Purpose
To evaluate the spectrum of retinal diseases that can demonstrate paracentral acute middle maculopathy and isolated ischemia of the intermediate and deep capillary plexus.
Design
Retrospective, multicenter, observational case series.
Methods
This is a retrospective case series review of 9 patients (10 eyes) from 5 centers with paracentral acute middle maculopathy lesions and previously unreported retinal vascular etiologies. Case presentations and multimodal imaging, including color photographs, near-infrared reflectance, fluorescein angiography, spectral-domain optical coherence tomography (SD OCT), and orbital color Doppler imaging, are described. Baseline and follow-up findings are correlated with clinical presentation, demographics, and systemic associations.
Results
Five men and 4 women, aged 27–66 years, were included. Isolated band-like hyperreflective lesions in the middle retinal layers, otherwise known as paracentral acute middle maculopathy, were observed in all patients at baseline presentation. Follow-up SD OCT analysis of these paracentral acute middle maculopathy lesions demonstrated subsequent thinning of the inner nuclear layer. Novel retinal vascular associations leading to retinal vasculopathy and paracentral acute middle maculopathy include eye compression injury causing global ocular ischemia, sickle cell crisis, Purtscher’s retinopathy, inflammatory occlusive retinal vasculitis, post-H1N1 vaccine, hypertensive retinopathy, migraine disorder, and post–upper respiratory infection.
Conclusion
Paracentral acute middle maculopathy lesions may develop in a wide spectrum of retinal vascular diseases. They are best identified with SD OCT analysis and may represent ischemia of the intermediate and deep capillary plexus. These lesions typically result in permanent thinning of the inner nuclear layer and are critical to identify in order to determine the cause of unexplained vision loss.
The retinal capillary system in the central macula is a layered vascular structure composed of the superficial and deep capillary plexus. The latter consists of an intermediate and deep plexus along the inner and outer aspect of the inner nuclear layer, respectively. The superficial capillary plexus is visible with fluorescein angiography and ischemia of this structure may manifest as a cotton-wool spot. However, fluorescein angiography fails to adequately visualize the intermediate and deep plexuses. Before the advent of spectral-domain optical coherence tomography (SD OCT), abnormalities in these deeper plexuses, located in the middle retina, were not readily appreciated.
Recently the term “paracentral acute middle maculopathy” has been added to our vernacular and refers to the presence of a hyperreflective parafoveal band at the level of the inner nuclear layer on SD OCT that co-localizes precisely with the intermediate and deep capillary plexuses. The subsequent development of inner nuclear layer thinning corresponding to the original paracentral acute middle maculopathy lesion indicates that the primary etiology may be ischemia of the intermediate and deep capillary systems.
Paracentral acute middle maculopathy has recently been associated with various retinal vascular diseases, including nonproliferative diabetic retinopathy, central retinal vein occlusion, and retinal artery occlusion, further supporting the possible underlying ischemic nature of this SD OCT finding. This series will present an additional 9 cases of paracentral acute middle maculopathy associated with various disorders not listed above, including ocular compression causing global ischemia, sickle cell retinopathy, retinal vasculitis, Purtscher’s retinopathy, and other etiologies.
Methods
Institutional review board approvals for retrospective chart reviews were obtained commensurate with the respective institutional requirements prior to the beginning of the study. The research adhered to the tenets of the Declaration of Helsinki and was conducted in accord with regulations set forth by the Health Insurance Portability and Accountability Act. This was a multicenter, retrospective, observational case series review of the clinical and multimodal imaging findings for 10 eyes (9 patients) with paracentral acute middle maculopathy. The diagnostic criteria for paracentral acute middle maculopathy included band-like hyperreflectivity on SD OCT in the middle macula centered on the inner nuclear layer that evolved into thinning of that retinal layer. Multimodal imaging included color fundus photographs (Carl Zeiss Meditec, Dublin, California, USA; Topcon Medical Systems, Oakland, New Jersey, USA), near-infrared reflectance (SPECTRALIS; Heidelberg Engineering, Heidelberg, Germany), fluorescein angiography (Carl Zeiss Meditec; Topcon Medical Systems), SD OCT (SPECTRALIS; Heidelberg Engineering), and orbital color Doppler imaging (Logiq 700; General Electric Medical Systems, Milwaukee, Wisconsin, USA). Detailed clinical evaluation was performed and associated systemic etiologies were identified. Baseline and follow-up SD OCT findings were correlated with the clinical presentation, demographics, systemic associations, and baseline and final visual acuities, as well as adjunctive imaging findings.
Results
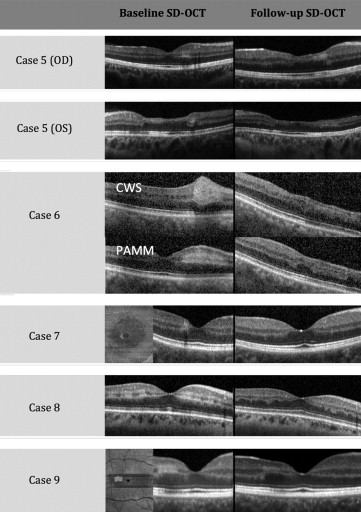
Ten eyes with paracentral acute middle maculopathy in 9 patients (5 men and 4 women) were identified and collected for this study. Patient ages ranged from 27 to 66 years (mean 39 years). Hyperreflectivity on SD OCT in the middle retinal layers was observed for all patients in the acute presentation, followed by thinning of the inner nuclear layer with follow-up SD OCT analysis. All patients presented with a form of retinal vascular disease. Four cases are described in detail below, and 5 other cases are summarized in the Table and Figure 1 , with the baseline and follow-up SD OCT images included.
| Case No. | Age/Sex | Presentation | Systemic Disease | Eye Disease | Eye | Baseline BCVA | Baseline Fundus | Follow-up BCVA |
|---|---|---|---|---|---|---|---|---|
| 5 | 27/F | 2–3 months of vision loss OS and “changing vision” OD. In-clinic BP was 180/80 | Migraines, OCP, Adderall use, HTN | Hypertensive retinopathy | OD | 20/20 | Nasal parafoveal, wedge-shaped, yellowish white lesion | 20/20 |
| OS | CF | Superonasal, parafoveal, wedge-shaped, yellowish white lesion | CF | |||||
| 6 | 50/M | Acute-onset blurry vision OD. Recent BP ranged from 112/71 to 195/88 depending on medication compliance | HTN, CHF, pulmonary hypertension, alcohol abuse | Hypertensive retinopathy, pseudophakia | OD | 20/30 | Nasal parafoveal wedge-shaped yellowish lesion (localizes to PAMM) with an adjacent, more superficial-appearing white lesion (localizes to a CWS) | 20/40 |
| 7 | 28/M | Acute-onset paracentral scotoma OD | Migraine with visual aura | _ | OD | 20/20 | Normal dilated exam | 20/20 |
| 8 | 53/F | Acute onset of paracentral scotomas OD 2–3 days after H1N1 vaccine | Hypothyroidism, HTN, anxiety | Pseudophakia | OD | 20/50 | Scattered parafoveal whitening (localizes with PAMM), peripapillary CWSs | 20/50 |
| 9 | 37/M | Acute onset of scotoma OD 2 weeks after a URI | Recent URI | _ | OD | 20/25 | Temporal parafoveal wedge-shaped light-yellow lesion | 20/20 |
Case 1
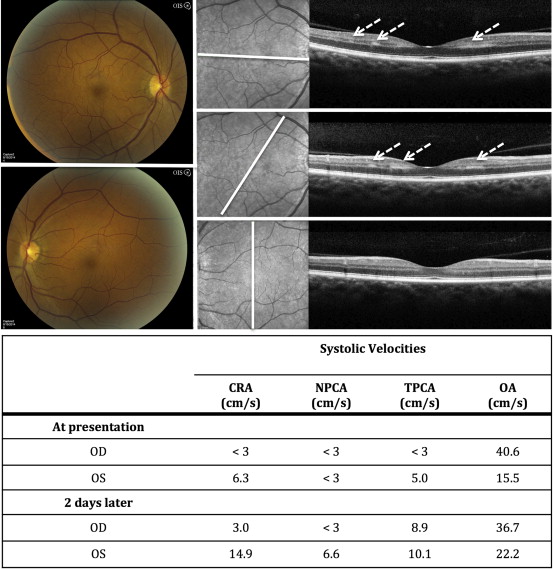
A 61-year-old African-American man with a history of hypertension, hyperlipidemia, diabetes mellitus, and obstructive sleep apnea presented with an acute onset of multiple paracentral scotomas in the right eye after falling asleep overnight with his head on top of his hands. Review of systems was otherwise negative. Visual acuity was 20/25 in the right eye and 20/20 in the left. Anterior segment and dilated examinations were unremarkable. Orbital color Doppler imaging showed an absence of flow in the right central retinal artery, right nasal and temporal short posterior ciliary artery, and left nasal short posterior ciliary artery. Flow in the right ophthalmic artery was normal. Erythrocyte sedimentation rate, C-reactive protein, and platelets were all within normal limits. He was started immediately on high-dose steroids because of the concern for giant cell arteritis. A subsequent stroke evaluation showed <50% bilateral carotid stenosis and an incidental 2.2 mm right internal carotid artery aneurysm. Subsequent bilateral temporal artery biopsies returned negative for giant cell arteritis and steroid tapering was initiated. Repeat orbital color Doppler imaging 2 days after the initial presentation showed improved flow rates and velocities in the right central retinal artery and right temporal short posterior ciliary artery. An absence of flow persisted in the short nasal posterior ciliary artery bilaterally. At the 2-week follow-up interval, the paracentral scotomas persisted, with vision remaining 20/25 bilaterally. Fluorescein angiography showed bilateral global delayed perfusion. Bilateral near-infrared reflectance imaging showed multiple parafoveal dark-gray lesions, and SD OCT through these lesions revealed multiple paracentral acute middle maculopathy lesions ( Figure 2 ).
Case 2
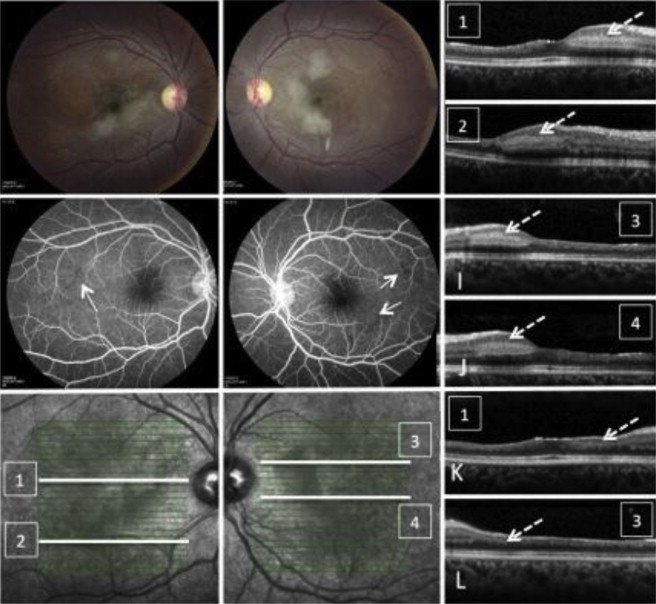
A 28-year-old African-American woman with sickle cell disease presented with bilateral paracentral scotomas in the absence of other signs of occlusive crisis (eg, bone pain, chest pain, abdominal pain). Visual acuity at presentation was 20/50 in her right eye and 20/200 in her left eye. Macular examination showed a wedge of deep retinal whitening nasal to each fovea without any other stigmata of sickle cell retinopathy, such as retinal hemorrhages, iridescent spots, pigment clumps, or peripheral neovascularization. Fluorescein angiography showed bilateral capillary pruning and temporal retinal vascular nonperfusion. SD OCT showed hyperreflective bands at the level of the inner nuclear layer corresponding to the white macular lesions, consistent with paracentral acute middle maculopathy, and inner retinal atrophy of the temporal macula typical of old branch retinal artery occlusions ( Figure 3 ).
Case 3
A 36-year-old Brazilian woman presented with a central scotoma of her right eye and floaters in the left eye for 1 week. She had a prior history of flu-like illness with gastrointestinal symptoms and right-sided retro-orbital pain. Medical history was remarkable for a pregnancy-induced deep vein thrombosis. Visual acuity was 20/150 in the right eye and 20/25 in the left eye. Anterior examination was normal. Dilated retinal examination showed papillitis, occlusive vasculitis, and multifocal retinal infiltrates in each eye and inferotemporal retinal ischemia in the right eye, all of which was confirmed with fluorescein angiography. SD OCT through the zone of inferotemporal ischemia showed paracentral acute middle maculopathy temporal to the fovea and both superficial and deep capillary ischemia nasal to the fovea. The patient was started on prednisone 60 mg daily. Vision later improved to 20/25 in the right eye ( Figure 4 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


