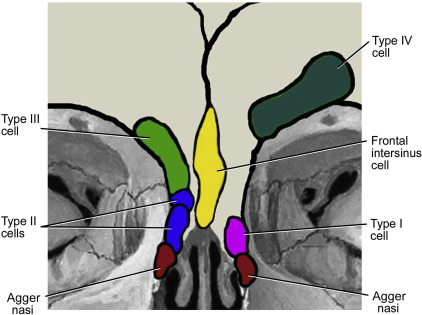
Intersinus Septal Cell
The intersinus septal cell represents pneumatization of the frontal sinus septum. It contributes to obstruction of the frontal recess and compromises the frontal ostium from a medial to lateral direction. This cell needs to be addressed in frontal sinus surgery to ensure adequate lateral dimensions of the frontal sinus ostium to prevent subsequent closure or stenosis.
Frontal Ethmoidal Cells
The frontal infundibular cells border the frontal drainage outflow tract anteriorly approximately in the same coronal plane as the uncinate and agger nasi cell. These cells were previously described by Bent and Kuhn into 4 types: type 1 (1 cell above the agger nasi), type II (2 or more cells above the agger nasi, but below the level of the frontal infundibulum and orbital roof), type III (at least 1 cell extending supraorbitally), and type IV (independent cell within the frontal sinus and not in contiguity with the other cells). They can be seen anywhere from 25% to 40% of the population and are located superior to the agger nasi cell. The surgeon needs to be aware of the sequence of cells that are opened to ensure a wide and clear frontal recess without the crushing of these cells of the persistent of obstructive inflammatory disease of the frontal outflow tract. These cells are best evaluated on coronal and sagittal cuts ( Fig. 3 ).
Suprabullar Cell
The frontal outflow tract is bordered posteriorly by the suprabullar cells, best viewed on sagittal cuts. These cells lie above the ethmoid bulla and pneumatize up to its attachment to the skull base. These cells may be variable in size and number, and do not enter the frontal sinus proper, unless the very last superior suprabullar cell pneumatizes superiorly, and extends into the frontal sinus (frontal bulla cell).
Frontal Bulla Cells
Frontal bulla cells are also best seen on sagittal views. They arise from the most superoanterior suprabullar cells. These cells pneumatize toward the frontal infundibulum along the skull base and posterior wall of the frontal sinus.
The goal is to achieve a mental 3-dimensional reconstruction of the drainage pathway and associated cells so as to formulate an appropriate surgical plan. These cells vary among patients but their careful and methodical dissection is crucial to ensure a successful surgery.
Frontal Sinus Ostium
The frontal sinus ostium or infundibulum represents the narrowest point of the frontal sinus complex. The anteroposterior diameter of the frontal ostium needs to be assessed preoperatively. Patients who have a wide AP diameter will usually have an easier dissection and better postoperative prognosis. This is best assessed on sagittal cuts. Special care should be paid to patients with a narrow AP diameter, particularly in terms of mucosal preservation to prevent postoperative scarring and stenosis. This is particularly important in patients with no osteoneogenesis, where more advanced procedures may be needed, and mucosal sparing may not be possible. The goal is to achieve a wide AP diameter that can prevent consequent stenosis and scarring. In addition, evaluating the AP diameter preoperatively aids in reflecting the need for a drill out (Draf IIb or III) or more advanced procedures.
The surgeon should always gauge the degree of difficulty and keep in mind the possibility of extended procedures.
Indications for frontal sinusotomy
The most common indication for endoscopic frontal sinusotomy is chronic frontal sinusitis refractory to maximal medical management. This could be attributed to nasal polyposis, mucoceles, mechanical obstruction, osteoneogenesis, severe acute frontal sinusitis, benign and malignant neoplasms, and frontal sinus fractures, among others.
The aim is to achieve functional mucus clearance with removal of all frontal recess cells and prevent future restenosis and scarring.
Patient positioning
Before starting any endoscopic sinus surgery, proper patient positioning should be ensured. The patient should be placed in a supine position on the operating table with the table tilted to 30° anti-Trendelenburg to prevent venous congestion and allow more adequate control of hemostasis intraoperatively. The head should be in a neutral position to allow the surgeon to work in a plane parallel to the skull base and prevent inadvertent injury. The surgeon typically stands on the right side of the patient. The video tower and associated imaging devices are positioned at the head of the table facing the surgeon.
Both eyes need to be protected with a clear adhesive dressing, to be able to detect acute proptosis or chemosis, consistent with an orbital injury or hematoma. The eyes should be periodically palpated during the superior ethmoidectomy and frontal sinusotomy. The forehead, eyes, nose, and upper lip need to be exposed.
We advocate the use of a 30-degree, 45-degree, and/or 70-degree scope in frontal sinus surgery. The endoscopes and instruments should never cross. Using angled scopes facilitates easier passage of instruments and better visualization.
It is important to operate in a comfortable setting.
Key landmarks
The key to safe frontal sinus surgery is accurate knowledge of anatomy. We advocate the use of several key anatomic landmarks to warrant safe endoscopic frontal sinus surgery.
Key landmarks described by Dr Casiano in 2001 include the following :
- •
Uncinate process superior attachment
- •
Middle turbinate vertical lamella
- •
Vertical line from the maxillary natural ostium area, parallel to the nasolacrimal apparatus convexity
- •
Anterior ethmoid artery
- •
The suprabullar and agger nasi cells
- •
Frontal sinus posterior wall.
Identifying the frontal sinus outflow tract is the initial and most fundamental step in frontal sinus surgery. Before addressing the frontal recess, an ethmoidectomy should be achieved to allow for safe frontal sinus surgery with a clear identification of the fovea ethmoidalis.
Skeletonization of the medial orbital wall (lamina papyracea) needs to be achieved to ensure adequate dissection and exposure of the frontal sinus.
The frontal recess should be addressed in a posterior to anterior and a medial to lateral direction to avoid skull base penetration, particularly at the level of the lateral lamella of the cribriform plate. It can be initially identified approximately 5 to 10 mm behind the anterior attachment of the middle turbinate. We advocate using the ball probe initially to prevent inadvertent skull base injury. The correct point of entry will be superomedially, adjacent to the vertical lamella of the middle turbinate, and posterior to the coronal plane of the superior attachment of the uncinate process, or anterior to the coronal plane of the face of the ethmoid bulla if intact. The tip of the probe should be directed superolaterally, without exerting pressure (2-finger palpation), and toward the direction of the orbital roof and parallel to the sloping fovea ethmoidalis.
The location of the anterior ethmoid artery always should be kept in mind. It is located an average of 20 mm from the anterior attachment of the middle turbinate or 10 mm from the posterior wall of the frontal sinus. All septations should be displaced anteroinferiorly at the level of the anterior ethmoid artery to avoid inadvertent injury. If there is to be aggressive manipulation in the area, it is best to perform this medially, so as to minimize orbital retraction of the artery if severed close to the orbital wall near the entry into its canal.
We recommend using the 70-degree telescope especially when internal frontal sinus manipulation is indicated.
The posterior wall of the frontal sinus serves as a guide during surgery to avoid intracranial penetration and injury at the level of the cribriform plate. This will be discussed later in this article.
We also advocate the use of the frontal probe, giraffe forceps, and an angled microdebrider to remove the frontal recess cell septations, while preserving normal mucosa circumferentially at the level of the infundibulum. Small septations should be carefully removed with overlying mucosa, without stripping of infundibular mucosa, or crushing of septations and mucosal elements, obliterating the frontal outflow tract.
Care should be taken with using the microdebrider and it entails surgeon experience. It should be used only to clean up loose mucosal edges and not for meticulous dissection in narrow passages. The opening of the angled microdebrider should initially be pointed anteriorly, until the posterior wall of the frontal and anterior ethmoid artery has been identified. The tip should always be kept moving, and never kept in a stationary location, to minimize inadvertent bone and mucosal removal, and orbital or skull base penetration. It also never should be pointed toward the orbit, until the orbit has been clearly identified.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


